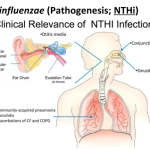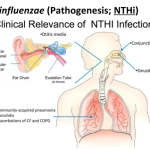
H influenzae was first isolated during the 1892 influenza pandemic and was originally believed to be the causative agent of influenza. Although subsequent studies revealed the fallacy of this idea, H influenzae has proved to be a common cause of localized respiratory tract and systemic disease, including meningitis, epiglottitis, pneumonia, pyogenic arthritis, cellulitis, otitis media, and sinusitis, among others (Box 1). Meningitis is the most common and serious form of invasive H influenzae type-b disease. In the mid-1980s, before the introduction of effective vaccines, ~ 10,000-12,000 cases of H influenzae type-b meningitis occurred in the United States each year, and 95% of cases involved children < 5 years old.