Definition
The spectrum of sexually transmitted diseases includes the classic venereal diseases – gonorrhea, syphilis, chancroid, lymphogranuloma venereum, and granuloma inguinale – as well as a variety of other pathogens known to be spread by sexual contact (Table Sexually Transmitted Diseases). Common clinical syndromes associated with sexually transmitted diseases are listed in Table Selected Syndromes Associated with Common Sexually Transmitted Pathogens. The most current information on epidemiology, diagnosis, and treatment of sexually transmitted diseases provided by the Centers for Disease Control and Prevention can be found at http://www.cdc.gov.
| TABLE. Sexually Transmitted Diseases | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| TABLE. Selected Syndromes Associated with Common Sexually Transmitted Pathogens | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| TABLE. Presentation of Gonorrhea Infections | ||||||||||||||||||
|
Gonorrhea
Syphilis
Chlamydia
Genital herpes
Trichomoniasis
- Trichomoniasis is caused by Trichomonas vaginalis, a flagellated, motile protozoan that is responsible for 3 to 5 million cases per year in the United States.
- Coinfection with other sexually transmitted diseases (such as gonorrhea) is common in patients diagnosed with trichmoniasis.
Clinical presentation
The typical presentation of trichomoniasis in males and females is presented in Table Presentation of Trichomonas Infections.
| TABLE. Treatment of Genital Herpes | ||||||||||||||||||||||||
|
||||||||||||||||||||||||
Diagnosis
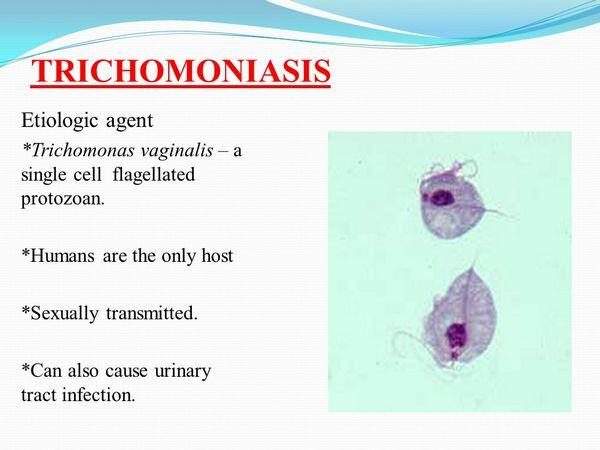
- T. vaginalis produces nonspecific symptoms also consistent with bacterial vaginosis, and thus laboratory diagnosis is required.
- The simplest and most reliable means of diagnosis is a wet-mount examination of the vaginal discharge. Trichomoniasis is confirmed if characteristic pear-shaped, flagellating organisms are observed. Newer diagnostic tests such as monoclonal antibody or DNA probe techniques, as well as Polymerase chain reaction tests are highly sensitive and specific.
| TABLE. Presentation of Trichomonas Infections | |||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||
| TABLE. Treatment of Trichomoniasis | |||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||
| TABLE. Treatment Regimens for Miscellaneous Sexually Transmitted Diseases | ||||||||||||||||||||||
|
||||||||||||||||||||||
Treatment
- Metronidazole is the only antimicrobial agent available in the United States that is consistently effective in T. vaginalis infections.
- Gastrointestinal complaints (e.g., anorexia, nausea, vomiting, diarrhea) are the most common adverse effects, with the single 2-g dose of metronidazole, occurring in 5% to 10% of treated patients. Some patients complain of a bitter metallic taste in the mouth.
- Patients intolerant of the single 2-g dose because of gastrointestinal adverse effects usually tolerate the multidose regimen.
- To achieve maximal cure rates and prevent relapse with the single 2-g dose of metronidazole, simultaneous treatment of infected sexual partners is necessary.
- Patients who fail to respond to an initial course usually respond to a second course of metronidazole therapy.
- Patients taking metronidazole should be instructed to avoid alcohol ingestion during therapy and for 1 to 2 days after completion of therapy because of a possible disulfiram-like effect.
- At present, no satisfactory treatment is available for pregnant women with Trichomonas infections.
Evaluation of therapeutic outcomes
- Follow-up is considered unnecessary in patients who become asymptomatic after treatment with metronidazole.
- When patients remain symptomatic, it is important to determine if reinfection has occurred. In these cases, a repeat course of therapy, as well as identification and treatment or retreatment of infected sexual partners, is recommended.
Other sexually transmitted diseases
Several sexually transmitted diseases other than those previously discussed occur with varying frequency in the United States and throughout the world.



