Goals of treatment
The goal of antiretroviral therapy is to achieve the maximum suppression of HIV replication (HIV RNA level that is less than the lower limit of quantitation). Secondary goals include an increase in CD4 lymphocytes and an improved quality of life. The ultimate goal is decreased morbidity and mortality.
General approach to treatment of HIV infection
- Regular, periodic measurement of plasma HIV RNA levels and CD4 cell counts is necessary to determine the risk of disease progression in an HIV-infected individual and to determine when to initiate or modify antiretroviral treatment regimens.
- Treatment decisions should be individualized by level of risk indicated by plasma HIV RNA levels and CD4 counts.
- The use of potent combination antiretroviral therapy to suppress HIV replication to below the levels of detection of sensitive plasma HIV RNA assays limits the potential for selection of antiretroviral-resistant HIV variants, the major factor limiting the ability of antiretroviral drugs to inhibit virus replication and delay disease progression.
- The most effective means to accomplish durable suppression of HIV replication is the simultaneous initiation of combinations of effective anti-HIV drugs with which the patient has not been previously treated and that are not cross resistant with antiretroviral agents with which the patient has been treated previously.
- Each of the antiretroviral drugs used in combination therapy regimens should always be used according to optimum schedules and dosages.
- Women should receive optimal antiretroviral therapy regardless of pregnancy status.
- The same principles of antiretroviral therapy apply to both HIV-infected children and adults, although the treatment of HIV-infected children involves unique pharmacologic, virologic, and immunologic considerations.
- Persons with acute primary HIV infections should be treated with combination antiretroviral therapy to suppress virus replication to levels below the limit of detection of sensitive plasma HIV RNA assays.
- HIV-infected persons, even those with viral loads below detectable limits, should be considered infectious and should be counseled to avoid sexual and drug-use behaviors that are associated with transmission or acquisition of HIV and other infectious pathogens.
- An excellent source for information on treatment guidelines can be found at http://www.aidsinfo.nih.gov.
- Treatment is recommended for all HIV-infected persons with symptomatic disease or CD4 lymphocyte counts less than 350 cell/ВµL or plasma HIV RNA greater than 55,000 copies/mL regardless of CD4 count (Table Treatment of HIV Infection: Antiretroviral Regimens Recommended in Antiretroviral-Naive Persons).
Pharmacologic therapy
Antiretroviral Agents
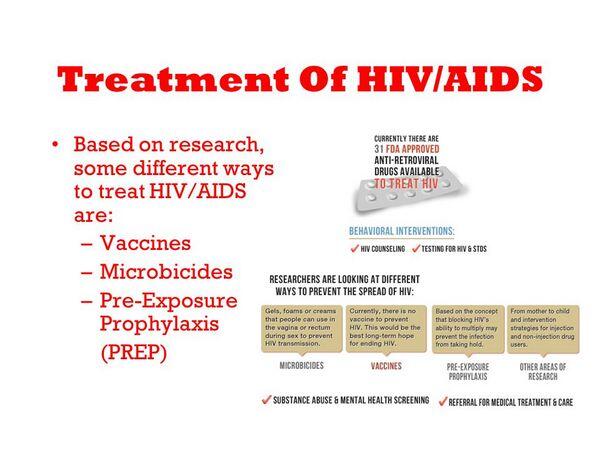
- Inhibiting viral replication with combination of potent antiretroviral therapy has been the most clinically successful strategy in the treatment of HIV infection. There have been three primary groups of drugs used: nucleoside and nonnucleoside reverse transcriptase inhibitors and protease inhibitors .
- Reverse transcriptase inhibitors are of two types: those that are derivatives of purine- and pyrimidine-based nucleosides and nucleotides (Nonnucleoside Reverse Transcriptase Inhibitors) and those that are not nucleoside or nucleotide based (NNRTIs).
- Current recommendations for treating HIV infection advocate a minimum of three antiretroviral agents. The typical regimen consists of two nucleoside analogues with either a protease inhibitor (Protease Inhibitor) or an Nonnucleoside Reverse Transcriptase Inhibitor.
- Significant drug interactions can occur with many antiretroviral agents:
- Amprenavir, Efavirenz, tipranavir, and nevirapine are inducers of drug metabolism, whereas delavirdine and protease inhibitors inhibit drug metabolism.
- Ritonavir is a potent inhibitor of cytochrome P4503A and is used to reduce clearance of other protease inhibitors.
| TABLE. Treatment of HIV Infection: Antiretroviral Regimens Recommended in Antiretroviral-Naive Persons | |||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||
-
- Two Nonnucleoside Reverse Transcriptase Inhibitors, zidovudine and stavudine, antagonize each other’s metabolism and should not be given together.
- Rifampin may substantially reduce the concentrations of PIs
- Saint John’s wort is a potent inducer of metabolism and is contraindicated with PIs and NNRTIs.
Treatment during pregnancy
Therapy during pregnancy is warranted, particularly in light of the dramatic reduction in transmission seen with zidovudine monotherapy. In general, pregnant women should be treated similar to nonpregnant adults; if possible, zidovudine should be used for both mother and infant.
Postexposure prophylaxis
- Postexposure prophylaxis with a triple-drug regimen consisting of two NRTIS and a Protease Inhibitor is recommended for percutaneous blood exposure involving significant risk (i.e., large volume of blood or blood from patients with advanced AIDS).
- Two Nonnucleoside Reverse Transcriptase Inhibitors may be offered to health care workers with lower risk of exposure such as that involving either the mucous membrane or skin. Treatment is not necessary if the source of exposure is urine or saliva.
- Treatment should ideally be initiated within 1 to 2 hours. The optimal duration of treatment is unknown, but at least 4 weeks of therapy is advocated.
| TABLE. Pharmacologic Parameters of Antiretroviral Compounds | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Evaluation of therapeutic outcomes
- Following the initiation of therapy, patients are usually monitored at 3-month intervals with immunologic (i.e., CD4 count), virologic (HIV RNA), and clinical assessments.
- There are two general indications to change therapy: significant toxicity or treatment failure.
- Specific criteria to indicate treatment failure have not been established through controlled clinical trials. As a general guide, the following events should prompt consideration for changing therapy:
- Less than a 1 log10 reduction in HIV RNA 1 month after the initiation of therapy, or a failure to achieve maximal suppression of HIV replications within 4 to 6 months.
- A persistent decline in the CD4 cell count or a return to the pretreatment value or an increase in HIV RNA of 0.3 to 0.5 log10 copies/mL from nadir.
- Clinical disease progression, usually the development of a new opportunistic infection.
Therapeutic failure
- Therapeutic failure may be the result of nonadherence to medication, development of drug resistance, intolerance to one or more medications, adverse drug-drug interactions, or pharmacokinetic-pharmacodynamic variability.
- In general, patients failing their first regimens should be treated with a drug representing a new class. Therapy should be changed to at least two new antiretroviral drugs that are not cross resistant with the agents the patient previously received.







