The optimal time to initiate antiretroviral therapy in asymptomatic patients is unclear.
A decision to initiate antiretroviral therapy in an HIV-infected adult or adolescent who is asymptomatic should be made after considering the patient’s willingness to begin antiretroviral therapy; the prognosis for disease-free survival in the absence of treatment as determined by baseline CD4+ T-cell count, plasma HIV-1 RNA level, and the rate of decline in CD4+ T-cell counts; and the potential benefits and risks of antiretroviral therapy.
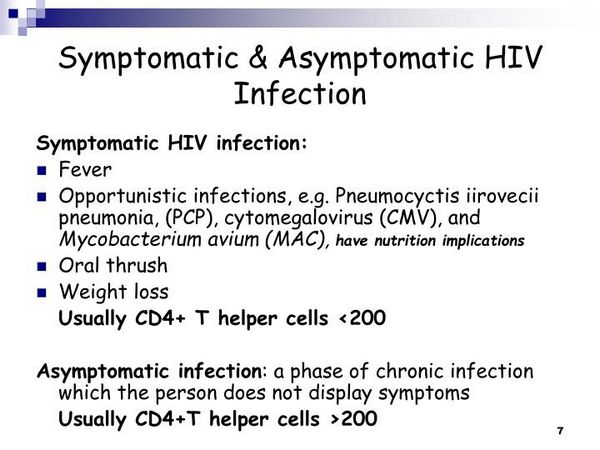
Because observational data and data from clinical studies indicate that the risk of opportunistic diseases increases markedly when CD4+ T-cell counts decrease to less than 200/mm3, most clinicians recommended that antiretroviral therapy be initiated in all asymptomatic adults with AIDS who have CD4+ T-cell counts less than 200/mm3, regardless of plasma HIV-1 RNA levels.
However, there are 2 general approaches to initiating antiretroviral therapy in asymptomatic patients with CD4+ T-cell counts exceeding 200/mm3: a therapeutically more aggressive approach that involves initiating antiretroviral therapy early in the course of the infection and a therapeutically more cautious approach that may involve delaying initiation of therapy.
Theoretical benefits of early initiation of antiretroviral therapy in asymptomatic HIV-infected adults include easier control of viral replication and mutation and reduction in viral burden; prevention of progressive immunodeficiency and potential maintenance or reconstruction of a normal immune system; delayed progression to AIDS and prolongation of life; decreased risk of selection of resistant HIV variants; and possible decreased risk of viral transmission.
Potential risks associated with early initiation of antiretroviral therapy include reduction in quality of life because of adverse drug effects and inconvenience of current maximally suppressive multiple-drug regimens; earlier development of drug resistance if viral suppression is suboptimal; limitations on antiretroviral agent choices that can be used in future regimens because of development of resistance; unknown long-term toxicity associated with antiretroviral regimens; risk of transmission of HIV-1 resistant to antiretroviral agents; and unknown duration of effectiveness of current antiretroviral therapies.
Potential risks associated with delayed initiation of antiretroviral therapy include the possibility that irreversible damage to the immune system may occur that might otherwise be salvaged by earlier therapy; greater difficulty in suppressing viral replication; and increased risk of HIV transmission to others during a longer untreated period.
Increasing recognition of the risks associated with initiation of antiretroviral therapy has resulted in more clinicians supporting the more conservative approach to initiating antiretroviral therapy in asymptomatic patients.
Based on the relationship between viral load, CD4+ T-cell count, and rates of disease progression, the Panel on Clinical Practices for Treatment of HIV Infection and other experts state that, in general, antiretroviral therapy should be offered to asymptomatic HIV-infected adults with CD4+ T-cell counts less than 350/mm3, regardless of plasma HIV-1 RNA level.
The recommendation is based in part on the substantial short-term risk of disease progression for untreated patients with CD4+ T-cell counts less than 350/mm3 at all plasma HIV-1 RNA levels. In addition, data from observational cohorts suggest that initiation of antiretroviral therapy when CD4+ T-cell counts are less than 200/mm3 is associated with shorter survival compared with initiation of therapy at higher CD4+ T-cell counts and that initiation of therapy at CD4+ T-cell counts exceeding 350/mm3 was associated with a higher rate of AIDS-free survival at 2 years compared with deferred therapy.
The Panel on Clinical Practices for Treatment of HIV Infection states that some experts recommend initiating antiretroviral therapy in asymptomatic adults with CD4+ T-cell counts exceeding 350/mm3 and plasma HIV-1 RNA levels exceeding 55,000 copies/mL (by bDNA or RT-PCR) since the 3-year risk of developing AIDS in these untreated patients is greater than 30%; however, other experts would use a more conservative approach and defer antiretroviral therapy in these patients (with close monitoring of CD4+ T-cell counts). In asymptomatic adults with CD4+ T-cell counts exceeding 350/mm3 and plasma HIV-1 RNA levels less than 55,000 copies/mL (by bDNA or RT-PCR), many experts would defer therapy with close observation since the 3-year risk of developing AIDS in untreated patients is less than 15%.
Recommendations regarding when to initiate antiretroviral therapy based on plasma HIV-1 RNA levels generally are the same for both women and men. There is some evidence that there may be differences in viral load and CD4+ T-cell count responses between men and women at different stages of HIV infection; however, data have been conflicting and additional study is needed. Some data suggest that plasma HIV-1 RNA levels may be lower in women than men during early HIV infection at the time of seroconversion, but this difference has not been consistently observed and may disappear as the disease progresses over the next 5-6 years.
Some data from HIV-seronegative individuals indicate that mean CD4+ T-cell percentages and counts generally are higher in women than in men and some data from HIV-infected individuals indicate that the rate of decline in CD4+ T-cell counts may differ between men and women. The clinical importance of the possible differences in these surrogate markers between men and women is unclear, but it has been suggested that men and women have similar rates of disease progression when matched for plasma HIV-1 RNA levels and CD4+ T-cell counts.
In patients with CD4+ T-cell counts less than 350/mm3, sex-based differences in viral load are small and some experts suggest that no change in recommendations for initiation of antiretroviral therapy is necessary for women in this group. Although some clinicians may wish to consider using lower threshold plasma HIV-1 RNA levels to initiate antiretroviral therapy in women with CD4+ T-cell counts exceeding 350/mm3, data are insufficient to determine such a threshold.
If antiretroviral therapy is deferred in an HIV-infected adult who is asymptomatic, the patient should be monitored carefully for signs of disease progression; plasma HIV-1 RNA levels should be measured about every 3-4 months and CD4+ T-cell counts repeated about every 3-6 months.
If antiretroviral therapy is initiated in an HIV-infected adult who is asymptomatic, a regimen that is expected to achieve sustained suppression of plasma HIV-1 RNA levels, sustained increase in CD4+ T-cell count, and a favorable clinical outcome (i.e., delayed progression to AIDS and death) should be selected with additional consideration given to issues that may affect compliance. The Panel on Clinical Practices for Treatment of HIV Infection strongly recommends use of a regimen that includes HIV protease inhibitors (indinavir, nelfinavir, ritonavir and indinavir, ritonavir and saquinavir, lopinavir and ritonavir) or efavirenz in conjunction with 2 NRTIs (stavudine and lamivudine, stavudine and didanosine, zidovudine and lamivudine, zidovudine and didanosine) for these patients.
Advanced HIV Disease
Antiretroviral therapy generally should be initiated in all HIV-infected patients diagnosed with advanced HIV disease (regardless of plasma HIV-1 RNA levels) and in those who are symptomatic (recurrent mucosal candidiasis, oral hairy leukoplakia, chronic and unexplained fever, night sweats, wasting) using the most potent antiretroviral regimen available. The preferred regimens for initial antiretroviral therapy in individuals with advanced HIV infection probably are 3- or 4-drug regimens that include 2 NRTIs and 1 or 2 HIV protease inhibitors or a 3-drug regimen of 2 NRTIs and efavirenz.
HIV-infected individuals with advanced infection often are acutely ill with opportunistic infections or other complications of HIV (e.g., anorexia, wasting) that may impact the timing of initiation of antiretroviral therapy and the choice of antiretroviral agents to include in the regimen.
There may be concerns relating to possible drug interactions or overlapping toxicities that need to be addressed (e.g., pharmacokinetic interactions between antiretroviral agents and antituberculosis agents) or concerns relating to the patient’s ability to adhere to the antiretroviral regimen. Initiation of antiretroviral therapy in individuals with advanced HIV infection often is associated with some degree of recovery of immune function and those who have subclinical opportunistic infections such as Mycobacterium avium complex (MAC) or cytomegalovirus (CMV) may develop a new immunologic response to the pathogen and new symptoms related to these infections. However, this should not be interpreted as a failure of the antiretroviral regimen.
Viral load measurement may be useful in clarifying these situations. Unless there are concerns regarding drug toxicity, intolerance, or drug interactions, the antiretroviral regimen should be maintained and should not be discontinued while an acute opportunistic infection or malignancy is being treated.
Acute HIV Infection
Although initiation of antiretroviral therapy during primary (acute) HIV infection has been controversial because of the limited clinical trial data available evaluating antiretroviral therapy in these patients, most experts now recommend treatment of acute HIV infection based on theoretical considerations and the limited, but supportive, clinical trial data.
Symptoms of Acute HIV Infection
Primary (acute) HIV infection has been defined as the period of time between initial exposure to and infection with HIV and seroconversion; this period can last from 1 week up to about 3 months. While some individuals with acute infection may be asymptomatic, it has been estimated that 40-90% of individuals acutely infected with HIV will experience at least some symptoms of the acute retroviral syndrome.
The associated signs and symptoms of acute retroviral syndrome include fever, fatigue, lymphadenopathy, pharyngitis, rash (erythematous maculopapular with lesions usually on face and trunk and sometimes on extremities including palms and soles), myalgia or arthralgia, diarrhea, headache, nausea and vomiting, night sweats, hepatosplenomegaly, weight loss, thrush, and neurologic symptoms (meningoencephalitis or aseptic meningitis, peripheral neuropathy or radiculopathy, facial palsy, Guillain-Barre syndrome, brachial neuritis, cognitive impairment or psychosis).
The duration of acute symptoms usually is less than 2 weeks. Acute HIV infection often is not recognized in the primary care setting because of similarities with flu symptoms or other common illnesses, and clinicians should maintain a high level of suspicion for HIV infection in all patients presenting with a compatible clinical syndrome.
Rationale for Treatment of Acute HIV Infection
Current knowledge about the pathogenesis of HIV infection indicates that acute HIV infection is associated with high viral load and rapid viral replication. Plasma HIV-1 RNA levels present during primary infection can exceed 105 to 107 copies/mL, and it has been estimated that the number of virions produced during a 1-month period of primary infection approximates the number of virions produced over several subsequent years of asymptomatic infection.

Initiation of antiretroviral therapy during primary infection when the HIV population is rapidly replicating and relatively homogeneous theoretically has the potential to suppress the initial burst of viral replication and decrease the magnitude of virus dissemination throughout the body; decrease the severity of acute disease; result in a low viral load at the time of seroconversion (viral set-point) which could improve the subsequent clinical course of the infection; reduce the risk of viral mutation due to the suppression of viral replication; reduce the risk of viral transmission; and preserve or restore immune function.
There is some evidence that those who have low plasma HIV-1 RNA levels after seroconversion experience substantially slower disease progression than those who have high plasma HIV-1 RNA levels after seroconversion. However, it is unclear whether early initiation of antiretroviral therapy during primary infection would decrease or increase the risk of viral mutation and development of drug resistance or limit future treatment options.
The long-term benefits of initiating antiretroviral therapy in the earliest stages of HIV infection and the possible effects this strategy could have on the body’s initial immune response to the virus are unknown. Without antiretroviral therapy, plasma HIV-1 RNA levels often decrease substantially and may become undetectable after the acute phase of the infection; however, virus is still active in lymph nodes or other reservoirs, and the low level of viremia is temporary. Preliminary data suggest that initiation of potent multiple-drug antiretroviral therapy at the time of primary infection has a beneficial effect on surrogate markers of disease progression and clinical outcome; studies are ongoing to determine the long-term clinical benefit of such a strategy.
Recommendations for Treatment of Acute HIV Infection
Based on the theoretical benefits and limited, but supportive, clinical trial data, most experts currently recommend that antiretroviral therapy be initiated in all patients diagnosed with acute HIV infection. However, the possible benefits should be weighed against potential risks in these patients, including adverse effects on quality of life from drug toxicities and dosing constraints, the potential for development of drug resistance if therapy fails to effectively suppress viral replication and the possibility that this would limit future treatment options, and the potential need for continuing antiretroviral therapy indefinitely.
A diagnosis can be established by the presence of plasma HIV-1 RNA in an individual with a negative or indeterminate test results for HIV antibody. Viremia occurs after infection prior to the detection of a specific immune response, and an indeterminate antibody test may occur when an individual is in the process of seroconversion.
While the presence of HIV p antigen in plasma also can be used to establish the diagnosis (e.g., when plasma HIV-1 RNA testing is unavailable), a negative p antigen test does not exclude the possibility of acute HIV infection. Testing for plasma HIV-1 RNA is recommended whenever there is a high suspicion of acute HIV infection (e.g., in patients with recent risk behavior in association with symptoms of acute antiretroviral syndrome) However, the fact that there may be low titer (less than 10,000 copies/mL) false-positive test results should be considered.
If a decision is made to initiate antiretroviral therapy during primary HIV infection, therapy should be started as soon as possible after the patient is diagnosed with acute retroviral syndrome. The goal of antiretroviral therapy in these patients is suppression of plasma HIV-1 RNA to levels below the limits of detection, and any regimen that is not expected to maximally suppress viral replication is not considered appropriate for treating individuals with acute HIV infection.
Optimum regimens for the treatment of acute HIV infection have not been determined; however, potential regimens are the same as those recommended for patients with established HIV infection. Some clinicians recommend use of 3-drug regimens that include 2 NRTIs and an HIV protease inhibitor.
Once antiretroviral therapy is initiated in a patient with acute HIV infection, many experts suggest that it probably should be continued indefinitely (even after plasma HIV-1 RNA levels are undetectable) since viremia has been documented to reappear or increase if antiretroviral therapy is discontinued. However, there are no clinical trial data to date to demonstrate the superiority of this approach.







