Otitis media
Definition
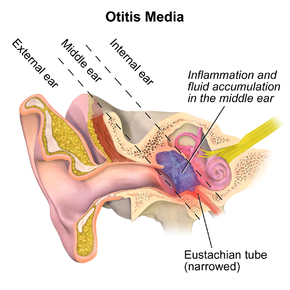
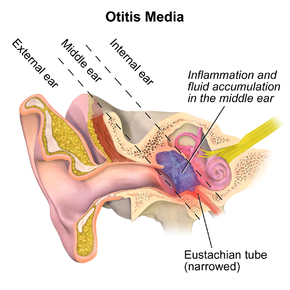
- Otitis media is an inflammation of the middle ear. Acute otitis media involves the rapid onset of signs and symptoms of inflammation in the middle ear that manifests clinically as one or more of the following: otalgia (denoted by pulling of the ear in some infants), hearing loss, fever, or irritability. Otitis media with effusion (accumulation of liquid in the middle ear cavity) differs from acute otitis media in that signs and symptoms of an acute infection are absent.
- Otitis media is the most frequent diagnosis in infants and children.
- Risk factors contributing to increased incidence of otitis media include the winter season, attendance at a day care center, non-breast feeding in infants, native American or Inuit origin, early age at first infection, and nasopharyngeal colonization with middle ear pathogens.
- Eustachian tube anatomy is different in children compared with adults and may cause improper drainage of the middle ear.
- Abnormal function of the eustachian tube can cause reflux transudation of liquid in the middle ear and proliferation of bacteria, resulting in acute otitis media.
Pathophysiology
- Streptococcus pneumoniae is the most common cause of acute otitis media (20% to 35%). Nontypable strains of Haemophilus influenzae and Moxarella catarrhalis are each responsible for 20% to 30% and 20% of cases, respectively. In 44% of cases, a viral etiology is found with or without concomitant bacteria.
- S. pneumoniae isolates are often intermediate resistant to penicillin (8% to 34%) and some are highly penicillin resistant (12% to 21%). Penicillin-resistant isolates are often resistant to multiple antibiotics. β- Lactam resistance occurs in about 23% to 35% of H. influenzae and in up to 100% of M. catarrhalis.
Clinical presentation
- Acute otitis media presents as an acute onset of signs and symptoms of middle ear infection such as otalgia, irritability, and tugging on the ear, following cold symptoims of runny nose, nasal congestion, or cough (Table Clinical Presentation of Acute Otitis Media).
- Resolution of acute otitis media occurs over 1 week. Pain and fever tend to resolve over 2 to 3 days.
Desired outcome
The goals of treatment include reduction in signs and symptoms, eradication of infection, and prevention of complications. Avoidance of unnecessary antibiotic use is another goal in view of S. pneumonia.
Treatment
- Antimicrobial therapy is used to treat otitis media; however, a high percentage of children will be cured with symptomatic treatment alone.
- Acetaminophen or a nonsteroidal anti-inflammatory agent, such as ibuprofen, can be used to relieve pain and malaise in acute otitis media. Decongestants, antihistamines, topical corticosteroids, or expectorants have not been proven effective for acute otitis media
| TABLE. Clinical Presentation of Acute Otitis Media |
| General |
| The acute onset of signs and symptoms of middle ear infection following cold symptoms of runny nose, nasal congestion, or cough |
| Signs and Symptoms |
| Pain that can be severe (>75% of patients)
Children may be irritable, tug on the involved ear, and have difficulty sleeping
Fever is present in less than 25% of patients and, when present, is more often in younger children
Examination shows a discolored, thickened, bulging eardrum
Pneumatic otoscopy or tympanometry demonstrates an immobile eardrum; 50% of cases are bilateral
Draining middle ear fluid occurs (<3% of patients) that usually reveals a bacterial etiology
|
| Laboratory Tests |
| Gram stain, culture, and sensitivities of draining fluid or aspirated fluid if tympanocentesis is performed |
|
- Surgical insertion of tympanostomy tubes (T tubes) is an effective method for the prevention of recurrent otitis media.
- Amoxicillin is the drug of choice for acute otitis media (40 to 45 mg/kg/day). High-dose amoxicillin (80 to 90mg/kg/day) is recommended if drug-resistant S. pneumoniae is suspected or a patient is at high risk for a resistant infection. Treatment recommendations for acute otitis media are found in Table Acute Otitis Media Treatment Recommendationsa.
- If treatment failure occurs with amoxicillin, an agent should be chosen with activity against β- lactamase-producing H. influenzae and M. catarrhalis as well as drug-resistant S. pneumoniae (such as amoxicillin-clavulanate, cefuroxime, or intramuscular ceftriaxone).
- Patients with penicillin allergy can be treated with a cephalosporin (some clinicians feel that the incidence of cross-reaction is sufficiently low in patients who have not experienced immediate pencillin-hypersensitivity reactions) or a macrolide such as azithromycin, or clarithromycin, erythromycin/ sulfisoxazole, trimethoprim/sulfamethoxazole, or, if S. pneumoniae is documented, clindamycin.
- It is difficult to identify who will benefit from antimicrobial therapy. With or without treatment, about 60% of children who have acute otitis media are symptom-free within 24 hours. In almost 40% of the remaining children, antibiotic use reduces the duration of symptoms by about 1 day.
- A meta-analysis reported no difference in cure rates with short (less than 7 days) and usual durations (at least 7 days) of antibiotic therapy in children. Five days of therapy is effective in acute uncomplicated otitis media.
Antibiotic Prophylaxis of Recurrent Infections
- Recurrent otitis media is defined as at least 3 episodes in 6 months or at least 4 episodes in 12 months. Recurrent infections are of concern because patients under 3 years of age are at high risk for hearing loss and language and learning disabilities. Data from studies generally do not favor prophylaxis. A meta-analysis demonstrated that prophylaxis against these infections leads to one infection prevented each time one child is treated for 9 months.
- Vaccination against influenza and pneumococcus may decrease risk of acute otitis media, especially in those with recurrent episodes. Immunization with the influenza vaccine reduces the incidence of acute otitis media by 36%.
- Treatment failure is a lack of clinical improvement after 3 days in the signs and symptoms of infection including pain, fever and redness or bulging of the tympanic membrane.
| TABLE. Acute Otitis Media Treatment Recommendationsa,b |
| Antibiotic Therapy in prior Month |
Day 0 |
Clinically Defined Treatment Failure Day 3 |
Clinically Defined Treatment Failures Days 10 to 28 |
| No |
Amoxicillin usual dose
40-45 mg/kg/day
|
Amoxicillin-clavulanate high dosec
Amoxicillin component 80-90 mg/kg/day clavulanate component 6.4 mg/kg/day
|
Same as day 3 |
| Amoxicillin high dose
80-90 mg/kg/day (high-risk patients)
|
Cefuroxime axetil
Suspension: 30 mg/kg/day divided twice daily (max: 1 g)
Tablets: 250 mg twice daily
Intramuscular ceftriaxone
1 g (50 mg/kg) daily for 3 days
|
| Yes |
Amoxicillin high dose
80-90 mg/kg/day
|
Intramuscular ceftriaxone
1 g (50 mg/kg) daily for 3 days
|
Amoxicillin-clavulanate high dose
Amoxicillin component 80-90 mg/kg/day
Clavulanate component 6.4 mg/kg/day
|
| Amoxicillin-clavulanate high dose |
Clindamycind |
Cefuroxime axetil |
| Amoxicillin component 80-90 mg/kg/day |
10-30 mg/kg/day divided every 6-8 h (max: 1.8 g/day) |
Suspension: 30 mg/kg/day divided twice daily (max: 1g) |
| Clavulanate component 6.4 mg/kg/day |
|
Tablets: 250 mg twice daily |
| Cefuroxime axetil |
Tympanocentesis |
Intramuscular ceftriaxone |
| Suspension: 30 mg/kg/day divided twice daily (max: 1 g) |
1 g (50mg/kg) daily for 3 days |
| Tablets: 250 mg twice daily |
Tympanocentesis |
| aThese recommendations are made by a group convened by the Centers for Disease Control. |
| bThe recommended duration of treatment for oral therapy is 7-10 days.
cHigher doses of clavulanate produce a significant increase in diarrhea.
dClindamycin is only recommended in cases of documented S. pneumoniae. It is not effective against H. influenzae or M. catarrhalis.
|
|
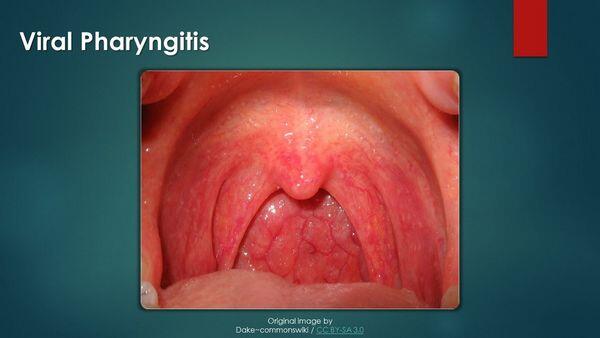
Pharyngitis
Pharyngitis is an acute infection of the oropharynx or nasopharynx that results in 1% to 2% of all outpatient visits. While viral causes are most common, group A β- hemolytic streptococcus, or streptococcus pyogenes, is the primary bacterial cause.
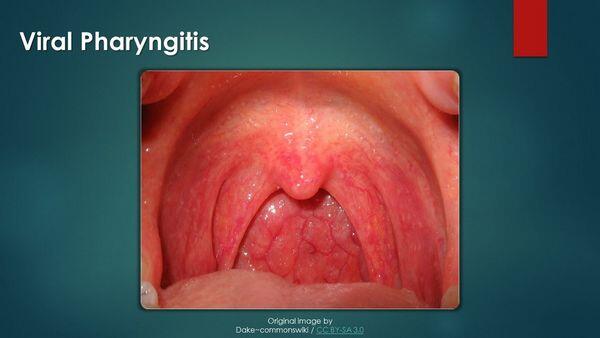
- Viruses cause most of the cases of acute pharyngitis. Specific etiologic agents include rhinovirus (20%), coronavirus (at least 5%), adenovirus (5%), influenza (2%) parainfluenza (2%), and Epstein-Barr virus (less than 1%). A bacterial etiology for acute pharyngitis is far less likely. Out of all of the bacterial causes, group A streptococcus is the most common (15 to 30% of persons of all ages with pharyngitis), and it is the the only commonly occurring form of acute pharyngitis for which antimicrobial therapy is indicated.
- Nonsuppurative complications such as acute rheumatic fever, acute glomerulonephritis, and reactive arthritis may occur as a result of pharyngitis with group A streptococcus.
Clinical presentation
- The incubation period is 2 to 5 days, and the illness often occurs in clusters.
- Guidelines from the Infectious Disease Society of America, American Academy of Pediatrics, and the American Heart Association suggest that testing for group A streptococcus be done in all patients with signs and symptoms. Only those with a positive test for group A Streptococcus require antibiotic treatment.
- There are several options to test for group A streptococcal pharyngitis. A throat swab can be sent for culture or used for rapid antigen detection testing.
Treatment
- The goals of treatment of pharyngitis are to improve clinical signs and symptoms, minimize adverse drug reactions, prevent transmission to close contacts, and prevent acute rheumatic fever and suppurative complications such as peritonsillar abscess, cervical lymphadenitis, and mastoiditis.
| TABLE. Clinical Presentation and Diagnosis of Group A streptococcal Pharyngitis |
| General |
| A sore throat of sudden onset that is mostly self-limited
Fever and constitutional symptoms resolving in about 3-5 days
Clinical signs and symptoms are similar for viral causes as well as nonstreptococcal bacterial causes
|
| Signs and Symptoms |
| Sore throat
Pain on swallowing
Fever
Headache, nausea, vomiting, and abdominal pain (especially children)
Erythema/inflammation of the tonsils and pharynx with or without patchy exudates
Enlarged, tender lymph nodes
Red swollen uvula, petechiae on the soft palate, and a scarlatiniform rash
Several symptoms that are not suggestive of group A Streptococcus are cough, conjunctivitis, coryza, and diarrhea
|
| Laboratory Tests |
| Throat swab and culture or rapid antigen detection testing. |
|
- Antimicrobial therapy should be limited to those who have clinical and epidemiological features of Group A streptococcal pharyngitis with a positive laboratory test.
- As pain is often the primary reason for visiting a physician, emphasis on analgesics such as acetaminophen and nonsteroidal anti-inflammatory drugs (nonsteroidal anti-inflammatory drugs) to aid in pain relief is strongly recommended. However, acetaminophen is a better option because there is some concern that nonsteroidal anti-inflammatory drugs may increase the risk for necrotizing fasciitis or toxic shock syndrome. Either systemic or topical analgesics can be used, as well as antipyretics and other supportive care including rest, fluids, lozenges, and salt water gargles.
- Antimicrobial treatment should be limited to those who have clinical and epidemiological features of group A streptococcal pharyngitis with a positive laboratory test. Penicillin is the drug of choice in the treatment of group A streptococcal pharyngitis (Table Dosing Guidelines for Pharyngitis). Table Antibiotics and Dosing for Recurrent Episodes of Pharyngitis presents dosing guidelines for recurrent infections.
- In patients allergic to penicillin, a macrolide such as erythromycin or a first-generation cephalosporin such as cephalexin (if the reaction is non IgE-mediated hypersensitivity with hives or anaphylaxis) can be used. Newer macrolides such as azithromycin and clarithromycin are as effective as erythromycin and cause fewer gastrointestinal adverse effects.
- If patients are unable to take oral medications, intramuscular benzathine penicillin can be given although it is painful and no longer available in canada.
Evaluation of therapeutic outcomes
- Most cases of pharyngitis are self-limited; however, antimicrobial therapy will hasten resolution when given early to proven cases of group A streptococcus. Fever generally resolves by 3 to 5 days, and most other acute symptoms by 1 week. Tonsils and lymph nodes may take a few weeks to return to baseline. Children should be kept home from daycare or school until afebrile and for the first 24 hours after antimicrobial treatment is initiated, after which time transmission is unlikely. Follow-up testing is generally not necessary for index cases or in asymptomatic contacts of the index patient.
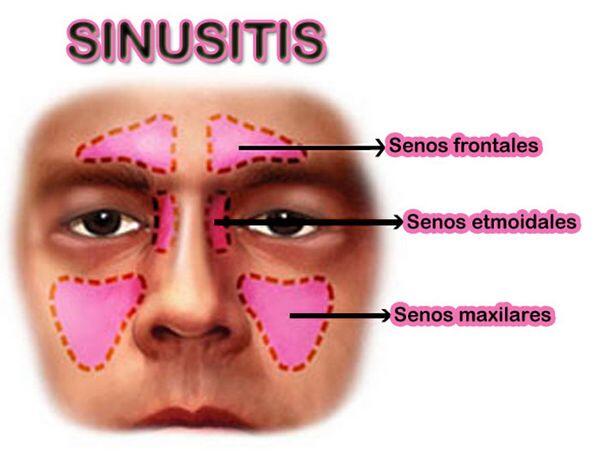
Sinusitis
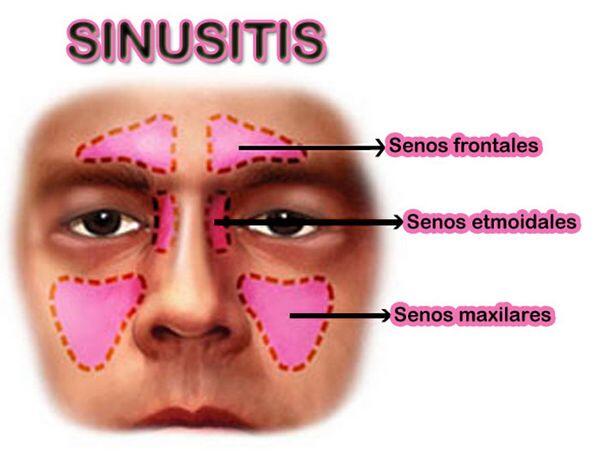
- Sinusitis is an inflammation and/or infection of the paranasal sinus mucosa. The term rhinosinusitis is used by some specialists, because sinusitis typically also involves the nasal mucosa. The majority of these infections are viral in origin. It is important to differentiate between viral and bacterial sinusitis to aid in optimizing treatment decisions.
- Bacterial sinusitis can be categorized into acute and chronic disease. Acute disease lasts less than 30 days with complete resolution of symptoms. Chronic sinusitis is defined as episodes of inflammation lasting more than 3 months with persistence of respiratory symptoms.
- Acute bacterial sinusitis is most often caused by the same bacteria implicated in acute otitis media: Streptococcus pneumoniae and Haemophilus influenzae. These organisms are responsible for about 70% of bacterial causes of acute sinusitis in both adults and children. Chronic sinusitis can be polymicrobial, with an increased prevalence of anaerobes as well as less common pathogens including gram-negative bacilli and fungi.
| TABLE. Dosing Guidelines for Pharyngitis |
| Drug |
Adult Dosage |
Pediatric Dosage |
Duration |
| Penicillin VK |
250 mg 3 times daily or 4 times daily or 500 mg twice daily |
50 mg/kg/day divided in 3 doses |
10 days |
| Penicillin benzathine |
1.2 million units intramuscularly |
0.6 million units for under 27 kg (50,000 units/kg) |
1 dose |
| Penicillin G procaine and benzathine mixture |
Not recommended in adolescents and adults |
1.2 million units (benzathine 0.9 million units, procaine 0.3 million units) |
1 dose |
| Amoxicillin |
500 mg 3 times daily |
40-50 mg/kg/day divided in 3 doses |
10 days |
| Erythromycin |
10 days |
| Estolate |
20-40 mg/kg/day divided 2-4 times daily (max: 1 g/day) |
Same as adults |
| Stearate |
1 g daily divided 2-4 times daily (adolescents, adults) |
– |
| Ethylsuccinate |
40 mg/kg/day divided 2-4 times daily (max: 1 g/day) |
Same as adults |
| Cephalexin |
250-500 mg orally 4 times daily |
25-50 mg/kg/day divided in 4 doses |
10 days |
|
| TABLE. Antibiotics and Dosing for Recurrent Episodes of Pharyngitis |
| Drug |
Adult Dosage |
Pediatric Dosage |
| Clindamycin |
600 mg orally divided in 2-4 doses |
20 mg/kg/day in 3 divided doses (max: 1.8 g/day) |
| Amoxicillin-clavulanate |
500 mg twice daily |
40 mg/kg/day in 3 divided doses |
| Penicillin benzathine |
1.2 million units intramuscularly for 1 dose |
0.6 million units for under 27 kg (50,000 units/kg) |
| Penicillin benzathine with rifampin |
As above
20 mg/kg/day orally in 2 divided doses x last 4 days of treatment with penicillin
|
As above
Rifampin dose same as adults
|
|
| TABLE. Clinical Presentation and Diagnosis of Bacterial Sinusitis42-44,46-49 |
| General |
| A nonspecific upper respiratory tract infection that persists beyond 7-14 days |
| Signs and Symptoms |
| Acute
Adults:
Nasal discharge/congestion
Maxillary tooth pain, facial or sinus pain that may radiate (unilateral in particular) as well as deterioration after initial improvement
Severe or persistent (beyond 7 days) signs and symptoms are most likely bacterial and should be treated with antimicrobials
Children:
Nasal discharge and cough for greater than 10-14 days or severe signs and symptoms such as temperature 39В°C or facial swelling or pain are indications for antimicrobial therapy
|
| Chronic
Symptoms are similar to those of acute sinusitis but more nonspecific
Rhinorrhea is associated with acute exacerbations
Chronic unproductive cough, laryngitis, and headache may occur
Chronic/recurrent infections occur 3-4 times a year and are unresponsive to steam and decongestants
|
|
| TABLE. Approach to Treatment of Acute Bacterial Sinusitis |
| Uncomplicated sinusitis |
Amoxicillin |
| Uncomplicated sinusitis, penicillin-allergic patient |
Immediate-type hypersensitivity: Clarithromycin or azithromycin or trimethoprim-sulfamethoxazole
Nonimmediate-type hypersensitivity: β- Lactamase-stable cephalosporin
|
| Treatment failure or prior antibiotic therapy in past 4-6 wk |
High-dose amoxicillin with clavulanate or β- lactamase-stable cephalosporin |
| High suspicion of penicillin-resistant S. pneumoniae |
High-dose amoxicillin or clindamycin |
|
| TABLE. Dosing Guidelines for Acute Bacterial Sinusitis |
| Drug |
Adult Dosage |
Pediatric Dosage |
| Amoxicillin |
500 mg 3 times daily
High dose: 1 g 3 times daily
|
Low dose: 40-50 mg/kg/day divided in 3 doses
High dose: 80-100 mg/kg/day divided in 3 doses
|
| Amoxicillin-clavulanate |
500/125 mg 3 times daily |
40-50 mg/kg/day divided in 3 doses
High dose: Can add 40-50 mg/kg/day amoxicillin
|
| Cefuroxime |
250-500 mg twice daily |
15 mg/kg/day divided in 2 doses |
| Cefaclor |
250-500 mg 3 times daily |
20 mg/kg/day divided in 3 doses |
| Cefixime |
200-400 mg twice daily |
8 mg/kg/day in 1 dose or divided in 2 doses |
| Cefdinir |
600 mg daily or divided in 2 doses |
14 mg/kg/day in 1 dose or divided in 2 doses |
| Cefpodoxime |
200 mg twice daily |
10 mg/kg/day in 2 divided doses (max: 400 mg daily) |
| Cefprozil |
250-500 mg twice daily |
15-30 mg/kg/day divided in 2 doses |
| Trimethoprim-sulfamethoxazole |
160/800 mg every 12 h |
6-8 mg/kg/day trimethoprim, 30-40 mg/kg/day sulfamethoxazole divided in 2 doses |
| Clindamycin |
150-450 mg every 6 h |
30-40 mg/kg/day divided in 3 doses |
| Clarithromycin |
250-500 mg twice daily |
15 mg/kg/day divided in 2 doses |
| Azithromycin |
500 mg day 1, then 250 mg/day x 4 days |
10 mg/kg day 1, then 5 mg/kg/day x 4 days |
| Levofloxacin |
500 mg daily |
N/A |
| N/A, not applicable. |
|
Clinical presentation
Treatment
- The goals of treatment of acute sinusitis are the reduction in signs and symptoms, achieving and maintaining patency of the ostia, limiting antimicrobial treatment to those who may benefit, eradication of bacterial infection with appropriate antimicrobial therapy, minimizing the duration of illness, prevention of complications, and prevention of progression from acute disease to chronic disease.
- Approximately 40% to 60% of patients with acute sinusitis will recover spontaneously (these are likely patients with viral sinusitis).
- Nasal decongestant sprays such as phenylephrine and oxymetazoline that reduce inflammation by vasoconstriction are often used in sinusitis. Use should be limited to the recommended duration of the product to prevent rebound congestion. Oral decongestants may also aid in nasal or sinus patency. To reduce mucociliary function, irrigation of the nasal cavity with saline and steam inhalation may be used to increase mucosal moisture, and mucolytics (e.g. guaifenesin) may be used to decrease the viscosity of nasal secretions. Antihistamines should not be used for acute bacterial sinusitis in view of their anticholineric effects that can dry mucosa and disturb clearance of mucosal secretions.
- Antimicrobial therapy is superior to placebo in reducing or eliminating symptoms, although the benefit is small.
- Amoxicillin is first-line treatment for acute bacterial sinusitis. It is cost effective in acute uncomplicated disease, and intial use of newer broad-spectrum agents is not justified.
- The current recommendations are 10 to 14 days, or at least 7 days, of antimicrobial therapy after signs and symptoms are under control.