Description of Medical Condition
Systemic bacterial infection caused by Brucella species in infected animal products, or vaccine. Incubation period usually 5-60 days, but highly variable and may be several months. Characterized by intermittent or irregular fevers, with symptoms ranging from subclinical disease to infection of almost any organ system. Bone and joint involvement common. May be chronic or recurrent. Case fatality untreated less than 2%.
System(s) affected: Endocrine/Metabolic, Gastrointestinal, Renal/Urologic, Pulmonary, Nervous, Skin/Exocrine, Musculoskeletal, Cardiovascular
Genetics: None; some evidence for intrauterine transmission
Incidence/Prevalence in USA:
- About 100/year (105 cases in 1992; 0.34/100,000), but probably underreported
- Common in developing countries; consider in immigrants
- Highest rates in Hispanic population, along US-Mexico border
- Considered a potential biological terror agent in aerosolized form
- Reportable in all states except Nevada
Predominant age: All ages, but especially 20-60 (occupational exposure), sometimes children (milk-related outbreaks)
Predominant sex:
- Male > Female (occupational exposure)
- Female > Male (milk exposure)
Medical Symptoms and Signs of Disease
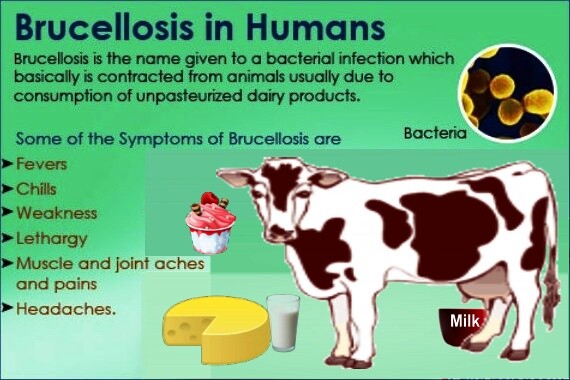
- Fever (may be undulant, increased in afternoon and evening, maximum 101-104° daily); weakness; headache; sweating; chills; generalized aching; arthralgia (90%)
- Also common — weight loss, depression, irritability, hepatosplenomegaly (20-30%)
- Hepatic dysfunction (abnormal liver function test) 30-60%
- Gastrointestinal symptoms (unusual)
- Lymphadenopathy, especially cervical, inguinal (12-21%)
- Orchitis, epididymitis (normal urinalysis) (2-40%)
- Nephritis, prostatitis (rare)
- Cystitis
- Pulmonary — cough or other pulmonary symptoms, x-ray may be normal (15-25%)
- Cutaneous — many transient, non-specific rashes have been described; also, purpura from thrombopenia (5%)
- Visual disturbances, eye pain
- Chronic fatigue syndrome and various neuro-psychiat-ric symptoms described. Unclear relationship.
- Also localized suppurative infections (see Complications)
What Causes Disease?
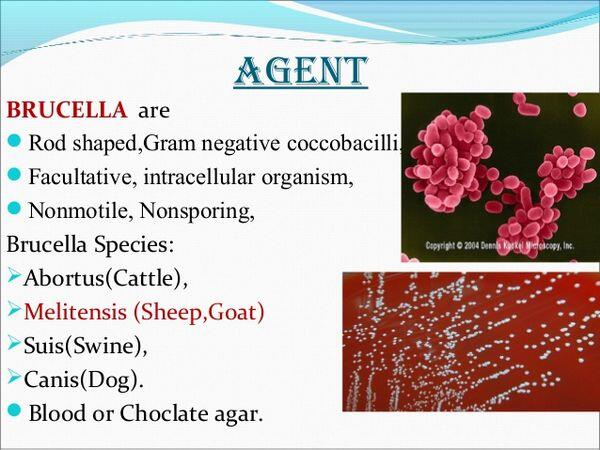
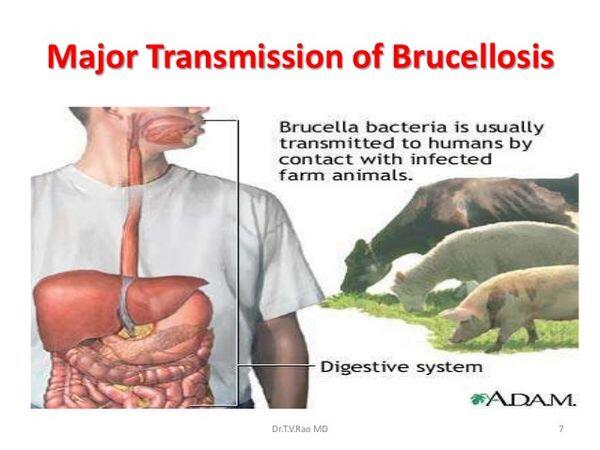
- Brucella ingestion from tissue or milk
- Worst disease: B. melitensis, B. suis; also B. cams, B. abortus. Enter through mucous membrane, broken skin, occasionally inhaled. Facultative intracellular parasite, releases endotoxin when destroyed.
- Person-to-person transmission rare; sexual, vertical, possibly breast milk. Case report of neonatal brucellosis from a blood transfusion
Risk Factors
- In US, from occupational exposure to infected animals (especially cattle, sheep). Veterinarians, meat processors, farm workers; who may experience accidental exposure to vaccine. 18 case outbreak in pork processing plant, 1992.
- Consumer exposure to unpasteurized milk products, cheese
- Exposure while traveling in countries where endemic (Mediterranean, Middle East, N. and E. Africa, central Asia, India, Mexico, Central and South America)
- Worse in chronically ill, immunosuppressed, malnourished
- Iron deficiency increases susceptibility
Diagnosis of Disease
Differential Diagnosis
- Many non-specific systemic febrile illnesses; a great mimic
- Tularemia
- Psittacosis
- Rickettsial disease
- Tuberculosis
- Visceral leishmaniasis
- Other disease of infected organs
- HIV infection
Laboratory
- Isolation of organism from blood, discharge, bone or other tissue. Fastidious and slow-growing. Watch 3-4 weeks, with periodic subcultures. Automated systems shorten time, but not all recognize brucellosis. PCR accurate including non-blood samples, but not available in most clinical labs. Skin tests not standardized, not recommended for diagnosis.
- Acute illness: Blood culture is positive 70%, bone marrow 90%
- May have thrombopenia, disseminated intravascular coagulation; granulopenia, lymphopenia, lymphocytosis. 30-60% with abnormal liver function test. Up to 70% may have normal labs.
- Serology: Brucella standard tube agglutination (STA) paired sera, > 1:160 or 4 x rise (cheapest). Easy, accurate, rapid dipstick for IgM now exists for developing countries.
- More effective ELISA, indirect fluorescent antibody test (IFAT), Coombs tests, immunocapture-agglutination (Brucellacapt). With ELISA, IgM, IgG or IGA may be present at low levels > 1 year even if treated.
- IgM increased initially for several weeks, declines by 3 months
- IgG begins rise 2 weeks, may stay up (low levels) > 1 yr if treated or not treated (though IgM increase may be lower or gone by 6 months if treated, can also persist > 1 year at low levels). IgG titer rises again with reinfection or reactivation. IgG and IGA titer > 1:160 at 1 year implies ongoing disease.
- New research: gene cloning and amplification for discriminatory markers detection and strain differences: PCR-EUSA
Drugs that may alter lab results: None
Disorders that may alter lab results: Serologic cross-reaction with F. tularensis, Yersinia en-terocolitica, V. cholerae, or vaccinated patients. It has been misdiagnosed in culture as Moraxella phenylpyruvica.
Pathological Findings
- Facultative intracellular gram negative coccobacil-lus; can survive inside phagocyte cells, circulate to regional lymph nodes, and into circulation. (Cell-mediated immunity necessary to kill intracellular organism.)
- Macrophages kill, releasing endotoxin that may cause symptoms of acute disease
- Variable tissue reaction depending on site, organisms. Causes local microabscesses; noncaseating granulomas; possibly some immune reaction in arthritis, including elevated C3, C4; ANA, RF.
Special Tests
Echocardiogram depending on location
Imaging
- Bone scan, CT, depending on location
- Chest x-ray — pleural effusion, lung cavitation
- Joint x-rays frequently normal, requiring scan or MRI
Diagnostic Procedures
Biopsy aspiration depending on location
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient in mild cases, hospitalization in severe illness. Cardiac care unit in patients with complicating cardiac
General Measures
- Supportive care
- In milk-related or occupational outbreak, lookfor other cases
Surgical Measures
Specific complications may require surgical drainage, or valve replacement in endocarditis
Activity
Bedrest during febrile periods and restricted activity in acute cases
Diet
No special diet. May need to provide supplemental foods, e.g., milk shakes, to counter weight loss.
Patient Education
Food Safety and Inspection Service, Office of Public Awareness, Department of Agriculture, Room 1165-S, Washington. DC 20205, (202)447-9351
Medications (Drugs, Medicines)
Drug(s) of Choice
- Optimal therapy includes two drugs, at least one with good intracellular penetration. In some cases, 3 drugs may give a better long-term cure. Longer courses (months) may improve relapse rate in complicated disease.
- Rifampin 600-900 mg and doxycycline 200 mg given together every day for at least 6 weeks (possible for several months with severe complications). 5% relapse rate, not related to drug resistance — use same drugs for relapse. Usual cause is localized sequestration of organisms, or noncompliance with medication.
- Steroids in Herxheimer’s reaction, severe illness, pancytopenia
Contraindications: Avoid doxycycline in children, pregnant women
Precautions: May get Herxheimer’s reaction when therapy initiated
Significant possible interactions:
- Rifampin is a potent inducerforthe hepatic P450 enzyme system, and may increase metabolism of many drugs metabolized by the liver
- Doxycycline: Antacids, anticoagulants, barbiturates, carbamazepine, hydantoins, cimetidine, digoxin, insulin, iron salts, lithium, methoxyflurane, oral contraceptives, penicillins, sodium bicarbonate
Alternative Drugs
- In recent studies, ciprofloxacin 1 gm/qd and rifampin 600 mg/day for 30 days as effective as rifampin/doxycycline for 4-5 weeks
- Doxycycline orally bid and streptomycin by injection
- very effective. (Streptomycin currently not available in the USA except by special request from CDC in Atlanta.) Slightly more effective than doxycycline/rifampin, especially with spondylitis, but more toxic and less convenient.
- In children, trimethoprim-sulfamethoxazole (cotrimoxazole) plus rifampin 15 mg/kg (don’t use alone) — higher relapse rate
- In children and pregnant women, rifampin 15 mg/kg for 45 weeks plus: cotrimoxazole for 6 weeks or gentamicin for 7 days or netilmicin 5-6 mg/kg IM. Significant cotrimoxazole resistance in some countries.
- Ofloxacin plus rifampin effective in recent study
- No single drug is effective alone
Patient Monitoring
Check serology at 6 months and 1 year for chronic disease (difficult to evaluate if continuing exposure). Investigate any evidence of complication, recurrence. PCR recently shown sensitive and specific for monitoring treatment relapse.
Prevention / Avoidance
- Avoid infected dairy products
- For occupational exposure — caution, animal vaccination, use of protective goggles, protective gloves. Possible future human vaccine.
- Post-exposure prophylaxis same as treatment in large scale exposure such as bioterrorism
- Susceptible to heat, disinfectant but can survive in dust, soil or water for weeks
Possible Complications
- Relapse (5% overall)
- Localized suppurative infections — osteoarticular (20-85%). Includes arthritis (possibly also immune effect), bursitis, tenosynovitis, osteomyelitis, sacroiliitis. vertebral or paraspinous abscess.
- Endocarditis — rare, but main cause of death in brucellosis
- Thrombophlebitis
- Neuro-brucellosis — most are meningeal. Also peripheral neuritis (usually single, bilateral is possible), encephalitis, myelitis, radiculopathy. Possibly neuro-psychiatric symptoms; a chronic fatigue type syndrome may exist.
- Intrinsic ocular lesions — uveitis, retinal thrombophlebitis, nummular keratitis
- Pneumonitis with pleural effusion
- Hepatitis
- Cholecystitis
- Chronic infection. Persistent (> 1 year) signs of infection, elevated titers, occasional bacteria in blood or tissue. Chronic fatigue syndrome with everything negative is controversial.
Expected Course / Prognosis
- Untreated case fatality < 2%
- Most cases resolve with treatment. 2-3 weeks for acute uncomplicated cases, but at least 6 weeks treatment recommended
- Relapse rate overall, 5%
Miscellaneous
Associated Conditions
N/A
Age-Related Factors
Pediatric: May be mild, subclinical
Geriatric: N/A
Others: Worse in chronically ill, immunosuppressed
Pregnancy
High rates of miscarriage or abortion (can occur in subclinical cases). Early antibiotic treatment is preventive.
Synonyms
- Undulant fever
- Malta fever
International Classification of Diseases
023.9 Brucellosis, unspecified
See Also
Chronic fatigue syndrome Abortion, spontaneous Thrombosis, deep vein (DVT







