Definition of Tinea Corporis
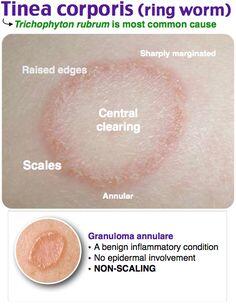
The term tinea corporis is used to refer to dermatophyte infections of the trunk, legs and arms, but excluding the groin, hands and feet.
Geographical distribution of Tinea Corporis
The condition is worldwide in distribution, but is most prevalent in tropical and subtropical regions.
Causal organisms
Tinea corporis is caused by E. floccosum and many species of Trichophyton and Microsporum. Infection with anthropophilic species, such as E. floccosum or T. rubrum often follows autoinoculation from another infected body site, such as the feet. Tinea corporis caused by T. tonsurans is sometimes seen in children with tinea capitis and their close contacts.
Tinea corporis commonly occurs following contact with infected household pets or farm animals, but occasional cases result from contact with wild mammals or contaminated soil. M. canis is a frequent cause of human infection, and T. verrucosutn infection is common in rural areas. Tinea corporis is more common among individuals in regular contact with animals or with the soil. Human-to-human spread of infection with geophilic or zoophilic species is unusual.
Essential investigations and their interpretation
Material for mycological investigation should be collected from the raised border of the lesion by scraping outwards with a blunt scalpel held perpendicular to the skin. If vesicles are present, the entire top should be submitted for examination.
Direct microscopic examination of infected material should reveal the branching hyphae characteristic of a dermatophyte infection.
Isolation of the aetiological agent in culture will permit the species of fungus involved to be determined. This will provide information as to the source of the infection and aid the selection of appropriate treatment.
Management of Tinea Corporis
Topical antifungal preparations are the treatment of choice for localized lesions. Four imidazoles (clotrimazole, econazole, miconazole and sulconazole) and two allylamine compounds (naftifine and terbinafine) are available in a number of topical formulations. All give similar high cure rates (70-100%) and side-effects are uncommon. These drugs should be applied morning and evening for 2-4 weeks. Treatment should be continued for at least 1 week after the lesions have cleared and the medication should be applied at least 3 cm beyond the advancing margin of the lesion.
If the lesions are extensive or the patient fails to respond to topical preparations, oral treatment is usually indicated. Itraconazole (100 mg/day for 2 weeks) and terbinafine (250 mg/day for 2-4 weeks) have proved more effective than griseofulvin (10 mg/kg per day for 4 weeks).





