P PSEUDOMALLEI MELIOIDOSIS
This organism is endemic in Southeast Asia with the highest prevalence in Thailand. The organism is a saprophyte living in the soil. Infection may be subclinical, acute, subacute, or chronic. Pulmonary infection is most common. Histologically, the acute illness is represented by lung abscesses and the subacute form by caseation necrosis. Upper lobe cavities must be distinguished from those caused by tuberculosis. Debilitated patients may develop hematogenous spread of the organism to other organs. Skin lesions from direct inoculation cause suppurative lesions often in association with nodular lymphangitis and regional lymphadenopathy.
Diagnosis is made in a patient from an endemic area with a compatible clinical illness who has a positive P pseudomallei culture or a fourfold increase or decrease in antibody titer. Appropriate therapy requires a combination of antimicrobial agents and surgical drainage. Ceftazidime alone or in combination with either trimethoprim-sulfamethoxazole or amoxicillin clavulanate is the therapy of choice. The duration of therapy ranges from 3 to 12 months with the longest duration of treatment necessary in chronic extrapulmonary disease. Imipenem, piperacillin-tazobactam, chloramphenicol, and tetracycline are alternative agents; the microorganism is resistant to ciprofloxacin and aztreonam.
P MALLEI (GLANDERS)
Infection with P mallei (glanders) is the result of contact with an infected equine source such as horses, donkeys, or mules. The disease is confined to Africa, Asia, and South America. Human disease takes the following forms: acute suppurative infection with localized nodules and lymphangitis, mucocutaneous granuloma and ulcer, acute pulmonary infection with nodules and lymphadenopathy, acute septicemia, or a chronic suppurative form.
Seroconversion or recovery of P mallei from culture confirms the diagnosis. Antimicrobial therapy is usually with the same agents effective for melioidosis administered for a period of 1-2 months often combined with surgical drainage.
STENOTROPHOMONAS MALTOPHILIA
This organism is a free-living microorganism that causes nosocomial infection in debilitated patients particularly in the intensive care or chronic ventilatory units. Infections encountered include pneumonia, UTI, wound infection, bacteremia, and, rarely, peritonitis, cholangitis, or endovascular infections.
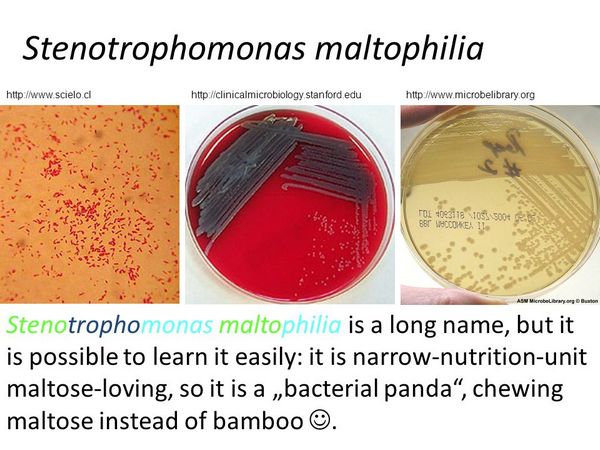
The emergence of this bacterium as a serious pathogen is caused by its antibiotic resistance pattern. It produces inducible ß-lactamases and has low outer membrane permeability but is often susceptible to trimethoprim-sulfamethoxazole or ticarcillin-clavulanate. Alternative agents include ciprofloxacin, minocycline, doxycycline, and occasionally third-generation cephalosporins, but the microorganism is usually resistant to carbapenem or aminoglycosides.
BURKHOLDERIA CEPACIA
This microorganism is a cause of nosocomial infections similar to those caused by Stenotrophomonas maltophilia. It is also an important pathogen in patients with CF, and infection is associated with progressive lung disease and high mortality. CF patients who are colonized with B cepacia preoperatively and undergo lung transplantation have higher post-transplantation mortality than those who are not colonized. In CF clinics, colonization rates are high. B cepacia is resistant to aminoglycosides and most ß-lactam agents. Some strains are variably susceptible to third-generation cephalosporins, ciprofloxacin, trimethoprim-sulfamethoxazole, ampicillin-sulbactam, chloramphenicol, or meropenem.



