Classical pertussis occurs in three clinical stages: catarrhal, paroxysmal, and convalescent (Box 5).
Clinical Findings
Signs and Symptoms
The catarrhal stage is characterized by nonspecific upper respiratory symptoms, including rhinorrhea, mild cough, and low-grade fever. During this stage, which typically lasts 1-2 weeks, the disease is highly communicable. The paroxysmal stage is marked by sudden attacks or paroxysms of severe, repetitive coughing, often culminating with the characteristic whoop and frequently followed by vomiting. A marked lymphocytosis usually accompanies this stage of the disease, with lymphocyte counts sometimes exceeding 50,000/mm3 and usually representing 70% or more of total circulating leukocytes. The paroxysmal stage typically lasts 1-4 weeks and can be associated with a variety of complications, including secondary bacterial infections such as pneumonia and otitis media, toxic central nervous system manifestations such as seizures and encephalopathy, and effects of increased intrathoracic and intra-abdominal pressure such as pneumothorax, hernia, and rectal prolapse. The beginning of the convalescent (recovery) stage is marked by a reduction in frequency and intensity of coughing spells. After clinical pertussis, immunity to disease is lifelong.
Although most cases of pertussis follow a characteristic course, exceptions exist. In infants < 3 months, the catarrhal stage is usually no longer than a few days, and the paroxysmal and convalescent stages are extremely protracted, with coughing spells that continue throughout the first year of life. In infants < 6 months, apnea is a common manifestation, and the whoop is often absent. Paradoxically, in infants, cough and whoop may become louder and more classic during convalescence, reflecting growth in body mass and increased strength. In immunized children, all three stages are shortened, and in adults, only a protracted cough may be present. Post-tussive vomiting is common in pertussis at all ages and is a major clue to the diagnosis in adolescents and adults. With subsequent respiratory illnesses over the next several months, paroxysmal coughing may recur, though not because of recurrence of active Bordetella infection.
Laboratory Findings
During the catarrhal stage, organisms are most readily isolated from cultures of the posterior nasopharynx. During the paroxysmal stage, it is increasingly difficult to recover the organism from the respiratory tract.
Imaging
The chest radiograph is mildly abnormal in the majority of hospitalized infants, showing perihilar infiltrates or interstitial edema and patchy atelectasis. Pneumothorax, pneumomediastinum, and soft tissue air are sometimes seen.
Complications
Surveillance data on pertussis in the United States from 1980 to 1989 demonstrated that the clinical course in infants was complicated by pneumonia in 21.7% of cases, by seizures in 3.0% of cases, and by encephalopathy in 0.9% of cases. The mortality rate was 1.3% in infants < 1 month and 0.3% in infants 2-11 months of age. Considering all individuals with pertussis, pneumonia develops in ~ 10%, seizures in ~ 2%, and encephalopathy in 0.5% to 1%.
Diagnosis
The traditional approach for diagnosing pertussis involves culturing B pertussis or B parapertussis from nasopharyngeal mucus (see Table 2). Mucus should be collected by aspiration or by swabbing the nasopharynx with a dacron or calcium alginate swab. After plating on an appropriate medium, B pertussis is usually detected in 3-5 days, and B parapertussis is visible in 2-4 days. Regan-Lowe agar or a related charcoal-horse blood agar containing 40 ug/mL cephalexin is the preferred medium for primary isolation.
The organism is rarely found after the fourth week of illness, and culture is less likely to be positive in immunized individuals and in those who have received antibiotics. Examination of nasopharyngeal secretions by direct immunofluorescent assay is considered an alternative approach to diagnosis. However, direct immunofluorescent assay has low sensitivity and variable specificity and requires experienced personnel for interpretation. Polymerase chain reaction has been used on an investigational basis and is more rapid than culture but is variably sensitive.
B pertussis infections stimulate a heterogeneous antibody response that differs among individuals, depending on age, previous exposure to the organism, and immunization status, and thus no single serologic test is diagnostic. Nevertheless, in experienced research laboratories, the serologic diagnosis of pertussis has excellent sensitivity and specificity when acute serum is collected early in the illness and paired acute and convalescent sera are tested for antibodies to a number of antigens.
Absolute lymphocytosis is often present in patients with classic pertussis but represents a nonspecific finding, especially in infants. The degree of lymphocytosis usually parallels the severity of the patient’s cough. The lymphocytes include both T cells and B cells and are normal small cells rather than large atypical lymphocytes. Adults and partially immunized children have less marked increases in lymphocyte count.
Because laboratory confirmation of pertussis can be difficult, clinicians often need to make the diagnosis on the basis of characteristic manifestations, including a prolonged paroxysmal cough, an inspiratory whoop, post-tussive emesis, and lymphocytosis. For sporadic cases, cough of > 14 days duration in combination with either paroxysms, whoop, or post-tussive vomiting has a sensitivity of 81% and a specificity of 58% for culture confirmation. In a study of university students, 25% of subjects with a coughing illness for 7 or more days had pertussis.
Treatment
Infants < 6 months and other patients with potentially severe disease often require hospitalization for supportive care to manage coughing paroxysms, apnea, cyanosis, feeding difficulties, and other complications. Antibiotic therapy initiated during the catarrhal stage promotes more rapid clinical improvement (Box 6). However, after the onset of paroxysms, antimicrobial agents usually have little discernible effect on the course of illness. Nevertheless, they are recommended to limit the spread of the organism to others. The drug of choice is erythromycin. Currently, the recommended duration of therapy is 14 days, although recent evidence suggests that a 7-day course is also efficacious. Azithromycin and clarithromycin are alternatives based on clinical studies demonstrating the ability of these drugs to eradicate the organism.
Trimethoprim/sulfamethoxazole is another possible alternative, but its efficacy is unproven. In in vitro studies, B pertussis is also susceptible to fluoroquinolones and to a lesser extent ampicillin and rifampin. B parapertussis is less susceptible in vitro to all agents except erythromycin.
Among patients with pertussis who are treated with erythromycin, nasopharyngeal cultures almost always become negative within 5 days after initiating therapy. In order to prevent secondary transmission effectively, antibiotic treatment also should be prescribed for all household and other close contacts, including those who have been immunized against B pertussis, since vaccine-induced immunity is not absolute and may not prevent infection. Individuals exposed to a patient with pertussis should be closely monitored for respiratory symptoms over the ensuing 2-3 weeks.
Corticosteroids, albuterol, and pertussis-specific immunoglobulin may be effective in reducing paroxysms of coughing but require further evaluation before they can be recommended.
Prevention & Control
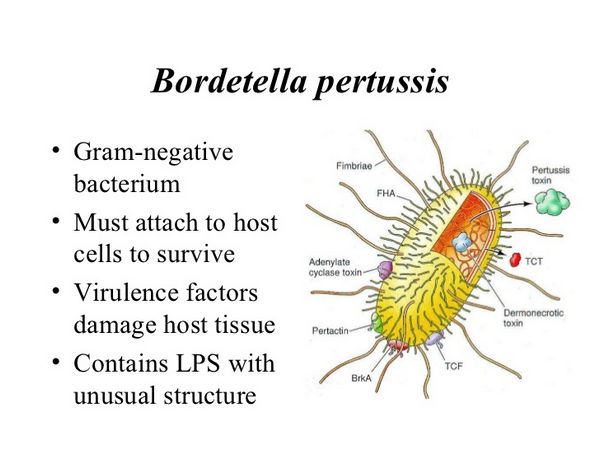
Universal immunization with pertussis vaccine is critical for control of pertussis (Box 7). Whole-cell and acellular pertussis vaccines in combination with diphtheria and tetanus toxoids (DTP and DTaP, respectively) are available in the United States and should be administered to all children < 7 years. The primary series includes doses at 2, 4, 6, and 15-18 months of age, followed by a booster at 4-6 years of age. Whole-cell vaccines are prepared from a suspension of inactivated B pertussis cells, whereas acellular vaccines contain one or more antigens derived from B pertussis and lack endotoxin. These antigens include pertussis toxin, filamentous hemagglutinin, fimbriae type 2, fimbriae type 3, and pertactin. All acellular vaccines contain pertussis toxin, in an inactivated form.
Based on household studies of children in the United States exposed to pertussis, the efficacy of whole-cell vaccines for children who received at least three doses is estimated to be 50 to 90%, depending on the case definition. Protection is greatest against culture-confirmed, more severe cases. Vaccine-induced immunity persists for at least 3 years and then diminishes. Although whole-cell vaccines have been highly effective in reducing the burden of disease and deaths due to B pertussis, they are associated with a number of troublesome adverse effects, including redness, induration, and tenderness at the injection site, low-grade fever, drowsiness, irritability, and anorexia. Less common serious adverse reactions include seizures, hypotonic-hyporesponsive episodes, fever > 40 °C, and persistent, severe, inconsolable crying lasting 3 or more hours. Encephalopathy, other neurologic conditions, and sudden infant death syndrome have been attributed to vaccination with whole-cell pertussis vaccines, but evidence for a causal association is lacking.
Acellular pertussis vaccines were first demonstrated to be efficacious in studies in Japan involving children 2 years of age and older, and in 1991, two different formulations were licensed in the United States for use as the fourth and fifth (booster) doses in the routine series. More recent studies in Europe compared acellular and whole-cell vaccines in infants and found them to be associated with similar levels of protective efficacy. Concentrations of serum antibody to PT, FHA, fimbriae, and pertactin were at least as high after immunization with the acellular vaccines as they were after vaccination with a whole-cell vaccine. Furthermore, adverse reactions were significantly less frequent among recipients of the acellular vaccines. With this information in mind, five acellular vaccines are now approved in the United States for use during infancy, and licensure of additional products is anticipated. Given their efficacy and safety profile, acellular vaccines are preferred over whole cell vaccines in the United States.
Once a case of pertussis has been diagnosed, all contacts should be identified. Close contacts < 7 years who have received fewer than four doses of pertussis vaccine (DTP or DTaP) should have pertussis immunization initiated or continued. As mentioned above, contacts should also receive chemoprophylaxis with erythromycin or a suitable alternative.
For the hospitalized patient, droplet precautions are recommended for 5 days after initiation of effective therapy. Similarly, outpatients should be excluded from day care or school until 5 days of treatment are completed. If antibiotic therapy is not administered, precautions should be continued until 3 weeks after the onset of paroxysms.






