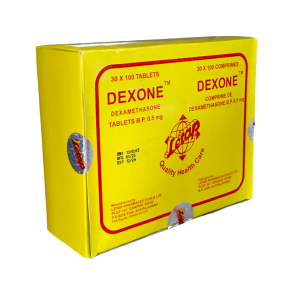
Dexamethasone is a potent glucocorticoid medication widely used for its anti-inflammatory and immunosuppressive properties. Dexamethasone was first synthesized in 1957. It is indicated for a variety of conditions, including rheumatic disorders, severe allergies, asthma, skin diseases, and certain types of cancer.
What is Dexamethasone?
Dexamethasone is a synthetic corticosteroid that mimics the effects of hormones produced by the adrenal glands. It works by decreasing inflammation and suppressing the immune response. It is a white to practically white, odorless, crystalline powder, stable in air and practically insoluble in water.
Indications
Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment in asthma, contact dermatitis, atopic dermatitis, perennial or seasonal allergic rhinitis, drug hypersensitivity reactions, and serum sickness.
The drug is designed to treat such dermatologic diseases as bullous dermatitis herpetiformis, mycosis fungoides, exfoliative erythroderma, pemphigus, and severe erythema multiforme (Stevens-Johnson syndrome).
Dexamethasone is used to treat such endocrine disorders as primary or secondary adrenocortical insufficiency, hypercalcemia associated with cancer, congenital adrenal hyperplasia, and nonsuppurative thyroiditis.
It may help with some gastrointestinal and ophthalmic diseases.
Dexamethasone may be indicated in hematologic disorders, like acquired (autoimmune) hemolytic anemia, idiopathic thrombocytopenic purpura in adults, congenital (erythroid) hypoplastic anemia (Diamond-Blackfan anemia), pure red cell aplasia, and selected cases of secondary thrombocytopenia.
In some cases, the medicine may be indicated for the palliative management of leukemias and lymphomas.
Acute exacerbations of multiple sclerosis, craniotomy, cerebral edema associated with a primary or metastatic brain tumor, or head injury can also be treated with Dexamethasone.
To induce a diuresis or remission of proteinuria in idiopathic nephrotic syndrome or due to lupus erythematosus, Dexamethasone can be indicated.
Respiratory diseases like berylliosis, fulminating or disseminated pulmonary tuberculosis, when used concurrently with appropriate antituberculous chemotherapy, idiopathic eosinophilic pneumonia, and symptomatic sarcoidosis are indications for this medicine.
It may help with some rheumatic disorders as adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in acute gouty arthritis, ankylosing spondylitis, acute rheumatic carditis, rheumatoid arthritis, psoriatic arthritis, juvenile rheumatoid arthritis (selected cases may require low-dose maintenance therapy), for the treatment of dermatomyositis, polymyositis, and systemic lupus erythematosus.
Clinical Pharmacology
Glucocorticoids, synthetic and naturally occurring, are adrenocortical steroids readily absorbed from the gastrointestinal tract. Glucocorticoids cause varied metabolic effects. Moreover, they modify the body’s immune responses to diverse stimuli.
It is approximately 25 times more potent than hydrocortisone (cortisol). It has minimal mineralocorticoid activity, which reduces the risk of fluid retention and other side effects associated with mineralocorticoid receptor activation. The drug’s pharmacokinetics indicate a long half-life, allowing for once-daily dosing in many cases.
Ingredients
The active ingredient is Dexamethasone, while inactive ingredients may vary depending on the specific formulation and manufacturer.
It is available in various formulations, including oral tablets, oral solutions, injectable forms, and topical applications.
What Are the Dosages of Dexamethasone?
The dosage of Dexamethasone varies based on the condition being treated, patient response, and specific formulation used. Common dosages include:
- Oral tablets: 0.5 mg to 20 mg.
- Oral liquid: 0.5 mg/5 mL.
- Injectable solutions: Varies based on clinical need.
Your physician will determine the appropriate dosage regimen tailored to individual patient needs.
Important Safety Information
Dexamethasone should be used with caution in patients with a history of infections, diabetes, high blood pressure, or mental health disorders. Long-term use can lead to significant side effects, including osteoporosis, adrenal suppression, and increased susceptibility to infections.
Rare instances of anaphylactoid reactions have occurred in patients receiving corticosteroid therapy.
Average and large doses of corticosteroids can cause elevation of blood pressure, sodium and water retention, and increased potassium excretion. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary.
If the patient is receiving steroids already, the dosage may have to be adjusted. Metabolic clearance of corticosteroids is decreased in hypothyroid patients and increased in hyperthyroid patients. Changes in the patient’s thyroid status may necessitate a dosage adjustment.
Therapy with corticosteroids should be used with great caution in patients after a recent myocardial infarction.
Patients on corticosteroids are more susceptible to infections than healthy individuals. These infections may be mild to severe. Infection with any pathogen (viral, bacterial, fungal, protozoan, or helminthic) in any body location may be associated with using corticosteroids alone or in combination with other immunosuppressive agents. With increasing doses of corticosteroids, the rate of occurrence of infectious complications increases. Be aware that corticosteroids may also mask some signs of current infection.
Corticosteroids may exacerbate systemic fungal infections and, therefore, should not be used in the presence of such infections unless they are needed to control life-threatening drug reactions. There have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac diseases.
Latent disease may be activated, or intercurrent infections may exacerbate due to pathogens, including those caused by Amoeba, Candida, Cryptococcus, Mycobacterium, Nocardia, Pneumocystis, and Toxoplasma. It is recommended that latent amebiasis or active amebiasis be ruled out before initiating corticosteroid therapy in any patient who has spent time in the tropics or with unexplained diarrhea. Corticosteroids should also be used with great care in patients with known or suspected threadworm infestation. The medicine should not be used in cerebral malaria.
The use of corticosteroids in active tuberculosis should be restricted to those cases of fulminating or disseminated tuberculosis in which the corticosteroid is used to manage the disease in conjunction with an appropriate antituberculous regimen. Close observation is necessary if corticosteroids are indicated in patients with latent tuberculosis or tuberculin reactivity.
Administration of live vaccines is contraindicated in patients receiving immunosuppressive doses of corticosteroids. Killed or inactivated vaccines may be administered. However, the response to such vaccines cannot be predicted.
Chickenpox and measles can have a more severe or even fatal course in pediatric and adult patients on corticosteroids. In pediatric and adult patients who have not had these diseases, particular care should be taken to avoid exposure.
Patients should be warned not to discontinue the use of corticosteroids abruptly or without medical supervision. As prolonged use may cause adrenal insufficiency and make patients dependent on corticosteroids, they should advise any medical attendants that they are taking corticosteroids. They should seek medical advice immediately should they develop an acute illness, including fever or other signs of infection. Symptoms of corticosteroid withdrawal include myalgia, arthralgia, and malaise. Persons on corticosteroids should be warned to avoid exposure to chickenpox or measles.
Pregnancy and Breast-feeding
The medicine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Infants born to mothers who have received substantial doses of corticosteroids during pregnancy should be carefully observed for signs of hypoadrenalism.
Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. A decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
The efficacy and safety of corticosteroids in children are based on the well-established course of effect of corticosteroids, which is similar in pediatric and adult populations. Published studies provide evidence of efficacy and safety in pediatric patients for the treatment of nephrotic syndrome in patients older than 2 years of age and aggressive lymphomas and leukemias in patients older than 1 month of age. Other indications for pediatric use of corticosteroids, e.g., severe asthma and wheezing, are based on adequate and well-controlled trials conducted in adults on the premise that the course of the diseases and their pathophysiology are considered substantially similar in both populations. The adverse effects of corticosteroids in pediatric patients are similar to those in adults. To minimize the potential growth effects of corticosteroids, pediatric patients should be titrated to the lowest effective dose.
Geriatric Use
Clinical studies did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and concomitant disease or other drug therapy. In particular, the increased risk of diabetes mellitus, fluid retention, and hypertension in elderly patients treated with corticosteroids should be considered.
Prescription
Dexamethasone is available by prescription only. Contact your physician to get a prescription.
Patients should closely follow their healthcare provider’s prescriptions regarding dosage and duration of treatment to minimize risks associated with corticosteroid therapy.
Contraindications to Dexamethasone
Dexamethasone should not be used in patients with:
- fungal infections;
- known hypersensitivity to Dexamethasone or any component of the formulation;
- certain viral infections (e.g., herpes simplex keratitis).
Side Effects
Side effects can include:
- Allergic reactions: anaphylaxis, anaphylactoid reaction, angioedema.
- Endocrine: development of cushingoid state, decreased carbohydrate and glucose tolerance, glycosuria, hyperglycemia, hypertrichosis, hirsutism, manifestations of latent diabetes mellitus, increased requirements for insulin or oral hypoglycemic agents in diabetes, secondary adrenocortical and pituitary unresponsiveness (particularly in times of stress, as in trauma, surgery, or illness), menstrual irregularities, suppression of growth in pediatric patients.
- Dermatologic: allergic dermatitis, acne, ecchymoses and petechiae, dry scaly skin, erythema, increased sweating, impaired wound healing, striae, rash, suppression of reactions to skin tests, thinning scalp hair, thin fragile skin, urticaria.
- Metabolic: negative nitrogen balance due to protein catabolism.
- Cardiovascular: cardiac arrest, bradycardia, cardiac arrhythmias, circulatory collapse, cardiac enlargement, fat embolism, congestive heart failure, hypertrophic cardiomyopathy in premature infants, hypertension, myocardial rupture following recent myocardial infarction, edema, syncope, tachycardia, pulmonary edema, thrombophlebitis, thromboembolism, vasculitis.
- Gastrointestinal: elevation in serum liver enzyme levels (usually reversible upon discontinuation), abdominal distention, hepatomegaly, nausea, peptic ulcer with possible perforation and hemorrhage, pancreatitis, perforation of the small and large intestine (particularly in patients with inflammatory bowel disease), ulcerative esophagitis.
- Fluid and electrolyte disturbances: fluid retention, congestive heart failure in susceptible patients, potassium loss, hypokalemic alkalosis, sodium retention.
- Musculoskeletal: loss of muscle mass, aseptic necrosis of femoral and humeral heads, muscle weakness, pathologic fracture of long bones, osteoporosis, steroid myopathy, vertebral compression fractures, tendon rupture.
- Ophthalmic: glaucoma, exophthalmos, posterior subcapsular cataracts, increased intraocular pressure.
- Neurological/Psychiatric: depression, convulsions, euphoria, headache, emotional instability, increased intracranial pressure with papilledema (pseudotumor cerebri) usually following discontinuation of treatment, mood swings, insomnia, neuropathy, neuritis, paresthesia, psychic disorders, personality changes, vertigo.
- Other: decreased resistance to infection, abnormal fat deposits, increased or decreased motility and number of spermatozoa, hiccups, moon face, malaise, weight gain.
Patients should report any severe or persistent side effects to their healthcare provider.
Interactions of Dexamethasone with Other Medicines
Dexamethasone can interact with various medications:
- Cholestyramine: It may increase the clearance of corticosteroids.
- Aminoglutethimide: it may diminish adrenal suppression by corticosteroids.
- Dexamethasone suppression test (DST): false-negative results in the dexamethasone suppression test (DST) in patients treated with indomethacin have been reported.
- Amphotericin B injection and potassium-depleting agents: patients should be observed closely for the development of hypokalemia. Moreover, there have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure.
- Digitalis glycosides: patients on digitalis glycosides may be at increased risk of arrhythmias due to hypokalemia.
- Antibiotics: macrolide antibiotics have been reported to cause a significant decrease in corticosteroid clearance.
- Ephedrine: It may enhance the metabolic clearance of corticosteroids, resulting in decreased blood levels and lessened physiologic activity, thus requiring an increase in corticosteroid dosage.
- Anticholinesterases: concomitant use of anticholinesterase agents and corticosteroids may produce severe weakness in patients with myasthenia gravis.
- Estrogens, including oral contraceptives: these drugs may decrease the hepatic metabolism of certain corticosteroids, thereby increasing their effect.
- Oral anticoagulants: co-administration of corticosteroids and warfarin usually results in inhibition of response to warfarin. However, there have been some conflicting reports.
- Hepatic Enzyme Inducers, Inhibitors, and Substrates: these medicines may enhance the corticosteroid metabolism and require the corticosteroid dosage to be increased.
- Antidiabetics: because corticosteroids may increase blood glucose concentrations, dosage adjustments of antidiabetic agents may be required.
- Ketoconazole: Ketoconazole has been reported to decrease the metabolism of certain corticosteroids by up to 60%, leading to an increased risk of corticosteroid side effects. Moreover, this drug alone can inhibit adrenal corticosteroid synthesis and may cause adrenal insufficiency during corticosteroid withdrawal.
- Antitubercular drugs: serum concentrations of isoniazid may be decreased.
- Nonsteroidal anti-inflammatory agents (NSAIDs): concomitant use of aspirin (or other nonsteroidal anti-inflammatory agents) and corticosteroids increases the risk of gastrointestinal side effects.
- Cyclosporine: increased activity of both cyclosporine and corticosteroids may occur when the two are used concurrently. Convulsions have been reported with this concurrent use.
- Vaccines: patients on corticosteroid therapy may exhibit a diminished response to toxoids and live or inactivated vaccines due to inhibiting antibody response.
- Skin tests: corticosteroids may suppress reactions to skin tests.
- Phenytoin: in post-marketing experience, there have been reports of both increases and decreases in phenytoin levels with dexamethasone co-administration, leading to alterations in seizure control.
- Thalidomide: co-administration with thalidomide should be employed cautiously, as toxic epidermal necrolysis has been reported with concomitant use.
Overdose of Dexamethasone
While an overdose of Dexamethasone is not typically life-threatening, it can lead to severe side effects such as hypertension, gastrointestinal bleeding, or psychiatric symptoms. In case of suspected overdose, seek immediate medical attention.
Storage
Dexamethasone should be stored at room temperature, away from moisture and heat. Keep children out of reach and dispose of any unused medication properly.
Benefits of Using Dexamethasone
|
Benefit |
Description |
|
Anti-inflammatory Effects |
Dexamethasone effectively reduces inflammation and alleviates symptoms such as swelling, redness, and pain associated with inflammatory disorders. It is beneficial for treating conditions like arthritis, asthma, and skin diseases. It |
|
Immunosuppressive Action |
It suppresses the immune system’s response, which is useful in managing autoimmune diseases like lupus and rheumatoid arthritis. This helps prevent the body from attacking its tissues. |
|
Management of Allergic Reactions |
Dexamethasone effectively treats severe allergic reactions and conditions like anaphylaxis by reducing the immune response and mitigating symptoms such as swelling and hives. |
|
Nausea and Vomiting Prevention |
It prevents nausea and vomiting in chemotherapy or surgery patients, enhancing comfort and recovery during treatment. |
|
Treatment of Croup in Children |
Dexamethasone is commonly indicated for croup in children, where a single dose can significantly reduce airway swelling, improving breathing and comfort. |
|
Support in Cancer Treatment |
It is used as part of treatment regimens for certain cancers, helping to manage symptoms and side effects associated with cancer therapies, such as nausea and inflammation. |
|
Improvement of Preterm Labor Outcomes |
Dexamethasone can improve neonatal outcomes when administered to mothers at risk of preterm labor, aiding in lung development of the fetus. |
|
High-Altitude Illness Treatment |
It effectively treats high-altitude cerebral edema (HACE) and high-altitude pulmonary edema (HAPE), making it a crucial medication for climbers experiencing altitude sickness. |
|
Versatile Administration Routes |
Dexamethasone can be administered via various routes (oral, intravenous, intramuscular), allowing flexibility based on patient needs and circumstances. |
Dexamethasone Brand Names in Different Countries
Dexamethasone is marketed under various brand names globally. Some examples include:
|
Country |
Brand Names |
|
United States |
Decadron, DexPak |
|
United Kingdom |
Dexadreson |
|
Canada |
Dexamethasone Injection |
|
India |
Dexasone, Dexamine, Decmax |
|
Bangladesh |
Decason, Demax, Dexam |
|
Australia |
Dexamethasone (various formulations) |
|
South Africa |
Dexa-Inject, Dexamethasone |
|
New Zealand |
Dexamethasone (various formulations) |
|
Pakistan |
Dexon, Dexamet |
|
Philippines |
Dexa, Dexamethasone |
|
Germany |
Dexamethason (various formulations) |
|
France |
Dexaméthasone |
|
Brazil |
Dexametason |
Check the additional information about this drug here. The information is provided by the Food and Drug Administration (FDA).