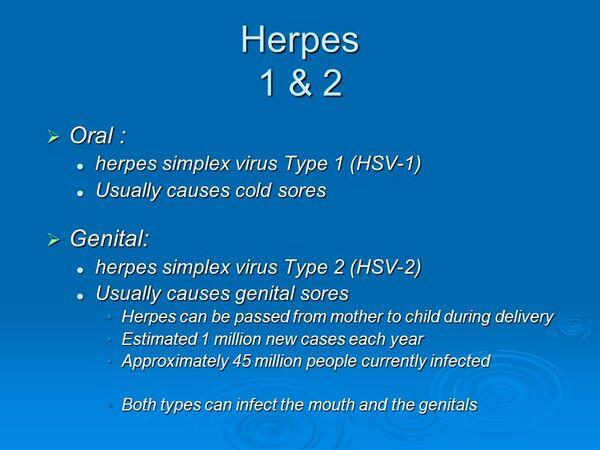
The term herpes is used to describe two distinct but antigenically related serotypes of herpes simplex virus. Herpes simplex virus type 1 (Herpes Simplex Virus-1) is most commonly associated with oropharyngeal disease; type 2 (Herpes Simplex Virus-2) is most closely associated with genital disease.
Diagnosis
- A presumptive diagnosis of genital herpes commonly is made on the basis of the presence of dark-field-negative, vesicular, or ulcerative genital lesions. A history of similar lesions or recent sexual contact with an individual with similar lesions also is useful in making the diagnosis.
- Tissue culture is the most specific (100%) and sensitive method (80% to 90%) of confirming the diagnosis of first-episode genital herpes
Treatment
- The goals of therapy in genital herpes infection are to shorten the clinical course, prevent complications, prevent the development of latency and/or subsequent recurrences, decrease disease transmission, and eliminate established latency.
- Palliative and supportive measures are the cornerstone of therapy for patients with genital herpes. Pain and discomfort usually respond to warm saline baths or the use of analgesics, antipyretics, or antipruritics.
- Specific chemotherapeutic approaches to treating genital herpes fall into six major areas: antiviral compounds, topical surfactants, photodynamic dyes, immune modulators, vaccines, and interferons.
- Specific recommendations are given in Table Treatment of Genital Herpes.
- Oral acyclovir, valacyclovir, and famciclovir are the treatments of choice for outpatients with first-episode genital herpes. Treatment does not prevent latency or alter the subsequent frequency and severity of recurrences.
- Continuous oral antiviral therapy reduces the frequency and the severity of recurrences in 70% to 90% of patients experiencing frequent recurrences.
- Acyclovir, valacyclovir, and famciclovir have been used to prevent reactivation of infection in patients seropositive for Herpes Simplex Virus who undergo transplantation procedures or induction chemotherapy for acute leukemia.
| TABLE. Presentation of Genital Herpes Infections | |||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
- The safety of acyclovir therapy during pregnancy is not established, although there is no evidence of teratogenic effects in humans.




