Neisseria gonorrhoeae was first described by Albert Neisser in 1879, in the ocular discharge and exudate from newborn infants with conjunctivitis. Descriptions of a condition resembling the disease gonorrhea can be found in the written record as early as 130 AD, when Galen created a descriptor for the malady by using the Greek words gonos (seed) and rhoea (flow) to characterize what was believed to be the morbid loss of semen. Neisseria meningitidis is thought to be responsible for epidemics in the Napoleonic and Persian armies in the early 1800s. The pathogen was first described in 1886 by Weichselbaum, who observed gram-negative diplococci in the cerebrospinal fluid (CSF) of a young patient who died with purulent meningitis.
Within the family Neisseriaceae, there are five genera — Neisseria, Branhamella, Moraxella, Kingella, and Acinetobacter. N meningitidis and N gonorrhoeae are the organisms that are pathogenic for humans in the Neisseria genus (Table 1). Approximately 10 other Neisseria species have been isolated from humans, but these usually establish a commensal relationship with their host and usually do not cause disease. They lack virulence factors, such as pili and virulence-associated outer membrane proteins (OMPs).
NEISSERIA GONORRHOEAE
Essentials of Diagnosis
- Transmission associated with unprotected sex.
- Purulent urethral discharge, dysuria in men.
- Vaginal discharge, dysuria, intermenstrual bleeding in women.
- Dermatitis-arthritis syndrome with disseminated infection.
- Gram-negative diplococci inside neutrophils on stained smears of urethral, cervical, skin, or joint material.
- Fastidious organism requires special media and growth conditions.
- DNA amplification methods (PCR, LCR) offer improved sensitivity and specificity.
General Considerations
Epidemiology
N gonorrhoeae is found only in humans. It is primarily transmitted sexually by contact with infected secretions. It is the most common reportable infectious disease in the United States, with 300,000-400,000 cases occurring per year — a rate of ~ 130/100,000 persons per year. Chlamydia infections are more common but are not reportable in all states. The incidence of N gonorrhoeae rose during the late 1960s in the United States, peaked in the mid 1970s, and has since declined, but it now may be increasing in certain risk groups such as teenagers. The highest incidence is observed in those 20-24 y of age, in African-Americans, and in lower socioeconomic groups. Most cases are reported in men (male to female ratio, 4:3), which may reflect a greater frequency of symptoms in males. Incidence is higher in men, but prevalence is higher in women. The greatest decline in the prevalence of gonorrhea during the last 15 y has been noted in sexually active gay men, with > 10-fold decreases. This is attributable to safer sex practices in the early wake of the HIV epidemic.
The estimated risk of transmission from an infected female to a male by vaginal intercourse is 20% per exposure. The male-to-female transmission risk is less well studied, but is thought to be ~ 50% per contact. Transmission by rectal intercourse is relatively efficient, although it has not been quantified. Infection can also be transmitted perinatally. High rates of promiscuity are required to maintain a high prevalence of gonorrhea in a population. The so-called “core transmitters” of disease are those who frequently have unprotected intercourse with new partners.
Microbiology
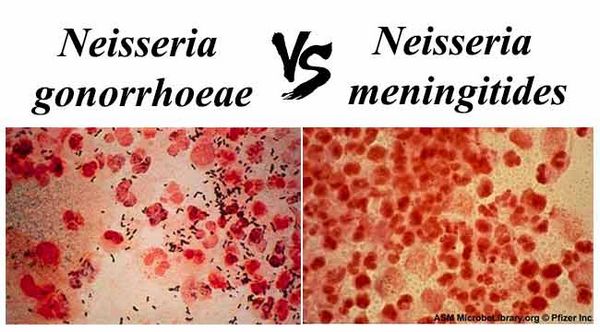
Neisseria species are gram-negative cocci, 0.6-1.0 um in their longest dimension, that usually form pairs (diplococci) with flattened adjacent edges. Their appearance has been likened to kidney beans. Motility is sometimes observed, although they are usually nonmotile. When grown on solid media, gonococci and meningococci form transparent or opaque, mucoid, nonpigmented, nonhemolytic colonies that are 1-5 mm in diameter.
Both N gonorrheae and N meningitidis require specially treated media such as chocolate agar to improve their growth. Chocolate agar is a heme-based growth medium enriched with glucose and other defined supplements; Thayer-Martin medium is chocolate agar with vancomycin, nystatin, and colistin, which inhibit other common commensals, as well as Neisseria species other than gonorrhoeae and meningitidis. Modified Thayer-Martin medium is now commonly used and also contains trimethoprim to inhibit Proteus spp. Growth is optimal at 35-37 °C and requires a carbon dioxide-enriched atmosphere. Fatty acids are toxic to N gonorrhoeae; hence, untreated cotton from some clinical swabs may prevent subsequent growth. Neisseria species are strictly aerobic, but, when nitrate is provided as an electron acceptor, these species can grow anaerobically. Neisseria colonies form within ~ 24-48 h on the solid media mentioned above. Neisseria species are usually identified by their carbohydrate utilization patterns. The principal distinguishing metabolic difference between N meningitidis and N gonorrhoeae is that the latter utilizes maltose. Both can generate acid from glucose. The Neisseria species are classified within the beta subdivision of the division Proteobacteria.
Pathogenesis
N gonorrhoeae has a complex set of molecular mechanisms for invasion and survival in humans. The activation of this complex armamentarium of cellular machinery begins when the pathogen arrives on a mucosal surface. The basic sequence of steps includes (a) long-range attachment by means of pili, (b) close attachment, (c) invasion of mucosal columnar cells, perhaps mediated by porin proteins, (d) transportation through the cell in phagosomes, and (e) occasional “transcytosis” into the submucosa and then, rarely, invasion into the blood stream. Once established in the host, N gonorrhoeae is antigenically heterogeneous, changing its surface structures to avoid host defenses. Several important antigenic structures include pili, porin proteins, opacity (Opa) proteins, reduction-modifiable protein, and lipooligosaccharide (LOS). Pili are the hairlike structures that extend several micrometers from the cell surface and enhance attachment to host cells, as well as help resist phagocytosis. There is great variability in their antigenic structure, through expression of different pilin structural subunit types, as well as variability in expression of different Opa proteins. Gonococci can express several LOS chains simulta- neously, but, unlike lipopolysaccharide from other gram-negative bacteria, the gonococcal LOS does not have long O-antigen side chains. The endotoxic effects of LOS are responsible for the systemic toxicity observed in patients with disseminated disease.
Iron acquisition by N gonorrhoeae at the mucosal surface is a critical requirement for survival and growth. This organism and N meningitidis express receptors on their surface for human lactoferrin and transferrin, to capture iron from the host.
Clinical Findings
Genital infection with N gonorrhoeae most often presents as urethritis in men and cervicitis in women.
Genital Infection in Men
In men dysuria usually precedes development of a urethral discharge, which is creamy, yellow, profuse, and sometimes blood tinged. The incubation period ranges from 1 to 10 d after exposure, but > 90% of men become symptomatic within 5 d. Most untreated cases resolve spontaneously within several weeks. The most common complication of urethral gonorrhea in men is epididymitis. However, N gonorrhoeae causes only 10% of all cases of infectious epididymitis. Other less common complications of genital infection include penile edema, penile lymphangitis, periurethral abscess, and infection of the Cowper’s glands. Stricture of the urethra is now uncommon, but was a more frequent complication in the past.
The microbiological differential diagnosis for urethritis includes other infectious agents such as Chlamydia trachomatis and Ureaplasma urealyticum. Reiter’s syndrome should be considered in patients with urethritis, conjunctivitis, and arthritis. Dysuria and an itching sensation characterize chlamydial urethritis and, in contrast to gonococcal urethritis, may not have profuse purulent discharge. Of men with chlamydial urethral infection, ~ 25% are asymptomatic.
Genital Infection in Women
In women, uncomplicated N gonorrhoeae genital infection is manifest as a purulent cervicitis. Although most women who are seen in acute care settings have symptoms with infection, population-based screening efforts identify many infected women who are asymptomatic. The incubation period in women is less well defined but is ~ 10 d. Symptoms include vaginal discharge, dyspareunia, dysuria without increased frequency, and intermenstrual bleeding. On physical exam, there may be mucopurulent cervical discharge, edema of the cervix, and mucosal friability.
Gonococcal infection in women may progress to involve the uterus and fallopian tubes, causing either acute or chronic salpingitis or pelvic inflammatory disease (PID). Bilateral lower abdominal pain is the most common symptom of PID. There are also signs and symptoms of accompanying lower genital tract infection, as well as cervical-motion tenderness. Fever, leukocytosis, and elevated erythrocyte sedimentation rate or C-reactive protein are common. In PID, anaerobes and chlamydiae may accompany the gonococcal infection. Tubal scarring and infertility are the dreaded sequelae. Perihepatitis (Fitz-Hugh-Curtis syndrome) is a rare complication that occurs by extension of the infection from the fallopian tubes to the peritoneum and the liver capsule. It is accompanied by right upper quadrant tenderness. Laparoscopy demonstrates adhesions between the liver and the parietal peritoneum.
The consequences of gonorrhea during pregnancy include an increased risk of spontaneous abortion, inappropriate rupture of membranes, preterm labor, and fetal mortality. The clinical presentation is essentially the same as that described with genital infection, except that, after the first trimester, PID is less commonly observed because the conceptus obstructs the opening of the uterine cavity. It is unclear whether pregnancy alters the risk for disseminated gonococcal infection.
Anorectal Gonorrhea
Anorectal gonorrhea is observed in ~ 40% of women with genital infection who have receptive anal intercourse and in the same percentage of gay men with genital infection. Only a minority of persons with positive rectal cultures are asymptomatic; in those who are symptomatic, complaints and findings include tenesmus, purulent discharge, pruritus, and rectal bleeding.
Ocular Infection
Gonococcal conjunctivitis occurs by direct inoculation of gonococci into the eye. In adults, this occurs primarily by self-inoculation in persons with active genital infection. In neonates, infection can occur during delivery or postpartum. In adults and neonates, the conjunctivitis is severe, with copious purulent exudate. Corneal ulceration and even blindness can result, especially in the newborn.
Disseminated Gonococcal Infection
Disseminated gonococcal infection results from hematogenous spread of gonococci. It occurs in ~ 3% of infected patients. Arthritis and skin lesions, including pustules and hemorrhagic papules, are the most common manifestations of dissemination (“arthritis-dermatitis syndrome”) and are mediated in part by immune complexes, as well as other indirect immunologic mechanisms. The arthritis most commonly affects the knees, ankles, and wrists. Fever and leukocytosis with polymorphonuclear leukocyte (PMN) predominance are also observed. Cultures of blood or synovium are positive in only about half of all patients with disseminated gonococcal infection, but cultures of mucosal sites are positive in ~ 80% of cases.
Diagnosis
The cornerstone of diagnosis is the Gram stain or culture. One is looking for gram-negative diplococci associated with neutrophils. Gram stain of urethral exudate from men has a sensitivity of 90% and specificity of 98% when compared with culture. Staining of endocervical exudates is 50% sensitive and 95% specific in the hands of an experienced microscopist. Stained smears of the throat or rectum are not helpful because there are confounding flora that make specific diagnosis a challenge. Cultures need not be done for men in the setting of a positive Gram stain, but are indicated for samples from women or in any case in which there is a question of drug resistance. To cultivate the organism, a swab specimen is streaked on enriched selective medium, such as modified Thayer-Martin, and incubated in 5% carbon dioxide at 37 °C. If immediate inoculation with optimal growth conditions is not possible, a transport culture system (ie, JEMBEC) can be used.
In systemic disease, blood culture is necessary. An isolator tube system is preferred. N gonorrhoeae can be cultured from the blood in ~ 30% of cases of gonococcal arthritis. Skin pustule cultures are also useful in defining systemic disease, especially if antibiotic therapy has already been started, because blood cultures will be of lower yield.
Other diagnostic modalities may be used when laboratory culture is not practical or there are specimen transport problems. Assays based on the polymerase chain reaction or ligase chain reaction offer a rapid diagnosis and may offer better specificity and sensitivity than culture; they are becoming more widely available in the United States. Serologic detection of antibodies to gonococcal pili and OMPs by using immunoblotting, radioimmunoassay, or enzyme-linked immunosorbent assay are available for epidemiologic or research purposes but are not clinically useful because of antigenic heterogeneity, the delay in the development of antibody in the setting of acute infection, and the cost.
Treatment
Many antibiotics are safe and effective for the treatment of N gonorrhoeae (Box 1). In choosing a regimen, consideration must be given to the site of infection, other concurrent infections, and the possibility of resistance. The treatment of sex partners is also a crucial consideration in treating any patient with N gonorrhoeae (see Prevention & Control section below). Ceftriaxone in a single dose is the treatment of choice for uncomplicated gonorrhea at all sites. Ciprofloxacin has the advantages of a single oral dose, less expense than ceftriaxone, and effectiveness in patients who are intolerant of cephalosporins; however, resistance has been observed with ciprofloxacin, and it is not active against Treponema pallidum.
Complicated infections or disseminated gonococcal infections, such as arthritis, perihepatitis, or bacteremia resulting in petecchial or pustular skin lesions, require a higher dose of antibiotics than uncomplicated gonorrhea infections and a longer duration of therapy. These regimens should be continued for 24-48 h after clinical improvement is noted (ie, they become afebrile, or joint erythema or skin lesions improve) and then switched to an oral regimen for a total of 7 d. Patients with gonococcal meningitis or endocarditis require higher doses and longer duration of therapy. Meningitis is treated with ceftriaxone for 14 d. Endocarditis should be treated for = 4 wk.
Concurrent infection with C trachomatis is estimated to occur in 40% of those infected with N gonorrhoeae. Therefore doxycycline or azithromycin must be added to the antigonococcal regimen. In pregnant women, for whom doxycycline is contraindicated, an erythromycin base can be used. If erythromycin cannot be tolerated, amoxicillin for 7-10 d is indicated.
Antibiotic resistance has been a major concern, as penicillin resistance has spread and, more recently, fluoroquinolone resistance has been increasingly reported. Beta-lactams remain the drugs of choice in most instances. Antibiotic resistance occurs by one or more mechanisms, including chromosomal mutations leading to decreased penicillin-binding-protein affinity, decreased outer membrane permeability, or beta-lactamase production.
Prevention & Control
The primary measures for prevention of gonorrhea include sexual abstinence and barrier methods with sexual intercourse (“safer sex”) (Box 2). Once a case of gonorrhea is identified, treatment of sex partners is an essential element of control of the disease. Epidemiologic treatment refers to the treatment of contacts of patients after a history of exposure to the disease, but without confirmation of infection. This is done in situations in which the risk of unnecessary treatment is outweighed by the risk of developing complications of the infection or the probability of transmission to other contacts. The prevention of gonorrhea must also be considered in sexual assault cases, and antigonococcal medications are included in the recommendations for treatment.




