STAPHYLOCOCCUS AUREUS
Essentials of Diagnosis
- Large gram-positive cocci (0.7-1.5 um in size).
- Colonies surrounded by zone of hemolysis on blood agar.
- Colonies pigmented pale yellow to deep orange macroscopically.
- Cluster in grapelike bunches microscopically.
- Biochemically differentiated from streptococci by presence of the enzyme catalase.
- Biochemically differentiated from other staphylococci by presence of the enzyme coagulase.
- Analysis of chromosomal DNA can identify clonal isolates (useful in epidemiologic studies).
General Considerations
Epidemiology
Staphylococcus aureus colonizes the human skin, vagina, nasopharynx, and gastrointestinal tract. Colonization occurs shortly after birth and may be either transient or persistent. Published studies differ widely in estimates of the prevalence of S aureus carriage. Between 10% and 35% of healthy adults have transient or persistent nasopharyngeal colonization. This percentage is increased among health care workers and individuals with repetitive needle exposure such as diabetics, patients on hemodialysis, and injection drug users. Vaginal carriage in premenopausal women approaches 10%, with the highest prevalence rates found at the start of the menstrual cycle.
Phage typing and molecular techniques have demonstrated that invasive disease is usually caused by the colonizing strain; therefore it is not surprising that groups with the highest prevalence of colonization are at the highest risk for S aureus infection. Fortunately, progression to infection is relatively unusual, occurring in only 2.5% of colonized nursing home patients and 37% of postoperative patients (compared with 11% of noncolonized postsurgical patients).
Acute infections in noncolonized patients are usually attributed to physical contact with a colonized individual. Studies have proven that health care workers can serve as vectors for transmission of staphylococci. The importance of person-to-person transmission underscores the need for strict hand washing in hospital settings. Other, less common, methods of acquisition include airborne transmission and spread from clothing and bed linens.
Microbiology
Staphylococci are aerobic, nonmotile, gram-positive cocci frequently cultured from environmental and clinical specimens. Although these organisms are generally considered commensal (ie, nonpathogenic normal flora) when cultured from the skin, nasopharynx, intestinal tract, and vagina, they may at times cause life-threatening disease. The clinical interpretation of a culture growing staphylococci depends on the bacterial species, host characteristics, and culture source.
Staphylococci share common characteristics that allow differentiation from other gram-positive cocci (Table 1). All species produce the enzyme catalase. Staphylococci are distinguished microscopically from other gram-positive cocci by a propensity to form clusters, as suggested by the genus name, which comes from the Greek staphule, meaning “bunch of grapes.” Despite these common properties, individual staphylococcal species differ with respect to microbiologic properties, epidemiologic patterns, and clinical manifestations. Many of these differences relate to the production of the enzyme coagulase, and the genus has traditionally been subdivided into S aureus (which is coagulase-positive) and the relatively homogeneous coagulase-negative staphylococci (CoNS).
On blood agar media, S aureus can be distinguished macroscopically from CoNS by a ring of hemolysis surrounding the colonies. Colonies often have a golden-yellow hue (aureus meaning golden in Latin) as a result of the presence of carotenoids. While these morphologic characteristics may serve as general guides for differentiation of S aureus from the CoNS, definitive diagnosis is made by demonstrating the presence of coagulase through agglutination of rabbit plasma.
S aureus possesses a number of properties that contribute to organism virulence and host disease (Table 1): the presence of an extracellular capsule (sometimes called a slime layer), the enzymes catalase and coagulase, and membrane exotoxins that inhibit host immune defenses. More than 70% of strains harbor transmissible plasmids that produce beta-lactamase under certain conditions. These inducible beta-lactamases inactivate penicillin and some first-generation cephalosporins. In addition, an increasing proportion of isolates have intrinsic (as opposed to inducible) resistance to all beta-lactam-containing antibiotics. These strains, known collectively as methicillin-resistant S aureus (MRSA), produce penicillin-binding proteins with low affinity for penicillin, nafcillin, and other beta-lactam drugs. Because antibiotics cannot attach to their target site, the bacteria are not inhibited or killed in the presence of these drugs. Finally, some bacteria produce toxins that damage specific host organ systems such as the gastrointestinal tract (enterotoxins) and dermis (epidermolytic toxins).
Pathogenesis
Much is now known about the process of S aureus infection, which proceeds in a series of steps. Adherence, a necessary condition for colonization, occurs when a bacterium attaches to the teichoic acid component of the host cell wall. Adherence and colonization do not activate the host immune system. Invasion occurs when the epidermis is disrupted through an injury or an iatrogenic procedure, and bacteria gain access to the tissues or bloodstream, activating immune defenses. The interplay between bacterial virulence factors (Table 1) and host susceptibility factors (Table 2) determines whether bacterial proliferation occurs. The final step in the pathogenesis of clinically apparent infection is tissue injury, either localized, as with an abscess, or systemic, as in toxic shock syndrome.
CLINICAL SYNDROMES
S aureus causes a wide spectrum of clinical disease, ranking among the most common bacterial causes of skin and soft tissue infection, gastroenteritis, wound infection, septic arthritis, bacteremia, endocarditis, and osteomyelitis. This section focuses on syndromes unique to S aureus and on syndromes for which S aureus is the most common bacterial agent.
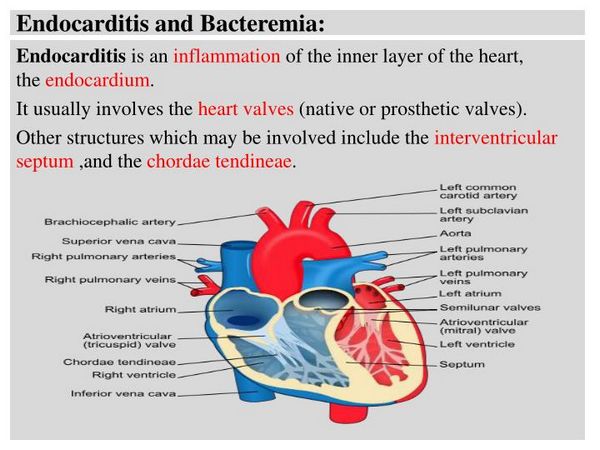
Primary Bacteremia & Endocarditis
COAGULASE-NEGATIVE STAPHYLOCOCCI
Essentials of Diagnosis
- Gram-positive cocci.
- No zone of hemolysis surrounding colonies on blood agar.
- Colonies gray or white macroscopically.
- Cluster in grapelike bunches microscopically.
- Biochemically differentiated from streptococci by production of the enzyme catalase.
- Biochemically differentiated from S aureus by absence of the enzyme coagulase.
- Analysis of chromosomal DNA can identify clonal isolates (useful in epidemiologic studies).
General Considerations
Epidemiology
Like S aureus, coagulase-negative staphylococci (CoNS) are normal human flora. S epidermidis is the most common bacteria cultured from intact skin, while S saprophyticus is commonly cultured from the vagina of asymptomatic women. With the exception of S saprophyticus, which causes cystitis in young, sexually active women, infections with CoNS occur almost exclusively in the presence of foreign bodies.
Microbiology
As with all Staphylococcus species, CoNS are aerobic, nonmotile, gram-positive cocci. This group is comprised of > 30 species, of which about half are known human pathogens. The most clinically important are S epidermidis, S saprophyticus, and S haemolyticus. Although species can be differentiated by biochemical tests, this is rarely clinically indicated, as the high prevalence of methicillin-resistance among CoNS mandates treatment with vancomycin. Molecular analysis can determine if organisms from the same species are clonally related, which may be useful for epidemiologic investigations.
Pathogenesis
Less is known about the mechanisms through which CoNS cause disease. As noted above, adherence, colonization, and invasion occur almost exclusively in the setting of indwelling foreign bodies, such as intravenous catheters or implanted prosthetic devices. CoNS attach to foreign material by the production of an exopolysaccharide slime layer and are able to alter the local immune response through a poorly understood mechanism, hindering host eradication. These organisms are much less virulent than S aureus and generally produce indolent infections with inflammation restricted to local tissues.
BACTEREMIA & ENDOCARDITIS
The rising incidence of CoNS bacteremia in the last decade may be attributed to the increasingly common use of prosthetic devices, especially intravascular catheters, among hospitalized patients. Positive peripheral blood cultures are indicative of infection rather than skin contamination in only 10% of cases, and the challenge lies in differentiating these two entities.
Clinical Findings
Signs and Symptoms
Clinical signs of CoNS bacteremia are often minimal; the finding of fever and leukocytosis support infection rather than colonization, particularly in a host with an indwelling vascular catheter or implanted prosthetic material. While erythema or purulence at a catheter site is compelling evidence supporting catheter-associated bacteremia, only 50% of patients with bacteremia from vascular lines develop local signs of infection.
Although CoNS rarely infect native cardiac valves, they are the most common cause of early (defined as occurring < 12 months postoperatively) prosthetic valve endocarditis (PVE). The majority of cases of early PVE are caused by intraoperative seeding. Infections are indolent, with fever the most common sign. Diagnosis may be delayed by the lack of physical findings specific for endocarditis; most patients do not develop audible murmurs until valve destruction is advanced.
Laboratory Findings
Laboratory abnormalities in CoNS bacteremia and endocarditis are variable. Prosthetic valve endocarditis due to CoNS is usually an indolent process, with nonspecific laboratory findings, including anemia and hematuria. Patients who have CoNS native valve endocarditis present with typical laboratory findings for subacute endocarditis, including elevated erythrocyte sedimentation rate (~90%), anemia (~75%), positive rheumatoid factor (~33%), and hematuria (~33%). Leukocytosis is present in only 40-45% of patients with either bacteremia or endocarditis.
Imaging
Transthoracic echocardiography may be useful in native valve endocarditis or in the later stages of PVE when there is significant valve dehiscence. Diagnosis of PVE may be difficult in the early stages when bacteremia may be intermittent. A diagnosis of PVE is supported by new conduction abnormalities on the electrocardiogram, suggestive of valve ring abscess. The most sensitive technique for diagnosing valvular infection is the transesophageal echocardiogram, which allows excellent visualization of the valve ring and prosthesis.
Differential Diagnosis
A positive blood culture for CoNS represents one of two entities: contamination with skin flora (~90% of cases) or a true infection. The presence of prosthetic biomaterial, either in the form of a temporary indwelling venous catheter or an implanted device, increases the probability of infection as the majority of bloodstream infections are caused by seeding from infected foci. Patients with CoNS bacteremia should have all temporary indwelling catheters removed or replaced, and the tip sent for a semiquantitative culture.
Complications
Hemodynamic instability consistent with septic shock occurs in 10-20% of patients with CoNS bacteremia. Complications of CoNS native valve endocarditis are comparable to those seen with subacute bacterial endocarditis: systemic embolization, valve ring abscess with conduction system disturbance, or congestive heart failure occur in two-thirds of patients, and ~25-50% of patients require valve replacement. Of early PVE cases caused by CoNS, > 85% are complicated by congestive heart failure or prolonged fever despite appropriate antibiotic therapy.
Diagnosis
The diagnosis of CoNS bacteremia or endocarditis is supported by multiple positive cultures from separate venipunctures. Molecular techniques proving clonality of two or more species may argue for true infection (rather than contamination), but access to these tests is generally restricted to research laboratories. In health care settings where molecular testing is not available, the finding of multiple isolates with identical antibiotic susceptibility patterns supports infection rather than contamination. However, the finding of even a single positive culture may be clinically significant and should be interpreted in the context of the patient’s clinical condition.
Treatment
The recommended regimens for CoNS bacteremia are given in Box 7. Although > 70% of CoNS are resistant to PRSPs, beta-lactam resistance is heterotypically expressed, and antibiograms may falsely suggest methicillin sensitivity.
Bacteremia from infected indwelling vascular lines may be cured in > 75% of cases with the catheter remaining intact. Indications for catheter removal include hemodynamic instability, cutaneous tunnel infections, and persistent fever or bacteremia after > 48 h of antibiotic treatment.
A diagnosis of PVE is usually an indication for surgical replacement of the infected valve. A trial of conservative therapy with antibiotics alone may be attempted in hemodynamically stable patients without evidence of congestive heart failure or ring abscess. Treatment requires at least 6 weeks of therapy, with synergistic dosing of gentamicin for the initial 2-week period (Box 7). The clinician should have a low threshold for surgical intervention in patients with persistent fever or bacteremia, or in patients who develop new signs of congestive heart failure. Patients who complete medical therapy should be followed closely after discontinuation of antibiotics, as relapse is also an indication for surgery.
URINARY TRACT INFECTIONS
S saprophyticus is a common cause of uncomplicated urinary tract infection (UTI) in young women, accounting for as many as 15% of all cases of cystitis in this group. There is a seasonal variation in incidence, with the majority of cases occurring in late summer and fall. Risk factors for S saprophyticus UTI include recent sexual intercourse, delayed postcoital urination, and contraception with diaphragm/spermicide combinations.
Clinical Findings
Signs and Symptoms
S saprophyticus causes typical symptoms of cystitis: fever, dysuria, and suprapubic pain. Approximately 20% of women show signs of upper tract disease. It is likely that the number of cases of S saprophyticus pyelonephritis is significantly higher, as localization studies suggest that renal infections may occur in the absence of flank pain.
Laboratory Findings
In uncomplicated pyelonephritis and cystitis, the laboratory findings are restricted to hematuria and pyuria. A Gram stain of centrifuged urine sediment typically reveals gram-positive cocci.
Complications
Complications secondary to S saprophyticus are rare. There have been anecdotal case reports of bacteremia and endocarditis complicating S saprophyticus urinary tract infections. Infection in males, though unusual, is associated with anatomic abnormalities of the urinary tract or urethral catheterization, and ~40% require hospitalization.
Diagnosis
Definitive diagnosis of S saprophyticus UTI is by culture of organisms from a sterile midstream urine collection. A colony count of > 102 bacteria in an appropriate clinical setting (a young woman with symptoms of cystitis) is considered to be diagnostic. However, because cystitis in young women is usually uncomplicated and easily treated empirically, many authorities do not recommend urine cultures and proceed with therapy if microscopy reveals red or white cells in the sediment of a spun urine.
Treatment
S saprophyticus is sensitive to the antibiotics empirically used to treat community-acquired, uncomplicated UTIs (see site). Treatment failures of S saprophyticus UTIs have been reported with single-day therapy (particularly with the fluoroquinolones), leading to the current recommendation of 3 days of antibiotics, regardless of which agent is used. Of note, S saprophyticus is variably sensitive to vancomycin, and this agent should not be used for empiric therapy.
Prevention & Control
Prevention efforts for the ubiquitous methicillin-sensitive S aureus and CoNS have centered around strict aseptic technique for procedures and compulsive attention to hand washing. Intranasal mupiricin may be effective in eradicating S aureus carriage during a hospital outbreak or if epidemiologic investigation implicates a health care worker as a vector for nosocomial infections.
Staphylococcal infection control efforts have concentrated on limiting the nosocomial spread of MRSA (Box 8). Patients colonized or infected with MRSA should be isolated or cohorted, and health care workers should don protective gowns and gloves before patient contact. Hand washing after contact with colonized patients is particularly important as MRSA can survive > 3 h on cutaneous surfaces but is rapidly eradicated by washing with an antibacterial soap. Airborne transmission rarely occurs but is of concern if a patient with respiratory colonization produces copious secretions or requires frequent tracheal suctioning. Both patient isolation and use of masks by contacts is advisable in this setting.
BOX 1. Cutaneous Syndromes Caused by S aureus
Pyogenic
Impetigo
More Common
- Folliculitis
Papules
Pustules
- Furuncles
Abscesses
- Scarlatiniform eruption
- Blisters eroding to honey-colored crust
- Local tenderness
- Regional lymphadenopathy
- Bullous impetigo
Local erythroderma
Flaccid bullae rupturing to brown crust
Involvement of face, trunk, perineum
Less Common
- Carbuncles
Coalescent abscesses with draining fistulae
- Fever
- Systemically ill
- Elevated WBC count
- Fever
- Bacteremia
- Generalized SSS
Diffuse dermal desquamation
Nikolsky’s sign
Fever
Leukocytosis
Bacteremia
Staphylococcal scalded skin syndrome
BOX 2. Empiric Treatment of S aureus Skin Infections
Pyogenic
Impetigo
First Choice
- Folliculitis and furuncles
Local hygiene
I & D of mature furuncles
- Carbuncles
Surgical debridement
PRSP2 1-2 g IV every 4 h for 10-14 days
Pediatric:
Dicloxacillin, 12.5-50 mg/kg/d orally, divided into 4 daily doses OR mupiricin 2% ointment topically 3 times daily3
Adult:
Dicloxacillin 500 mg orally every 6 h for 7 days
- Aggressive hydration
- Close monitoring of fluid status
Pediatric:
PRSP,2 150 mg/kg/d IV, every 6 h for 10-14 days
Adult:
PRSP,2 1-2 gm IV every 4 h for 10-14 days
Second Choice
- Carbuncles
Surgical debridement
Cefazolin, 1-2 g IV every 8 h for 10-14 days
Pediatric:
Cephalexin, 25-50 mg/kg/d orally, divided into 4 daily doses for 7 days
Adult:
Cephalexin, 500 mg orally every 6 h for 7 days
Pediatric:
Cefazolin, 20 mg/kg/d IV every 8 h for 10-14 days
Adult:
Cefazolin, 1-2 g IV every 8 h for 10-14 days
Penicillin Allergic
- Carbuncles
Surgical debridement
Vancomycin, 15 mg/kg/ twice daily for 10-14 days
Pediatric:
Erythromycin, 40 mg/kg/d orally, divided into 4 doses for 7 days
Adult:
Erythromycin, 500 mg orally every 6 h for 7 days
Pediatric:
Vancomycin, 40 mg/kg/d IV divided into 6-h doses
Adult:
Vancomycin, 15 mg/kg/d IV every 12 h for 10-14 days
- Staphylococcal scalded skin syndrome
- Penicillinase-resistant, semisynthetic penicillin—nafcillin or oxacillin
- Topical therapy only indicated for mild, self-limited disease
BOX 3. Treatment of Staphylococcal Toxic Shock Syndrome
Agent/Dose/Route/Duration
Supportive Measures
- Removal of foreign bodies/tampons
- Irrigation of the vaginal vault
- Irrigation and debridement of infected wounds
- Close hemodynamic monitoring
- Vigorous fluid or vasopressor support
- Consider IV gamma-globulin, 400 mg/kg as a single dose
First Choice
- PRSP,2 2 g IV every 4 h for 10-14 days PLUS
- Clindamycin, 900 mg IV every 8 h
Second Choice
- Cefazolin, 1-2 g IV every 8 h for 10-14 days PLUS
- Clindamycin, 900 mg IV every 8 h
Penicillin Allergic PLUS
- Vancomycin, 15 mg/kg IV every 12 h for 10-14 days
- Clindamycin, 900 mg IV every 8 h
- No controlled studies; reserve for life-threatening situations
- Penicillinase-resistant, semisynthetic penicillin—nafcillin or oxacillin
BOX 4. S aureus Native Valve Endocarditis
Right-sided
Left-sided
Common
- Fever
- Leukocytosis
- Heart murmur (~50%)
- Pleuritic chest pain
- Cough
- Hemoptysis
- Dyspnea
- Fever
- Leukocytosis
- Heart murmur (~85%)
- Systemic emboli
- Hemodynamic compromise
- Congestive heart failure
Uncommon
- Hemodynamic compromise
- Congestive heart failure
- Systemic emboli
- Osler’s nodes
- Janeway lesions
- Splinter hemorrhages
- Roth spots
BOX 5. Treatment of S aureus Endocarditis
Scenario
Agent/Dose/Route/Duration
Left-sided Native
Valve Endocarditis
- PRSP, 2 g IV every 4 h for 4-6 weeks PLUS
- Gentamicin, 1 mg/kg IV every 8 h for 3-5 days
Right-sided Native
Valve Endocarditis
- PRSP, 2 g IV every 4 h for 2 weeks PLUS
- Gentamicin, 1 mg/kg IV every 8 h for 2 weeks
Penicillin Allergy
- Cefazolin,3 2 g IV every 4 h for 4-6 weeks PLUS
- Gentamicin, 1 mg/kg IVevery 8 h for 3-5 days OR
- Vancomycin, 15 mg/kg every 12 h for 4-6 weeks
MRSA (Native Valve)
- Vancomycin, 15 mg/kg every 12 h for 4-6 weeks
Prosthetic Valve (PVE)
- PRSP, 2 g IV every 4 h for =6 weeks PLUS
- Rifampin, 300 mg every 8 h for =6 weeks PLUS
- Gentamicin, 1 mg/kg IV every 8 h for 2 weeks
MRSA (Prosthetic Valve)
- Vancomycin, 15 mg/kg every 12 h for =6 weeks
PLUS
- Rifampin, 300 mg every 8 h for =6 weeks PLUS
- Gentamicin, 1 mg/kg IV every 8 h for 2 weeks
- Penicillinase-resistant, semisynthetic penicillin—nafcillin or oxacillin
- 2-week course not indicated if patient unable to tolerate PRSP or if evidence of metastatic disease beside septic pulmonary emboli
- Cephalosporins contraindicated if penicillin allergy is immediate hypersensitivity reaction
BOX 6. Treatment of Osteomyelitis
Children
Adults
General Care
- Debridement of devitalized bone
Methicillin Sensitive
- PRSP,1 150 mg/kg/day IV divided every 6 h FOLLOWED BY2
- Dicloxacillin, 500-100 mg/kg/d orally divided into 4 daily doses
- Treat for 4-6 weeks
- PRSP,1 2.0 gm IV every 4 h
- Treat for 4-6 weeks
MRSA
- Vancomycin, 40 mg/kg/d IV divided every 6 h
- Treat for 4-6 weeks
- Vancomycin, 15 mg/kg every 12 h
- Treat for 4-6 weeks
Penicillin Allergic
- Cefazolin, 20 mg/kg IV every 8 h FOLLOWED BY2,3
- Clindamycin, 30 mg/kg/d orally divided into 4 daily doses OR
- Vancomycin, 40 mg/kg/d IV divided every 6 h
- Treat for 4-6 weeks
- Cefazolin,3 2.0 g IV every 8 h OR
- Vancomycin, 15 mg/kg every 12 h
- Treat for 4-6 weeks
- Penicillinase-resistant, semisynthetic penicillin—nafcillin or oxacillin
- Consider change to oral regimen when WBC count has normalized and ESR is reduced by at least 20%
- Cephalosporins contraindicated if penicillin allergy is immediate hypersensitivity reaction
BOX 7. Treatment of CoNS Bacteremia and Prosthetic Valve Endocarditis
Bacteremia
PV endocarditis
General Care
- Remove indwelling catheters if persistent fever or bacteremia, hypotension, or tunnel infection
- Surgical consult for congestive failure or valve ring abscess
Antibiotic Regimens
- Vancomycin, 15 mg/kg every 12 h
- Treat for 10-14 days
- Vancomycin, 15 mg/kg every 12 h for =6 weeks PLUS
- Rifampin, 300 mg every 8 h for =6 weeks
PLUS
- Gentamicin, 1 mg/kg IV every 8 h for 2 weeks
BOX 8. Nosocomial Control of MRSA
Nasopharyngeal
Colonization
- Single room or cohorting of colonized patients
- Use of gloves for patient contact
- Strict hand washing
Wound/Tracheostomy/
Urinary Tract
Colonization or
Infection
- Single room or cohorting of colonized patients
- Use of gloves for patient contact
- Strict hand washing
- Gown for direct contact
- Dress wounds for hospital transport
- Mask (if aerosolization or splashing likely)
Burns or Extensive Skin Involvement/
Lower Respiratory
Tract Involvement
- Single room or cohorting of colonized patients
- Use of gloves for patient contact
- Strict hand washing
- Gown
- Dress wounds for hospital transport
- Mask (if aerosolization or splashing likely)





