Description of Medical Condition
Inflammation of the bladder mucosa. This topic refers primarily to infectious cystitis. Other urinary tract infections are discussed elsewhere.
System(s) affected: Renal/Urologic
Genetics: N/A
Incidence/Prevalence in USA: 3-8% of women have bacteriuria at any given time. 30% of females have at least one UTI; 7 million doctor visits a year
Predominant age: Young adults and older Predominant sex: Female
Medical Symptoms and Signs of Disease
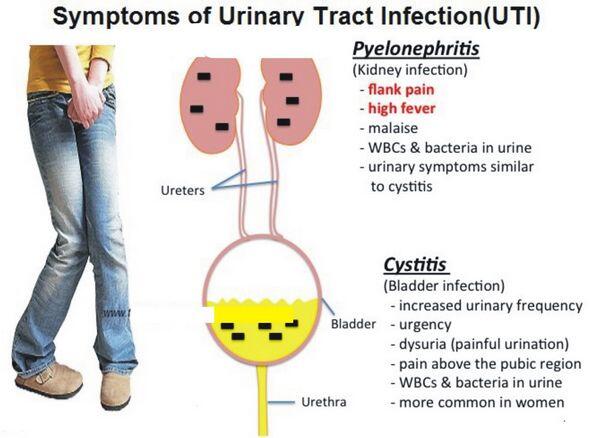
Note: Any or all may be present
- Burning during urination
- Pain during urination
- Urgency (sensation of need to urinate frequently)
- Frequency
- Sensation of incomplete bladder emptying
- Blood in urine
- Lower abdominal pain or cramping
- Offensive odor of urine
- Nocturia
What Causes Disease?
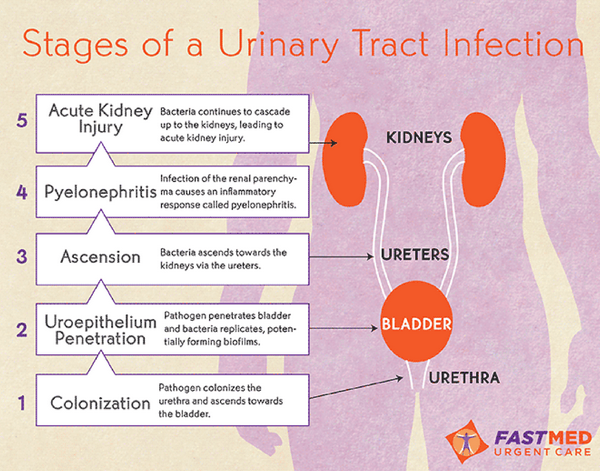
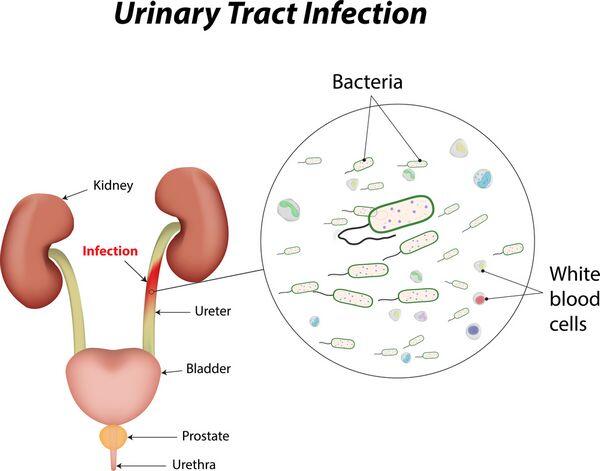
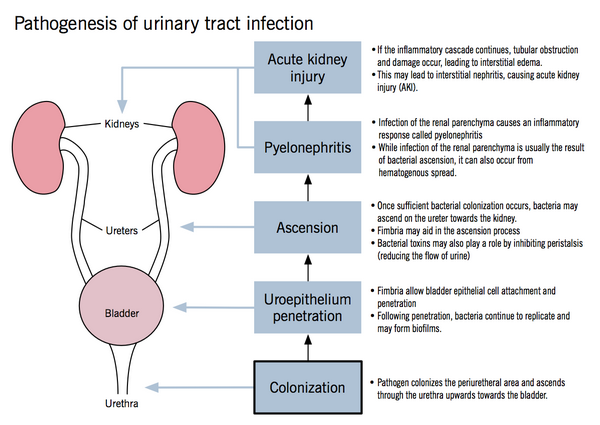
Acute infection, usually with gram negative bacteria (E. coli in >90% of uncomplicated cystitis).
Risk Factors
- Previous urinary tract infection
- Diabetes mellitus
- Pregnancy
- More frequent or vigorous sexual activity than usual
- Use of spermicides or diaphragm
- Underlying abnormalities of the urinary tract such as tumors, calculi, strictures, incomplete bladder emptying, etc.
Diagnosis of Disease
Differential Diagnosis
- Vaginitis
- Sexually transmitted diseases causing urethritis or pyuria
- Hematuria from causes other than infection (e.g. neoplasia, calculi)
- Interstitial cystitis
- Psychological dysfunction
Laboratory
- Urinalysis demonstrating pyuria (more than 10 neutrophils per high power field on microscopic exam). Leukocyte esterase dipsticks also useful for detecting pyuria but fail to detect pyuria in up to 20% of patients, and false positives occur from vaginal leukocytes.
- Urinalysis demonstrating bacteriuria (any amount on unspun urine, or 10 rod-shaped bacteria per high power field on centrifuged urine). Nitrite dipsticks also useful (and 94% specific), but fail to detect bacteriuria in 30-50% of patients. Nitrite dipsticks may be negative in patients who do not eat meat.
- Urine culture demonstrating growth of single species of bacteria. Suspect contaminated specimen when culture shows multiple types of bacteria.
Drugs that may alter lab results: N/A Disorders that may alter lab results: N/A
Pathological Findings
N/A
Imaging
For all infants and may be indicated for older patients with recurrent infections:
- Ultrasound imaging is first choice test
- For infants and children, obtain ultrasound and if ureteral dilation detected, obtain either voiding cysto-urethrogram or isotope cystogram to detect reflux
Diagnostic Procedures
- Suprapubic bladder aspiration or urethral catheterization to obtain urine specimen from infants
- Urethral catheterization to obtain urine specimen from children and adults if voided urine suspected of being contaminated
- Classic symptoms in non-pregnant young adult female with first episode of UTI require no urine culture for diagnosis. Obtain urinalysis and culture in other age groups, if repeat episode, if pregnant, or if symptoms not classic.
- Some recent research suggests the most cost-effective approach is empiric treatment without lab tests in non-pregnant premenopausal women with symptoms of UTI and no risks for complicated infection
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient, except for complicated or upper tract infections
General Measures
- Maintain good hydration
- One-fourth of women with simple UTI experience a second UTI within six months, and half at some time during lifetime. Patients with multiple recurrent UTI and no underlying urinary tract abnormality may receive long-term prophylactic antibiotic treatment. Trimethoprim-sulfamethoxazole and nitrofurantoin commonly used.
- Patients with chronic indwelling urinary catheters always have colonization of urine, usually with multiple bacterial species. This should not be treated unless symptomatic with fever, sepsis, or other systemic symptoms.
- Preliminary studies indicate that Vaccinium macrocarpon (Cranberry Juice) may help prevent and treat UTIs by inhibiting bacterial adherence to bladder epithelium
Activity
Avoid sexual intercourse when symptoms present
Diet
No special diet
Patient Education
- Take antibiotic as directed
- Return if symptoms not resolved or markedly improved within 48 hours
- Return if fever, chills, or flank pain develop
- If taking prophylactic antibiotics, take at bedtime
Medications (Drugs, Medicines)
Drug(s) of Choice
- First, rare, or infrequent UTI in older children, adolescents, and adults who are nonpregnant, nondiabetic afebrile, nonimmunocompromised and have no abnormality of the urinary tract (i.e., uncomplicated). New studies show 3 day therapy is OK for children.
- 3 day treatment with fluoroquinolone or trimethoprim-sulfamethoxazole (TMP-SMX) Increasing resistance being reported to TMP-SMX. It is the preferred treatment if local sensitivity patterns indicate low resistance rates.
- Postcoital
- Single-dose TMP-SMX or cephalexin may reduce frequency of UTI in sexually active women
- Pregnant patients
- 010-14 day or longer treatment with pregnancy-safe antibiotic chosen based on culture/sensitivity results. May begin with cephalosporin, amoxicillin, or other antibiotic while awaiting culture/sensitivity results.
- All other patients
- 010-14 day treatment with antibiotic chosen based on culture/sensitivity results. May begin with fluoroquinolone, TMP-SMX, cephalosporin or other antibiotic while awaiting culture/sensitivity results.
Contraindications: Refer to manufacturer’s literature. Fluoroquinolones not safe during pregnancy or for treatment of children. TMP/SMX use in pregnancy not desirable (especially in 3rd trimester), but appropriate in some circumstances. Precautions: Refer to manufacturer’s literature Significant possible interactions: Refer to manufacturer’s literature
Alternative Drugs
Change antibiotic if indicated by culture/sensitivity results
Patient Monitoring
- First or rare UTI: In young or middle-age, nonpregnant adult female requires no followup if patient cured after 3 day therapy. If not resolved within two to three days, obtain culture/sensitivity and change antibiotic accordingly.
- All other patients should have post-treatment urine culture to document eradication of infection
Prevention / Avoidance
- Maintain good hydration
- Women with frequent or intercourse-related UTI should empty bladder immediately before and following intercourse and consider postcoital antibiotic treatment
- Avoid feminine hygiene sprays and scented douches
- Wipe urethra from front to back
Possible Complications
- Pyelonephritis or sepsis
- Renal abscess
- Acute urinary outlet obstruction
Expected Course / Prognosis
Symptoms resolve within 2-3 days after starting treatment in almost all patients
Miscellaneous
Associated Conditions
Described under Risk Factors
Age-Related Factors
Pediatric: Infants and young children with cystitis are at higher risk of pyelonephritis Geriatric:
- Elderly may have bacteriuria without symptoms; generally does not require treatment if urinary tract otherwise normal
- Elderly more apt to have underlying urinary tract abnormality
- Acute UTI sometimes associated with incontinence or mental status changes in the elderly
Pregnancy
UTI during pregnancy always requires culture/sensitivity and usually requires 10-14 day treatment. Following treatment of acute infection, pregnant women often receive prophylactic antibiotics for the remainder of pregnancy.
Synonyms
Cystitis
International Classification of Diseases
595.0 Acute cystitis
See Also
Pyelonephritis Urinary tract infection in males
Description of Medical Condition
Cystitis is an infection of the lower urinary tract, usually resulting from a single gram-negative enteric bacteria. (See separate chapters for information on prostatitis, pyelonephritis, and non-gonococcal urethritis.) System(s) affected: Renal/Urologic Genetics: No specific genetic pattern Incidence/Prevalence in USA: Not common Predominant age: Increases with age. Uncommon in men under 50. 8 infections/10,000 men, ages 21-50. Predominant sex: Male only (for this discussion)
Medical Symptoms and Signs of Disease
- Urinary frequency
- Urinary urgency
- Dysuria
- Hesitancy
- Slow urinary stream
- Dribbling of urine
- Nocturia
- Suprapubic discomfort
- Low back pain
- Hematuria
- Systemic symptoms (chills, fever) present with concomitant pyelonephritis or prostatitis
What Causes Disease?
- Escherichia coli (80% of infections)
- Klebsiella
- Enterobacter
- Proteus
- Pseudomonas
- Serratia
- Streptococcus faecalis and Staphylococcus
Risk Factors
- Benign prostatic hypertrophy
- Cognitive impairment
- Fecal incontinence
- Urinary incontinence
- Anal intercourse
- Recent urologic surgery, catheterization
- Infection of the prostate or kidney
- Urinary tract instrumentation
- Immunocompromised host
- Outlet obstruction
Diagnosis of Disease
Differential Diagnosis
- Anatomic or functional pathology
- Urethritis
- Infections in other sites of the genitourinary tract (e.g. epididymis)
Laboratory
- Pyuria
- Bacteriuria
- Urine dipstick leukocyte esterase (75-90%, sensitivity. 95% specificity), and nitrate (35-85% sensitivity, 70% specificity)
- Urine culture — 10/high power colonies of pathogens (or counts > 100,000 bacteria/mL of urine) confirms diagnosis (Escherichia coli, Klebsiella, Pseudomonas. other agents). Lower counts can also be indicative of infection, especially in presence of pyuria.
- Segmented bacteriologic localization cultures
- VB1 — collect 5-10 mL of urine of patient’s initial voiding
- VB2 — then a sample of sterile midstream urine is obtained
- EPS — prostatic massage performed, and expressed prostatic secretion is collected from the meatus
- VB3 — patient completes voiding and 4th sample is collected
- Cultures and sensitivity collected from each specimen
Drugs that may alter lab results: Antibiotics prior to culture Disorders that may alter lab results: N/A
Pathological Findings
Depends on site of infection
Special Tests
Urologic investigations necessary to rule out other disorders
Imaging
Intravenous pyelography, cystoscopy, ultrasound
Diagnostic Procedures
Careful history and physical
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient, except for acute illness with toxicity or kidney failure
General Measures
- Hydration and analgesia if required
- Discontinue sexual activity until cured
- Patient with indwelling catheters
- If asymptomatic bacterial colonization — no need to treat (sterilization of urine not possible and resistant organisms can take up residence)
- If symptomatic of acute infection — institute treatment
Activity
Activity as tolerated.
Diet
No special diet
Medications (Drugs, Medicines)
Drug(s) of Choice
- Acute UTI, first infection, no risk factors for treatment: 7-10 days of oral antibiotics either empirically or based on cultures and sensitivity results. For empiric therapy, trimethoprim-sulfamethoxazole (SMX-TMP) bid will usually treat the most likely pathogens.
- Complicated or recurrent UTI: 14-21 days of antibiotics based on antimicrobial sensitivities with repeat urine check after treatment
Contraindications: Refer to manufacturer’s information Precautions: Refer to manufacturer’s information Significant possible interactions: Refer to manufacturer’s information
Alternative Drugs
According to culture and sensitivity results and patient’s history
Patient Monitoring
Close followup until clinically well and repeat urinalysis after treatment
Prevention / Avoidance
- Prompt treatment of predisposing factors
- Catheter use only when necessary. If needed, use aseptic technique and closed system, with removal as soon as possible.
Possible Complications
- Pyelonephritis
- Ascending infection
- Recurrent infection
Expected Course / Prognosis
Clearing of infections with appropriate antibiotic treatment
Miscellaneous
Associated Conditions
- Acute bacterial pyelonephritis
- Chronic bacterial pyelonephritis
- Urethritis
- Prostatitis
- Prostatic hypertrophy
- Prostate cancer
Age-Related Factors
Pediatric: Usually associated with obstruction to normal flow of urine, such as vesicoureteral reflux Geriatric: Bacteriuria is common in the elderly, appears related to functional status and is usually transient. If asymptomatic bacteriuria is noted, no treatment is needed.
Pregnancy
N/A
Synonyms
- UTI
- Cystitis
International Classification of Diseases
595.0 Acute cystitis 595.1 Chronic interstitial cystitis 595.2 Other chronic cystitis
See Also
- Prostatic cancer
- Prostatitis
- Prostatic hyperplasia, benign (BPH)
- Pyelonephritis





