Essentials of Diagnosis
- Characteristic appearance of yeast and hyphae on KOH preparations.
- Formation of germ tubes in serum is presumptive diagnosis for Candida albicans.
- Cultures must be interpreted with caution because positive culture may represent colonization rather than infection.
- Serology not useful.
General Considerations
Epidemiology
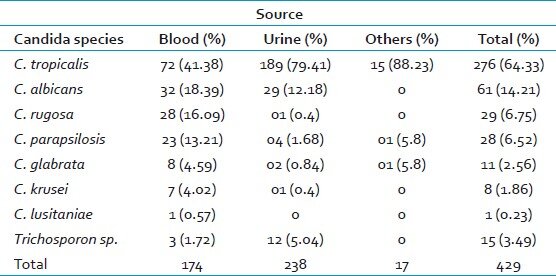
Candida organisms are commensal with humans and, in the absence of alterations in host defense mechanisms, usually do not cause disease. Candida exists as normal flora within the oral cavity, throughout the gastrointestinal (GI) tract, in expectorated sputum, in the vagina, and in the bladder of patients with indwelling catheters. There are >150 species within the genus Candida, although the majority are not known to cause disease in humans. C albicans, C krusei, C glabrata, C tropicalis, C pseudotropicalis, C guilliermondii, C parapsilosis, C lusitaniae, and C rugosa are known human pathogens.
Candida species cause a wide spectrum of clinical diseases that range from mild, superficial infection of the skin and mucous membranes to life-threatening, invasive, multisystem disease. Infection with Candida requires an alteration in the normal milieu that allows the fungus to proliferate and evade host responses.
Under correct conditions, Candida is able to infect any of the body’s mucosal surfaces, as well as the skin. Three-quarters of women report vaginal candidiasis within their lifetime, and the incidence appears to have increased over the last 20 years. Risk factors include recent antibiotic use, pregnancy, oral contraceptive use, diabetes, and human immunodeficiency virus (HIV) infection.
Oral thrush is another frequent manifestation of mucosal candidiasis with similar risk factors to vaginal candidiasis. These risks include systemic disease such as HIV infection or diabetes, inhaled or oral corticosteroid use, and neutropenia induced by chemotherapy.
In addition to the local forms of disease described above, Candida species may cause invasive disease with systemic manifestations and multiple infected organs. Although once limited to the oncology ward and bone marrow transplant unit, candidemia is now more frequent in all areas of the hospital, with Candida the fourth most common organism reported from hospital blood cultures. Specific risk factors for invasive disease include previous isolation of Candida from another site, the use of antimicrobial agents, prolonged neutropenia, indwelling central catheters, and the use of parenteral nutrition.
Although the majority of Candida infections are caused by C albicans, several non-albicans species are emerging as important pathogens and deserve mention. C krusei appears to be less virulent than C albicans and rarely causes disease in the normal host. However, in those with depressed immune function, C krusei is able to cause significant infection. Candidemia, ocular infection, endocarditis, and renal disease all occur with some frequency. C krusei infection has important therapeutic implications as the organism is generally resistant to fluconazole. C glabrata, another Candida species with increasing recovery rates, usually has intermediate resistance to fluconazole.
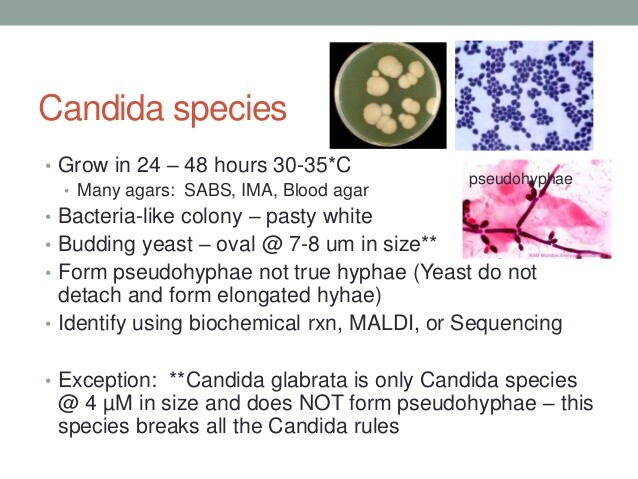
Microbiology
Candida is a fungus that exists primarily in the yeast state, although it may be found in tissue in both yeast and mold forms. The yeast cells are 4-6 um in diameter and reproduce primarily by budding but also by sexual reproduction. In culture, Candida forms smooth white colonies, and a presumptive diagnosis of C albicans can be made by observing the formation of germ tubes within 90 min of placing the organism in serum. Candida will grow on agar plates and in routine blood culture bottles, although the lysis-centrifugation and the BACTEC systems have increased recovery of the organism.
Pathogenesis
As previously mentioned, Candida is part of the normal flora in many areas of the body and, without alteration in host defense, does not cause disease. Factors particularly important to preventing infection are normal bacterial flora, intact skin and mucous membranes within the GI tract, and normal cell-mediated immunity. Alterations of any of the above mechanisms predispose to infection. This is seen clinically as the use of antibiotics (which alter the normal bacterial flora), maceration of the skin, GI surgery, HIV infection, and chemotherapy-induced neutropenia, all of which increase rates of Candida infection.
Candida produces proteins expressed within the cell wall that promote binding and adherence to epithelial cells, endothelium, platelet and fibrin clots, and plastics. These proteins likely help the organism attach to and invade damaged mucosa and may play a role in Candida infection in hosts with indwelling bladder and central venous catheters. Candida species also produce proteases and phospholipases, which may aid the organism in evading host defenses and invading mucosal surfaces.
CLINICAL SYNDROMES
Candiduria, Candida Cystitis & Urinary Tract Candidiasis
Candidemia & Disseminated Candidiasis
CANDIDA ENDOCARDITIS
Endocarditis caused by Candida species has been reported with increasing frequency, particularly after valvular surgery. Other predisposing factors include underlying valvular disease, concomitant bacterial endocarditis, intravenous drug use, intravenous catheters, and chemotherapy. Aortic and mitral valves are commonly infected. The symptoms are similar to that of bacterial endocarditis with fever, malaise, weight loss, and signs and symptoms of embolic phenomena. Splinter hemorrhages, Osler’s nodes, Janeway lesions, hepatosplenomegaly, hematuria, proteinuria, and pyuria may all occur. Candida has the ability to cause large vegetations and large emboli, which may be catastrophic, and valvular lesions may progress to cause perforation, congestive heart failure, and myocarditis (Box 2).
Diagnosis
Blood cultures are generally positive in Candida endocarditis, although negative cultures may occur in up to 25% of patients. Echocardiography reveals vegetations, which may become quite large. Transesophageal echocardiography is more sensitive for detection of vegetations than transthoracic echocardiography. The role of serologic tests (Candida antibodies) is uncertain, as both false positive and false negative results occur with some frequency.
Treatment
Treatment of Candida endocarditis generally requires combined surgical and medical therapy. Once the diagnosis is established, therapy with amphotericin B should be initiated and the valve replaced as soon as possible (Box 8). Antifungal therapy is generally required for a total of 6-10 weeks, and patients should be monitored for a minimum of 2 years after completion of therapy because of the high risk of relapse. For those in whom surgical treatment is not possible, such as those too ill to survive an operation, there exist case reports of treatment success with medical therapy alone (amphotericin B followed by fluconazole).
GI CANDIDIASIS (NONESOPHAGEAL)
Candida species may infect any mucosal surface of the GI tract. After esophageal candidiasis, infection of the stomach is most common. Typically, the organism is seen infecting benign ulcers, although a diffuse mucosal form of infection resembling thrush has been described. In the small and large bowel, ulceration and pseudomembrane formation are common. Mucosal GI involvement may cause deep ulcerations with resulting hemorrhage or perforation (Box 1).
Candida may also infect the peritoneum, liver, spleen, gallbladder, or pancreas. Peritoneal infection is associated with peritoneal dialysis, GI surgery, and GI perforation. Dissemination beyond the abdomen is uncommon. Involvement of the liver, spleen, and pancreas occurs most commonly in immunocompromised hosts, particularly with chemotherapy-induced neutropenia. Often, other manifestations of disseminated candidiasis are present. Fungus balls may form in the gallbladder and biliary tree and cause obstruction. Abscesses may involve the liver and spleen.
Diagnosis
Involvement of nonesophageal mucosal involvement of the GI tract is generally diagnosed by characteristic appearance during endoscopy and by demonstration of Candida by histology or culture of biopsy specimens. Involvement of the peritoneum, liver, spleen, gallbladder, and pancreas may be difficult to diagnose. Fluid returned after peritoneal dialysis may grow Candida in culture. Computer tomography or magnetic resonance imaging may reveal splenic or hepatic abscesses. Laparoscopy may be required for definitive diagnosis.
Treatment
Fluconazole is recommended for initial therapy of mucosal involvement in the stomach, small intestine, or colon (Box 9). Amphotericin B may also be used. Candida peritonitis may also be treated with fluconazole alone or amphotericin B followed by fluconazole. Peritoneal dialysis catheters should be removed if possible. For patients with a perforated viscus, prophylactic therapy is not indicated and should be reserved for those patients with intraoperative findings consistent with Candida infection and positive peritoneal cultures.
Involvement of the liver, spleen, gallbladder, or pancreas should be treated with fluconazole or amphotericin followed by fluconazole. Dosages and duration of therapy are the same as for candidemia and disseminated disease. Large abscesses and fungus balls may require drainage or surgical removal.
OTHER CANDIDA SYNDROMES
Candida species are capable of causing many other infectious syndromes, which will be mentioned briefly. Infection of the respiratory tract may result in bronchopneumonia or diffuse nodular infiltrates. Within the central nervous system (CNS), Candida spp. may cause meningitis and parenchymal abscesses, usually as part of a disseminated infection. Candida spp. have been described as the etiologic agents for osteomyelitis, septic arthritis, myositis, and chostochondritis. Ocular infection may involve any structure within the eye and is common following hematogenous dissemination.
Diagnosis
The diagnosis of Candida infection of the lung, CNS, musculoskeletal system, or eye generally requires demonstration of the organism by tissue culture or on histologic examination. However, visualization of the typical well-demarcated white retinal or vitreal lesion by funduscopic examination in the setting of positive blood cultures is adequate for the diagnosis of Candida endophthalmitis. It should be noted that sputum culture is generally not sufficient for diagnosis of respiratory involvement, particularly in an intubated patient, as the organism may only be colonizing the respiratory tract.
Treatment
Amphotericin B has been the standard treatment for Candida infection in the CNS, eye, lung, and musculoskeletal system. Prosthetic material or other foreign bodies should be removed, if possible. The role of 5-FC is not clear, but it may be added to amphotericin. There is growing support for the use of the azole class, particularly fluconazole, as treatment for deep Candida infection. While case reports of success with fluconazole exist, there are very limited data regarding fluconazole in these settings and virtually no data comparing fluconazole with amphotericin.
Prevention & Control of Candida Infections
Candida species are ubiquitous; thus prevention of disease is best accomplished by elimination of risk factors as opposed to elimination of the organism (Box 10). Antibiotic therapy should be focused to treat specific organisms whenever possible. Indwelling vascular and bladder catheters should be removed as early as possible. In the hospital environment, health care professionals should practice good hand washing to minimize introduction of Candida infection to patients at risk.
The role of prophylactic therapy is unclear but generally not supported. Prophylactic therapy has been shown to reduce mortality in bone marrow transplant patients but not in any other setting. Prophylactic therapy for candidemia may be warranted in patients’ with negative blood cultures who have multiple risk factors for infection and have isolation of Candida from multiple sites but is generally discouraged because of concern for creating resistant organisms. Empiric therapy may also be employed in certain settings, such as neutropenic patients who remain persistently febrile for 7-14 days despite broad spectrum antibiotics and exclusion of other possible causes of infection or in patients with two or more risk factors for invasive Candida infection and isolation of Candida from sputum or urine. Fluconazole is the preferred agent in these settings.
BOX 1. Dermatologic and Mucosal Candidiasis
Dermatitis
Oral
Esophageal
GI (Nonesophageal)
Vulvovaginal
More Common
- Erythematous, macerated skin with scalloped border and satellite lesions
- Typically in warm, moist areas (groin, under breasts)
- Paronychia
- Onychomycosis
- Multiple white patches on tongue, palate, and pharnx that are easily removed with tongue blade, leaving erythematous mucosa
- Asymptomatic
- Dysphagia
- Odynophagia
- Epigastric pain
- Nausea and vomiting
- Hematemesis
- Concurrent oral thrush
- Infection in benign ulcers
- Ulceration and pseudomembrane formation within small and large intestine
- Vulvar pruritus
- Vaginal discharge (may range from thin and white to thick and curdlike)
- Odorless or mild odor
- Vulvar burning
- Dyspareunia
- Exam revealing white plaques on erythematous mucosa
Less Common
- Generalized cutaneous eruption
- Single or multiple 5-10-mm papules1
- Candida granulomas2
- Erythematous mucosa on palate and tongue without white plaques
- Erythema and edema of mucosa of denture wearers
- Adherent white plaques (not removable with tongue blade) on erythematous base
- Stricture
- Perforation
- Diffuse involvement of stomach similar to thrush
- Deep ulceration
- Hemorrhage
- Perforation
1 Part of disseminated candidiasis
2 Typically seen as part of chronic mucocutaneous candidiasis
BOX 2. Deep-Tissue Candida Infection
Urinary Tract
Candidemia and
Disseminated Candidiasis
Endocarditis
More Common
- Asymptomatic
- Patient with risk factors1
- Patient with risk factors2
- Presentation ranges from asymptomatic to septic shock
- Positive blood cultures
- Microabscesses involving multiple organs
- Patient with risk factors3
- Fever, malaise, weight loss
- Embolic phenomena
Less Common
- Dysuria, frequency, urgency
- Pyuria
- Involvement of ureters or renal parenchyma
- Negative blood cultures (does not exclude disseminated disease)
- Valve perforation
- Congestive heart failure (CHF)
- Myocarditis
- Indwelling bladder catheter, diabetes mellitus, systemic antibiotic use.
- Malignancy, neutropenia, organ transplantation, GI surgery, burns, intravascular catheters, broadspectrum antibiotics.
- Valvular surgery, IV drug use, bacterial endocarditis, IV catheters, chemotherapy.
BOX 3. Treatment of Oral Candidiasis
Topical
- Nystatin suspension (100,000 U/mL), 4-6 mL four times per day × 7-10 d
OR
- Clotrimazole troches (10 mg), 4-5 times/d × 7-10 d
- Dentures must be removed and properly cleaned daily
Systemic
- Fluconazole, 100 mg PO every day × 10-14 d
OR
- Itraconazole, 200 mg PO every day × 10-14 d1
1Dose of itraconazole may need to be increased in patients with HIV infection secondary to achlorhydria and decreased absorption.
BOX 4. Treatment of Candida Esophagitis
Topical
- Nystatin suspension (100,000 units/mL) 10-30 mL 4-5 times daily
- Clotrimazole troches (10 mg) 5 times daily
Systemic
- Fluconazole 50-200 mg PO every day × 10 days
- Itraconazole1 50-200 mg PO every day × 10 days
- Amphotericin B 0.3-0.6 mg/kg/day IV × 10 days
Patients with HIV or an acid suppresive therapy may have poor absorption due to high gastric pH.
BOX 5. Treatment of Candida Vulvovaginitis1
Topical
- Butoconazole, 2% cream, 5 g every day × 3 d
- Clotrimazole, 1% cream, 5 g every day × 7-14 d
- Clotrimazole, vaginal tablet, 100 mg every day × 7 d
- Clotrimazole, vaginal tablet, 200 mg every day × 3 d
- Clotrimazole, vaginal tablet, 500 mg every day × 1 d
- Econazole, vaginal tablet, 150 mg every day × 3 d
- Fenticonazole, 2% cream, 5 g every day × 7 d
- Miconazole, 2% cream, 5 g every day × 7 d
- Miconazole, vaginal suppository, 100 mg every day × 7 d
- Miconazole, vaginal suppository, 200 mg every day × 3 d
- Miconazole, vaginal suppository, 1200 mg every day × 1 d
- Nystatin suppository, 100,000 U every day × 14 d
- Terconazole, 0.4% cream, 5 g every day × 7 d
- Terconazole, 0.8% cream, 5 g every day × 3 d
- Terconazole, vaginal suppository, 80 mg every day × 3 d
- Tioconazole, 2% cream, 5 g every day × 3 d
- Tioconazole, 6.5% cream, 5 g every day × 1 d
Systemic
- Fluconazole, 150 mg PO once
- Itraconazole, 400 mg PO once
Women with recurrent infection and no reversible risk factors may require suppressive therapy.
BOX 6. Treatment of Urinary Tract Candidiasis
Asymptomatic Candiduria
- Remove prosthetic material (e.g., urinary catheters)
- No antibiotic therapy required unless patient is diabetic, nuetropenic, transplant recipient, has anatomic abnormalityof GU tract, or is undergoing GU procedure
- Fluconazole 200 mg PO on first day, then 100 mg PO every day × 4 days
- Amphotericin bladder irrigation1
Upper Urinary Tract Infection
- Fluconazole 400-800 mg PO/IV every day2
- Amphotericin B 0.8-1.0 mg/kg/day IV2
- Remove bladder catheters if possible
- Fungus balls or large perinephric abscesses may require surgery
- Rule out disseminated Candidiasis
- Amphotericin 50 mg in 1 liter sterile water infused at 40 mL/hour through continuous infusion/drainage system.
- Treatment continued until clinical improvement, definite resolution of parenchymal involvement, and for 14 days after any positive blood cultures.
BOX 7. Treatment of Candidemia and Disseminated Candidiasis1
Adults
Children
First Choice
- Fluconazole, 400-800 mg PO/IV every day2
- Remove intravascular catheters if possible
- Monitor for evidence of end-organ infection
- Fluconazole, 6 mg/kg twice per day
- Remove intravascular catheters if possible
- Monitor for evidence of end-organ infection
Alternative3
- Amphotericin B, 0.8-1.0 mg/kg/d4 IV with or without 5-FC, 100 mg/kg/d IV
- Amphotericin B, 0.8-1.0 mg/kg/d IV with or without 5-FC (5-FC adjusted to achieve peak level of 40-60 µg/mL)
- Treatment is continued until clinical improvement, definite resolution of parenchymal involvement, and for 14 days after the last positive blood culture.
- Fluconazole, 400 mg daily, is preferred as initial dosage in stable patients.
- Preferred in patient on fluconazole for > 2 days at time of positive blood culture, worsening on fluconazole therapy, unstable (eg, hypotension, mechanical ventilation, etc.), or infection with C. krusei.
- Amphotericin, 0.5-0.7 mg/kg/d IV, may be used as initial dose in stable patient.
BOX 8. Treatment of Candida Endocarditis
- Surgical replacement of valve
- Amphotericin B 0.8-1.0 mg/kg/day IV every day, continued for 6-10 weeks after operation
BOX 9. Treatment of Non-esophageal GI Candidiasis
Mucosal1
- Fluconazole 50-200 mg PO/IV every day × 10 days
- Amphotericin B 0.3-0.6 mg/kg/day IV × 10 days
Liver, Spleen, Gallbladder, Peritoneum
- Fluconazole 400-800 mg PO/IV every day2
- Amphotericin B 0.8-1.0 mg/kg/day IV3
- Stomach, small intestine, large intestine.
- Treatment continued until clinical improvement, definite resolution of parenchymal involvement, and for 14 days after any positive blood cultures.
- Treatment continued as for fluconazole; may change to fluconazole after initial therapy with amphotericin if clinically improved.
BOX 10. Prevention & Control of Candidiasis
Prophylactic Measures
- Candida ubiquitous, therefore cannot eliminate organism
- Eliminate risk factors if possible (indwelling catheters, Total parenteral nutrition [TPN], etc.)
- Good hygiene among health care workers to eliminate spread to those at risk
- Prophylactic therapy generally not indicated; concern for creation of resistant organisms
Isolation Precautions
- Generally not required
Resources
https://www.cdc.gov/fungal/diseases/candidiasis/index.html
https://www.labcorp.com/assets/5136
https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_ABX_Guide/540076/all/Candida_species