Demeclocycline Hydrochloride, Doxycycline Calcium, Doxycycline Hyclate, Doxycycline Monohydrate, Minocycline Hydrochloride, Oxytetracycline, Tetracycline, Tetracycline Hydrochloride
Tetracyclines are antibiotics and semisynthetic antibiotic derivatives obtained from cultures of Streptomyces.
Dosage and Administration
Administration
Tetracyclines, in appropriate dosage forms, are administered orally, IV, or by deep IM injection. IV or IM administration should be used only when the oral route is not feasible, and oral therapy should replace parenteral therapy as soon as possible. IM administration of tetracyclines is rarely indicated because this route of administration is painful and, in the usual dosage, produces lower serum concentrations than does oral administration. If the drugs are given IV, the risk of thrombophlebitis should be considered. Because food and/or milk reduce GI absorption of demeclocycline and tetracycline, these drugs should be administered orally 1 hour before or 2 hours after meals and/or milk. Doxycycline and minocycline may be given orally with food and/or milk without a clinically important reduction in GI absorption.
Dosage
The duration of tetracycline therapy depends on the type of infection. Generally, therapy should be continued for a minimum of 24-48 hours after the patient becomes asymptomatic or evidence of eradication of the infection has been obtained.
Dosage in Renal Impairment
With the exception of doxycycline, doses and/or frequency of administration of tetracyclines must generally be modified in response to the degree of renal impairment.
Drug Interactions
Because tetracyclines readily chelate divalent or trivalent cations (see Chemistry and Stability: Stability), concurrent oral administration of other drugs containing these cations may decrease absorption of oral tetracyclines and vice versa.
Antacids containing aluminum, calcium, or magnesium and laxatives containing magnesium impair the absorption of oral tetracyclines and should be given 1-2 hours before or after the anti-infective. Oral iron preparations also interfere with GI absorption of tetracyclines, leading to decreased serum concentrations of both the anti-infective and iron. Concurrent administration of an oral iron preparation and an oral tetracycline reportedly results in a 30-90% decrease in absorption of the tetracycline. In one study, oral ferrous sulfate also reportedly decreased the serum half-life of a single IV dose of doxycycline as the hyclate, presumably by interfering with intestinal reabsorption of the anti-infective. If simultaneous administration of an oral iron preparation and a tetracycline is necessary, the tetracycline should be given 3 hours after or 2 hours before the oral iron preparation. In one study, concomitant administration of oral zinc sulfate impaired absorption of oral tetracycline hydrochloride but had no effect on the absorption of oral doxycycline.
Drugs Affecting GI pH
In one study, oral sodium bicarbonate decreased absorption of oral tetracycline hydrochloride when the anti-infective was administered as capsules but had no appreciable effect on absorption when tetracycline hydrochloride was dissolved in water prior to oral administration. In another study, concurrent administration of sodium bicarbonate had no effect on the rate or extent of absorption of tetracycline hydrochloride administered as capsules. Although concurrent administration of oral cimetidine and tetracycline hydrochloride capsules resulted in slightly decreased serum concentrations of the anti-infective in one study, other studies have shown that serum concentrations of tetracycline hydrochloride are not appreciably affected by concurrent administration of oral cimetidine.
Oral Anticoagulants
Oral, IM, or IV tetracyclines reportedly may potentiate the effects of oral anticoagulants either by impairing utilization of prothrombin or by decreasing vitamin K production by intestinal bacteria. Prothrombin times should be monitored more frequently than usual in patients receiving concomitant tetracycline and oral anticoagulant therapy, and dosage of the anticoagulant should be adjusted as required. Tetracyclines have also been reported to interfere with the anticoagulant effect of heparin; however, this interaction has not been substantiated and special precautions are probably unnecessary.
Anti-infective Agents
Tetracyclines have been reported to antagonize the bactericidal activity of aminoglycosides and penicillins in vitro, and the manufacturers and some clinicians recommend that the drugs not be used concomitantly. There have been rare reports of in vivo antagonism when IV tetracyclines were used with IM penicillin in the treatment of pneumococcal meningitis; however, oral tetracyclines have been administered in conjunction with penicillin or streptomycin for other indications with no apparent decrease in activity. Although tetracyclines are inactive against fungi when used alone, preliminary in vitro studies indicate that tetracyclines may exert a synergistic effect with amphotericin B against yeast.
Other Drugs
Antidiarrhea agents containing kaolin and pectin or bismuth subsalicylate reportedly impair absorption of oral tetracyclines, and concurrent use probably should be avoided if possible. In patients receiving tetracycline hydrochloride in multiple-drug regimens including bismuth subsalicylate for the treatment of Helicobacter pylori infection and associated duodenal ulcer, the clinical importance of an anticipated reduction in tetracycline systemic absorption is unknown as the relative contribution of systemic versus local antimicrobial activity against H. pylori has not been determined.
Barbiturates, phenytoin, and carbamazepine decrease the serum half-life of doxycycline. Serum concentrations of demeclocycline, oxytetracycline, and tetracycline are not affected by concomitant administration of barbiturates, phenytoin, or carbamazepine and are preferred when a tetracycline is indicated in a patient receiving one of these drugs. In one patient stabilized on lithium carbonate, concurrent administration of oral tetracycline hydrochloride resulted in increased serum concentrations of lithium and lithium toxicity. Concurrent use of tetracyclines can reduce the effectiveness of oral contraceptives.
When administered concurrently with an oral contraceptive containing estrogen, tetracycline hydrochloride apparently decreased the effectiveness of the contraceptive in one patient resulting in pregnancy and caused breakthrough bleeding in another.
Patients should be advised to use a different or additional form of contraception during tetracycline therapy. (See Pregnancy, Fertility, and Lactation.) Preoperative or postoperative administration of tetracyclines to patients undergoing methoxyflurane anesthesia may produce fatal nephrotoxicity, and concurrent use of the drugs should be avoided.
Laboratory Test Interferences
Tests for Urinary Glucose
Although tetracyclines have reportedly caused false-positive results in urine glucose determinations using the cupric sulfate method (Benedict’s reagent, Clinitest®), this effect may have been caused by ascorbic acid which is included in parenteral preparations of tetracyclines. Tetracyclines also reportedly cause false-negative results in urine glucose determinations using glucose oxidase reagent (e.g., Clinistix®, Tes-Tape®).
Other Laboratory
Tests Tetracyclines generally interfere with fluorometric determinations of urine catecholamines resulting in falsely increased values.
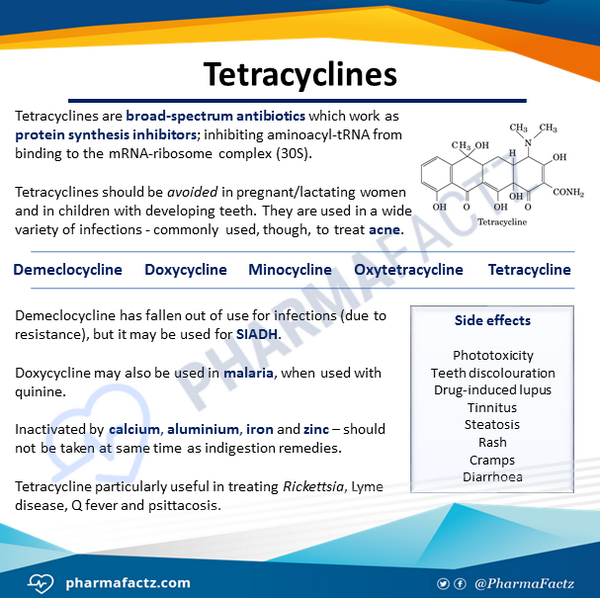
Mechanism of Action
Antibacterial Effects
Tetracyclines are usually bacteriostatic in action, but may be bactericidal in high concentrations or against highly susceptible organisms. Tetracyclines appear to inhibit protein synthesis in susceptible organisms mainly by reversibly binding to 30S ribosomal subunits, thereby inhibiting binding of aminoacyl transfer-RNA to those ribosomes. In addition, tetracyclines appear to reversibly bind to 50S ribosomal subunits. There is preliminary evidence that tetracyclines also alter cytoplasmic membranes of susceptible organisms resulting in leakage of nucleotides and other intracellular components from the cell. At high concentrations, tetracyclines also inhibit mammalian protein synthesis.
Effects on Acne
The exact mechanisms by which tetracyclines reduce lesions of acne vulgaris have not been fully elucidated; however, the effect appears to result in part from the antibacterial activity of the drugs. Following oral administration, the drugs inhibit the growth of susceptible organisms (mainly Propionibacterium acnes) on the surface of the skin and reduce the concentration of free fatty acids in sebum. The reduction in free fatty acids in sebum may be an indirect result of the inhibition of lipase-producing organisms which convert triglycerides into free fatty acids or may be a direct result of interference with lipase production in these organisms.
Free fatty acids are comedogenic and are believed to be a possible cause of the inflammatory lesions (e.g., papules, pustules, nodules, cysts) of acne. However, other mechanisms also appear to be involved because clinical improvement of acne vulgaris with oral tetracycline therapy does not necessarily correspond with a reduction in the bacterial flora of the skin or a decrease in the free fatty acid content of sebum. In an in vivo study, oral administration of demeclocycline or tetracycline hydrochloride suppressed the local inflammatory response (e.g., erythema, pustules) to patch tests with 40% potassium iodide.
Tetracycline hydrochloride also inhibited leukocyte chemotaxis in an in vitro study. It has been hypothesized that these effects could be other mechanisms by which tetracyclines suppress the inflammatory lesions of acne vulgaris.
Spectrum
Tetracyclines have a broad spectrum of activity and are active against most Rickettsia, Chlamydia, Mycoplasma, spirochetes, and many gram-negative and gram-positive bacteria. The drugs are inactive against fungi and viruses. In general, susceptible Rickettsia, Chlamydia, Mycoplasma, and bacteria are inhibited in vitro by demeclocycline, doxycycline, minocycline, oxytetracycline, or tetracycline concentrations of 0.1-5 mcg/mL. Minocycline and, to a lesser extent, doxycycline are more active in vitro against most susceptible organisms than are other currently available tetracyclines and slightly lower concentrations of these derivatives may be required to inhibit most susceptible organisms. In addition, minocycline is active against some bacteria including Acinetobacter, Enterobacteriaceae, and Staphylococcus aureus resistant to other currently available tetracyclines.
In Vitro Susceptibility Testing
Many factors such as inoculum size, pH, and test media can influence results of in vitro susceptibility tests of the tetracyclines. Results of in vitro susceptibility testing with tetracycline generally can be applied to all currently available tetracyclines, including demeclocycline, doxycycline, minocycline, and oxytetracycline. However, some organisms (e.g., some staphylococci, Acinetobacter) may be more susceptible to doxycycline or minocycline than to tetracycline.The National Committee for Clinical Laboratory Standards (NCCLS) states that, if results of in vitro susceptibility testing indicate that a clinical isolate is susceptible to tetracyclines, then an infection caused by this strain may be appropriately treated with dosages of the drugs recommended for that type of infection and infecting species, unless otherwise contraindicated. If results indicate that a clinical isolate has intermediate susceptibility to tetracyclines, then the strain has a minimum inhibitory concentration (MIC) that approaches usually attainable blood and tissue concentrations and response rates may be lower than for strains identified as susceptible.
Therefore, the intermediate category implies clinical applicability in body sites where the drugs are physiologically concentrated or when high dosages can be used. This intermediate category also includes a buffer zone which should prevent small, uncontrolled technical factors from causing major discrepancies in interpretation, especially for drugs with narrow pharmacotoxicity margins.
If results of in vitro susceptibility testing indicate that a clinical isolate is resistant to tetracyclines, the strain is not inhibited by systemic concentrations of the drugs achievable with normal dosage schedules and/or MICs fall in the range where specific microbial resistance mechanisms are likely and efficacy has not been reliable in clinical studies.
Disk Susceptibility Tests
When the disk-diffusion procedure is used for in vitro susceptibility testing, a tetracycline class disk containing 30 mcg of tetracycline hydrochloride may be used and results can generally be applied to all currently available tetracyclines.
However, because minocycline and doxycycline may be active against some strains of bacteria resistant to other currently available tetracyclines, additional in vitro testing using disks containing 30 mcg of minocycline or 30 mcg of doxycycline instead of or in addition to tetracycline may be necessary. When disk-diffusion susceptibility testing is performed according to NCCLS standardized procedures using the tetracycline disk and NCCLS interpretive criteria, Enterobacteriaceae or urinary isolates of Pseudomonas aeruginosa or Acinetobacter with growth inhibition zones of 19 mm or greater are susceptible to tetracyclines, those with zones of 15-18 mm have intermediate susceptibility, and those with zones of 14 mm or less are resistant to the drugs.
If susceptibility of Enterobacteriaceae or urinary isolates of Ps. aeruginosa or Acinetobacter are tested using a 30-mcg doxycycline disk, those with growth inhibition zones of 16 mm or greater are susceptible to doxycycline, those with zones of 13-15 mm have intermediate susceptibility, and those with zones of 12 mm or less are resistant to the drug. If susceptibility of these gram-negative organisms is tested using a 30-mcg minocycline disk, those with growth inhibition zones of 19 mm or greater are susceptible to minocycline, those with zones of 15-18 mm have intermediate susceptibility, and those with zones of 14 mm or less are resistant to the drug.
When disk-diffusion susceptibility testing is performed according to NCCLS standardized procedures using the tetracycline disk and Haemophilus test medium (HTM), Haemophilus with growth inhibition zones of 29 mm or greater are susceptible to tetracyclines, those with zones of 26-28 have intermediate susceptibility, and those with zones of 25 mm or less are resistant to the drugs. When tested using GC agar (with 1% defined growth supplement), N. gonorrhoeae with growth inhibition zones of 38 mm or greater are susceptible to tetracyclines, those with zones of 31-37 have intermediate susceptibility, and those with zones of 30 mm or less are resistant to the drugs. N. gonorrhoeae with growth inhibition zones of 19 mm or less usually are strains with plasmid-mediated tetracycline resistance (TRNG), and these strains should be confirmed using a dilution susceptibility test. When disk-diffusion susceptibility testing is performed according to NCCLS standardized procedures and a tetracycline disk, Staphylococcus or Enterococcus with growth inhibition zones of 19 mm or greater are susceptible to tetracyclines, those with zones of 15-18 mm have intermediate susceptibility, and those with zones of 14 mm or less are resistant to the drugs.
If susceptibility of Staphylococcus or Enterococcus is tested using a 30-mcg doxycycline disk, those with growth inhibition zones of 16 mm or greater are susceptible to doxycycline, those with zones of 13-15 mm have intermediate susceptibility, and those with zones of 12 mm or less are resistant to the drug. If susceptibility of these gram-positive organisms is tested using a 30-mcg minocycline disk, those with growth inhibition zones of 19 mm or greater are susceptible to minocycline, those with zones of 15-18 mm have intermediate susceptibility, and those with zones of 14 mm or less are resistant to the drug.
When testing susceptibility of S. pneumoniae or other Streptococcus according to NCCLS standardized procedures using Mueller-Hinton agar (supplemented with 5% sheep blood), Streptococcus with growth inhibition zones of 23 mm or greater are susceptible to tetracyclines, those with zones of 19-22 have intermediate susceptibility, and those with zones of 18 mm or less are resistant to the drugs. When the disk-diffusion susceptibility test is performed according to NCCLS standardized procedures using the tetracycline disk, Vibrio cholerae with growth inhibition zones of 19 mm or greater are susceptible to tetracyclines, those with zones of 15-18 mm have intermediate susceptibility, and those with zones of 14 mm or less are resistant to the drugs. NCCLS states that the doxycycline disk should not be used for testing susceptibility of V. cholerae since there is poor correlation between results of this test and MIC results.
Dilution Susceptibility Tests
When dilution susceptibility testing (agar or broth dilution) is performed according to NCCLS standardized procedures using tetracycline, Enterobacteriaceae or urinary isolates of Ps. Aeruginosa or other non-Enterobacteriaceae gram-negative bacilli (e.g., other Pseudomonas spp, Acinetobacter, Stenotrophomonas maltophilia) with tetracycline MICs of 4 mcg/mL or less are susceptible to tetracyclines, those with MICs of 8 mcg/mL have intermediate susceptibility, and those with MICs of 16 mcg/mL or greater are resistant to the drugs.
The same interpretive criteria should be used if susceptibility of these organisms is tested using doxycycline or minocycline. When broth dilution susceptibility tests are performed according to NCCLS standardized procedures using HTM, Haemophilus with tetracycline MICs of 2 mcg/mL or less are susceptible to tetracyclines, those with MICs of 4 mcg/mL have intermediate susceptibility, and those with MICs of 8 mcg/mL or greater are resistant to the drugs.
When dilution susceptibility testing of N. gonorrhoeae is performed using GC agar base (with 1% defined growth supplement) according to NCCLS interpretive criteria, N. gonorrhoeae with tetracycline MICs of 0.25 mcg/mL or less are susceptible to tetracyclines, those with MICs of 0.5-1 mcg/mL have intermediate susceptibility, and those with MICs of 2 mcg/mL or greater are resistant to the drugs.
When dilution susceptibility testing is performed according to NCCLS standardized procedures, Staphylococcus or Enterococcus with tetracycline MICs of 4 mcg/mL or less are susceptible to tetracyclines, those with MICs of 8 mcg/mL have intermediate susceptibility, and those with MICs of 16 mcg/mL or greater are resistant to the drugs. The same interpretive criteria should be used if susceptibility of these gram-positive organisms is tested using doxycycline or minocycline. When broth dilution susceptibility tests are performed according to NCCLS standardized procedures using cation-adjusted Mueller-Hinton broth (with 2-5% lysed horse blood), Streptococcus, including S. pneumoniae, with tetracycline MICs of 2 mcg/mL or less are susceptible to tetracyclines, those with MICs of 4 mcg/mL have intermediate susceptibility, and those with MICs of 8 mcg/mL or greater are resistant to the drugs.
When both dilution susceptibility tests are performed according to NCCLS standardized procedures, V. cholerae with tetracycline MICs of 4 mcg or less are susceptible to tetracyclines, those with MICs of 8 mcg have intermediate susceptibility, and those with MICs of 16 mcg or greater are resistant to the drugs. These same interpretive criteria should be used if susceptibility of V. cholerae is tested using doxycycline.
Gram-negative Bacteria
Tetracyclines generally are active in vitro and in vivo against the following gram-negative bacteria: Bartonella bacilliformis, Bordetella pertussis, Brucella, Calymmatobacterium granulomatis, Campylobacter fetus, Francisella tularensis, Haemophilus ducreyi, H. influenzae, Legionella pneumophila, Leptotrichia buccalis, Neisseria gonorrhoeae, N. meningitidis, Pasteurella multocida, Burkholderia pseudomallei (formerly Pseudomonas pseudomallei), B. mallei (formerly Ps. mallei, Shigella, Spirillum minus, Streptobacillus moniliformis, Yersinia enterocolitica, and Y. pestis. Although tetracyclines are active in vitro against some strains of Acinetobacter, Bacteroides, Enterobacter aerogenes, Escherichia coli, and Klebsiella, most strains of these organisms are resistant to the drugs.
Nearly all strains of Proteus and Pseudomonas aeruginosa are resistant to tetracyclines. In one study evaluating susceptibility of F. tularensis isolated from humans and animals, the MIC of tetracycline for this organism was 0.38 mcg/mL. In a study evaluating in vitro susceptibility of 100 Y. pestis isolates obtained from plague patients in Africa, all isolates were inhibited by doxycycline concentrations of 4 mcg/mL or less or tetracycline concentrations of 2 mcg/mL or less; the MIC90 for these drugs was 1 or 2 mcg/mL, respectively. In another study of Y. pestis isolates obtained from plague patients, rats, or fleas from Vietnam, these strains were inhibited in vitro by doxycycline concentrations of 0.25-1 mcg/mL and tetracycline concentrations of 0.5-4 mcg/mL. In addition, doxycycline has been shown to have in vivo activity against Y. pestis in murine plague infections.
Tetracyclines usually are active in vitro and in vivo against Vibrio cholerae and V. parahaemolyticus. V. vulnificus may be inhibited in vitro by minocycline concentrations of 0.06-0.25 mcg/mL. While the clinical importance is unclear, results of an in vitro study and a study in mice indicate that the combination of cefotaxime and minocycline is more active against V. vulnificus than either anti-infective alone.
Gram-positive Bacteria
Tetracyclines are active in vitro and in vivo against some gram-positive bacteria including Bacillus anthracis, Actinomyces israelii, Arachnia propionica, Clostridium perfringens, C. tetani, Listeria monocytogenes, Nocardia, and Propionibacterium acnes. Results of in vitro susceptibility testing of 11 B. anthracis isolates that were associated with cases of inhalational or cutaneous anthrax that occurred in the US (Florida, New York, District of Columbia) during September and October 2001 in the context of an intentional release of anthrax spores (biologic warfare, bioterrorism) indicate that these strains had tetracycline MICs of 0.06 mcg/mL and doxycycline MICs of 0.03 mcg/mL. Based on interpretive criteria established for staphylococci, these strains are considered susceptible to tetracyclines.
Although strains of B. anthracis with naturally occurring resistance to tetracycline have not been reported to date, there are published reports of strains that have been engineered to have tetracycline and penicillin resistance as well as resistance to other anti-infectives (e.g., macrolides, chloramphenicol, rifampin). Anti-infectives are effective against the germinated form of B. anthracis, but are not effective against the spore form of the organism. Although tetracyclines also are active in vitro and in vivo against some strains of staphylococci and streptococci, tetracycline resistance has been reported in these organisms with increasing frequency.
Spirochetes
Spirochetes, including Borrelia recurrentis, Leptospira, Treponema pallidum, and T. pertenue, generally are inhibited in vivo by tetracyclines. Borrelia burgdorferi, the causative organism of Lyme disease, reportedly may be inhibited in vitro by tetracycline, doxycycline, or minocycline concentrations of 0.01-2 mcg/mL. Minimum bactericidal concentrations for B. burgdorferi generally have ranged from 0.8 to 3.2 mcg/mL for tetracycline and from 0.4 to 6.4 mcg/mL for doxycycline.
Other Organisms
Tetracyclines generally are active in vitro and in vivo against Rickettsia akari, R. prowazeki, R. rickettsii, R. tsutsugamushi, R. typhi, and Coxiella burnetii. Tetracyclines are active in vitro and in vivo against Chlamydia trachomatis and C. psittaci. Mycoplasma hominis, M. pneumoniae, and Ureaplasma urealyticum (formerly T-strain mycoplasma) also are generally inhibited in vitro and in vivo by tetracyclines although some strains are naturally resistant. Tetracycline has demonstrated activity in vitro against most strains of Helicobacter pylori (formerly Campylobacter pylori or C. pyloridis).
Doxycycline and tetracycline hydrochloride have demonstrated activity in vitro against Mycobacterium fortuitum, and tetracycline hydrochloride and minocycline have demonstrated activity in vitro and in vivo against M. marinum.
Tetracyclines are active against Balantidium coli in vitro and in vivo. Doxycycline is a blood schizonticidal agent and is active against the asexual erythrocytic forms of P. falciparum; however, the drug is not gametocyticidal for P. falciparum. Doxycycline usually is not active against exoerythrocytic forms of P. falciparum, but the drug may interfere, irregularly, with the early hepatic exoerythrocytic stage of development of the plasmodium.
Resistance
Resistance to tetracyclines may be natural or acquired. Resistance is usually caused by decreased permeability of the cell surface as the result of mutation or the presence of an inducible plasmid-mediated resistance factor which is acquired via conjugation. Plasmid-mediated resistance can be transferred between organisms of the same or different species, and resistance to other tetracyclines and several other anti-infectives (e.g., aminoglycosides, chloramphenicol, sulfonamides) may be transferred on the same plasmid. N. gonorrhoeae resistant to tetracyclines were reported with increasing frequency in the US beginning in the 1980s.
Although some strains of N. gonorrhoeae with plasmid-mediated, high-level resistance to tetracyclines (TRNG) may be susceptible to cephalosporins (e.g., ceftriaxone) and/or spectinomycin, strains of penicillinase-producing N. gonorrhoeae (PPNG) (which is plasmid mediated) that also have plasmid or chromosomally mediated resistance to tetracyclines have been reported in the US. N. gonorrhoeae with chromosomally mediated resistance (CMRNG) to penicillins frequently also exhibit chromosomally mediated resistance to tetracyclines. Rarely, CMRNG may be resistant to penicillins, tetracyclines, and cephalosporins.
Complete cross-resistance usually occurs between demeclocycline, doxycycline, oxytetracycline, and tetracycline; however, only partial cross-resistance occurs between these derivatives and minocycline, and some organisms resistant to other currently available tetracyclines may be susceptible to minocycline.
Pharmacokinetics
Absorption
Demeclocycline hydrochloride, tetracycline, and tetracycline hydrochloride are approximately 60-80% absorbed from the GI tract in fasting adults. Doxycycline salts and minocycline hydrochloride are 90-100% absorbed from the GI tract in fasting adults. Absorption occurs mainly from the stomach and upper small intestine. Food and/or milk reduce GI absorption of oral preparations of tetracycline by 50% or more. GI absorption of oral preparations of doxycycline and minocycline (except minocycline hydrochloride pellet-filled capsules) may be reduced up to 20% by food and/or milk; however, the effect is not usually clinically important. Tetracyclines are poorly and erratically absorbed following IM administration.
Following oral administration of tetracyclines in fasting adults with normal renal function, peak serum concentrations of the drugs are usually attained within 1.5-4 hours. There is considerable interindividual variation in serum concentrations achieved with a specific oral dose of a tetracycline derivative, presumably because of interindividual differences in GI absorption rates.
Following IM administration of oxytetracycline hydrochloride, peak serum concentrations of the drug are usually attained within 30 minutes-1 hour. In the usual dosage, IM administration of oxytetracycline hydrochloride produces lower serum concentrations than does oral administration.
Distribution
Tetracyclines are widely distributed into body tissues and fluids including pleural fluid, bronchial secretions, sputum, saliva, ascitic fluid, synovial fluid, aqueous and vitreous humor, and prostatic and seminal fluids.
The degree of protein binding for the tetracyclines has been reported as follows: Drug % Bound to Serum Proteins Demeclocycline 36-91 Doxycycline 25-93 Minocycline 55-88 Oxytetracycline 10-40 Tetracycline 20-67 Tetracyclines are readily taken up by the reticuloendothelial cells of the liver, spleen, and bone marrow. Only small amounts of tetracyclines generally diffuse into CSF following oral, IM, or IV administration.
Minocycline and, to a lesser extent, doxycycline are more lipid soluble than other currently available tetracyclines and penetrate most body tissues and fluids better than do the other tetracyclines. All the tetracyclines are distributed into bile and undergo enterohepatic circulation in varying degrees. In the absence of biliary obstruction, concentrations of the drugs in bile may be 2-32 times higher than concurrent serum concentrations.
Tetracyclines have an affinity for and localize in tumors and necrotic or ischemic tissue where the drugs may persist for several weeks or months. The drugs also localize in and form stable tetracycline-calcium orthophosphate complexes at sites of new bone formation and calcification and in the dentin and enamel of developing teeth; these complexes have no antimicrobial activity. Tetracyclines readily cross the placenta and are distributed into milk in concentrations that may be equal to maternal serum concentrations.
Elimination
In adults with normal renal function, the serum half-lives of the tetracyclines (includes data from single and, when available, multiple-dose studies) have been reported as follows: Drug Serum half-life (in hours) Demeclocycline 10-17 Doxycycline 14-24 Minocycline 11-26 Oxytetracycline 6-10 Tetracycline 6-12 The half-lives of the drugs increase slightly following multiple doses.
Serum concentrations of tetracyclines may be higher and the half-lives slightly prolonged in patients with severe hepatic impairment or obstruction of the common bile duct. Serum concentrations of demeclocycline, minocycline, oxytetracycline, and tetracycline are higher and the half-lives prolonged in patients with impaired renal function. Serum concentrations of doxycycline are not substantially increased and the half-life of the drug is only slightly prolonged in patients with severe renal impairment. Demeclocycline, oxytetracycline, and tetracycline do not appear to be metabolized and are excreted unchanged mainly in urine by glomerular filtration. Both doxycycline and minocycline are excreted mainly by nonrenal routes.
Although it was previously suggested that doxycycline is partially metabolized in the liver, the drug probably is not metabolized in the liver but is partially inactivated in the intestine by chelate formation.
Preliminary studies indicate that minocycline, unlike other currently available tetracyclines, is partially metabolized to at least 6 metabolites. Tetracyclines are excreted into the GI tract via bile and by nonbiliary routes where they may become bound to fecal materials as inactive salts or complexes. Oxytetracycline is moderately hemodialyzable; however, other tetracyclines are only minimally removed by hemodialysis or peritoneal dialysis.
Chemistry and Stability
Chemistry
Tetracyclines are antibiotics and semisynthetic antibiotic derivatives obtained from cultures of Streptomyces. All commercially available tetracyclines contain the tetracycline nucleus. Addition of various groups at R5, R6, and R7 of the tetracycline nucleus results in derivatives with different degrees of antibacterial activity, GI absorption, affinity for divalent and trivalent cations, and protein binding. Tetracyclines and salts of the drugs generally occur as yellow, crystalline powders. Tetracycline bases are amphoteric and very slightly soluble in water while tetracycline salts are generally sparingly soluble to freely soluble in water.
Stability
In general, tetracyclines are stable in acid solutions with a pH greater than 2, but the drugs are rapidly inactivated in neutral and alkaline solutions. Tetracyclines, except minocycline, generally exhibit a brilliant yellow fluorescence under ultraviolet light. Tetracyclines readily chelate divalent and trivalent cations including aluminum, calcium, iron, magnesium, and zinc to form insoluble complexes.
Of the currently available tetracyclines, demeclocycline has the greatest affinity and doxycycline has the least affinity for calcium ions. Tetracyclines are potentially physically and/or chemically incompatible with some drugs and IV infusion solutions, but the compatibility depends on the specific drug and several other factors (e.g., concentration of the drugs, specific diluents used, resulting pH, temperature). Specialized references should be consulted for specific compatibility information.




