Sulfadiazine, Sulfamethizole, Sulfapyridine, Sulfasalazine, Sulfisoxazole, Sulfisoxazole Acetyl
Sulfonamides, synthetic derivatives of p-aminobenzenesulfonamide (sulfanilamide), are classified as anti-infectives if they possess antibacterial activity that is antagonized by p-aminobenzoic acid or p-aminobenzoyl glutamic acid.
Uses
Although at one time sulfonamides were widely used in the treatment and prophylaxis of infections, the development of resistance in formerly susceptible organisms has greatly limited the clinical usefulness of the drugs. Whenever possible, sulfonamide therapy should be justified by bacteriologic diagnosis.
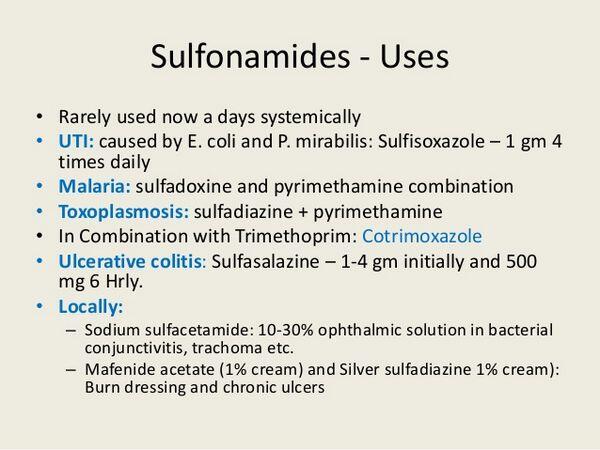
Urinary Tract Infections
Sulfonamides are used for the treatment of acute, nonobstructive urinary tract infections including pyelonephritis, pyelitis, and cystitis caused by susceptible organisms such as Escherichia coli, Klebsiella, Enterobacter, Staphylococcus aureus, Proteus mirabilis, and Proteus vulgaris. Chronic or recurrent urinary tract infections usually respond only temporarily to sulfonamide therapy. The most useful sulfonamides for the treatment of acute urinary tract infections are those with a high solubility at acidic pH, high antibacterial activity in urine, a low frequency of acetylation and crystalluria, and adequate antibacterial concentrations in blood and tissues during the period of high urinary excretion. The fixed combination preparation containing sulfamethoxazole and trimethoprim is considered a drug of choice for empiric treatment of acute uncomplicated urinary tract infections. Sulfamethizole and sulfisoxazole also are used in the treatment of urinary tract infections. Sulfasalazine is not used in the treatment of urinary tract infections; sulfadiazine should only be used for the treatment of urinary tract infections when more soluble sulfonamides have not been effective. Combination preparations containing sulfamethizole or sulfisoxazole with phenazopyridine hydrochloride are commercially available and may be used for the initial treatment of uncomplicated urinary tract infections caused by susceptible organisms when relief of symptoms of pain, burning, or urgency is needed during the first 2 days of therapy. There is a lack of evidence that combinations of sulfonamides with phenazopyridine hydrochloride provide greater benefit than a sulfonamide alone after 2 days, and treatment beyond 2 days should only be continued with a sulfonamide alone.
Nocardiosis
Sulfonamides are used for the treatment of nocardiosis. Co-trimoxazole or a sulfonamide alone (e.g., sulfisoxazole) are considered drugs of choice for the treatment of nocardiosis. Alternative anti-infectives for the treatment of nocardiosis include a tetracycline (should not be used in pregnant women or children younger than 8 years of age), amoxicillin and clavulanate potassium, imipenem, meropenem, amikacin, cycloserine, or linezolid. Amikacin and cycloserine generally should be reserved for use in the treatment of severe infections when other drugs are ineffective. In patients with nocardiosis involving the CNS or when the infection is disseminated or overwhelming, some clinicians suggest that amikacin be included during the first 4-12 weeks of therapy or until there is clinical improvement. In vitro susceptibility testing, if available, is recommended to guide selection of an anti-infective agent for the treatment of severe nocardiosis or for the treatment of patients unable to tolerate a sulfonamide. Nocardiosis in immunocompetent patients with lymphocutaneous disease usually responds after 6-12 weeks of appropriate anti-infective therapy. Immunocompromised patients and those with invasive disease require 6-12 months of anti-infective therapy and, because of the possibility of relapse, therapy should be continued for at least 3 months after apparent cure; nocardiosis in patients with human immunodeficiency virus (HIV) infection may require even longer therapy. Drainage of abscesses may be beneficial, especially in immunocompromised patients.
Chlamydial Infections
Although erythromycin usually is considered the drug of choice for the treatment of Chlamydia trachomatis conjunctivitis and pneumonia in infants, the American Academy of Pediatrics (AAP) suggests that an oral sulfonamide can be used after the immediate neonatal period for the treatment of chlamydial conjunctivitis or pneumonia in infants who cannot tolerate erythromycin. Although sulfonamides have been used in the past as alternatives for the treatment of infections caused by the lymphogranuloma venereum serotype of Chlamydia trachomatis and have been used for the treatment of pelvic inflammatory disease (PID), sulfonamides are not included in current US Centers for Disease Control and Prevention (CDC) recommendations for treatment of these infections.
Chancroid
Oral sulfonamides have been used for the treatment of chancroid, genital ulcers caused by Haemophilus ducreyi; however, the CDC and many clinicians currently recommend oral erythromycin, oral azithromycin, oral ciprofloxacin, or IM ceftriaxone as the treatments of choice for chancroid.
Asymptomatic Meningococcus Carriers
Oral sulfonamides (e.g., sulfadiazine, sulfisoxazole) have been used to eliminate meningococci from the nasopharynx of asymptomatic N. meningitidis carriers and for chemoprophylaxis in close contacts of individuals with invasive meningococcal disease. However, strains of N. meningitidis resistant to sulfonamides are prevalent and other anti-infective agents (i.e., rifampin, ceftriaxone, ciprofloxacin) generally are recommended to eliminate nasopharyngeal carriage of meningococci or for chemoprophylaxis of meningococcal disease. Sulfonamides are no longer included in CDC or AAP guidelines for chemoprophylaxis of meningococcal disease.
Prophylaxis of Recurrent Rheumatic Fever
Although IM penicillin G benzathine generally is considered the drug of choice for prophylaxis of recurrent rheumatic fever (secondary prevention), oral prophylaxis with penicillin V potassium, sulfadiazine, or sulfisoxazole also is effective and may be used in patients at lower risk of rheumatic recurrences. Sulfadiazine or sulfisoxazole should be used when hypersensitivity precludes the use of a penicillin; however, the increasing incidence of sulfonamide-resistant Streptococcus pyogenes (group A b-hemolytic streptococci) should be considered. Sulfonamides will not eradicate group A b-hemolytic streptococci nor prevent potential complications (e.g., poststreptococcal glomerulonephritis) and therefore should not be used for the acute treatment of group A b-hemolytic streptococcal infections including pharyngitis and tonsillitis.
Toxoplasmosis
Treatment Sulfadiazine is used in conjunction with pyrimethamine for the treatment of toxoplasmosis. Sulfadiazine is designated an orphan drug by the US Food and Drug Administration (FDA) for use in this condition. Most clinicians currently state that pyrimethamine in conjunction with sulfadiazine is the regimen of choice when treatment of toxoplasmosis is indicated, including toxoplasmosis in immunocompromised patients (e.g., those with acquired immunodeficiency syndrome [AIDS]) and symptomatic congenital infections. Oral or parenteral leucovorin usually is added to pyrimethamine and sulfonamide therapy to prevent pyrimethamine-induced adverse hematologic effects. In the treatment of ocular toxoplasmosis with macular involvement, some clinicians suggest use of systemic corticosteroids in addition to pyrimethamine and a sulfonamide; however, other clinicians caution that use of corticosteroids in the management of ocular complications or CNS disease is controversial. Spiramycin (not commercially available in the US) is considered an alternative to combination therapy with pyrimethamine and sulfadiazine for the treatment of toxoplasmosis. The AAP also recommends a regimen of clindamycin and pyrimethamine in patients who cannot tolerate sulfonamides. Appropriate clinical specialists should be consulted regarding treatment of toxoplasmosis in pregnant women.
Prevention
The Prevention of Opportunistic Infections Working Group of the US Public Health Service and the Infectious Diseases Society of America (USPHS/IDSA) recommends that HIV-infected individuals who have completed initial therapy for toxoplasmic receive long-term suppressive or maintenance therapy (secondary prophylaxis) to prevent relapse. Secondary prophylaxis against toxoplasmosis is generally administered for life, unless immune recovery has occurred as the result of potent antiretroviral therapy. The USPHS/IDSA and other clinicians state that combination therapy with pyrimethamine (with leucovorin) and sulfadiazine generally is the regimen of choice for secondary prophylaxis in these patients since it provides coverage against both toxoplasmosis and Pneumocystis jiroveci (formerly Pneumocystis carinii) pneumonia (PCP). Alternatively, especially for patients who cannot tolerate sulfonamides, a regimen of pyrimethamine (and leucovorin) used in conjunction with clindamycin is recommended. For information on USPHS/IDSA recommendations regarding primary and secondary prophylaxis of toxoplasmosis in HIV-infected individuals, including when to initiate or discontinue such prophylaxis.
Malaria
The fixed-combination preparation of sulfadoxine and pyrimethamine is used in conjunction with quinine sulfate for the treatment of uncomplicated chloroquine-resistant Plasmodium falciparum and P. vivax malaria and is one of several regimens of choice for these infections. The fixed-combination preparation also is used for presumptive self-treatment in individuals who elect not to take prophylaxis and to treat themselves if they experience symptoms or individuals who require or chose prophylaxis regimens that do not have optimal efficacy (i.e., use of chloroquine prophylaxis in areas with chloroquine-resistant P. falciparum.) Because severe and sometimes fatal adverse reactions have been reported with sulfadoxine and pyrimethamine, the CDC and most clinicians currently do not recommend use of the drug for prevention of malaria. For further information on prevention and treatment of malaria with the fixed-combination preparation containing sulfadoxine and pyrimethamine.
Plague
Although other anti-infectives generally are used in the treatment of plague (e.g., streptomycin, tetracycline, chloramphenicol), co-trimoxazole is recommended by the CDC for anti-infective prophylaxis in adults 18 years of age and older and children at least 2 months of age with close exposure to pneumonic plague or an exceptionally high risk of exposure to plague.
Rheumatoid Arthritis
Sulfasalazine is used in the management of rheumatoid arthritis in adults whose symptoms progress despite an adequate regimen of nonsteroidal anti-inflammatory agents (NSAIAs) and for the management of polyarticular course juvenile rheumatoid arthritis in pediatric patients who have had an inadequate response to NSAIAs.
Other Uses
Although bacillary dysentery caused by sulfonamide-susceptible strains of Shigella has been controlled or prevented by oral sulfonamides, many strains of Shigella, especially S. sonnei, are now resistant to sulfonamides and other anti-infectives (e.g., fluoroquinolones, co-trimoxazole, azithromycin, cephalosporins, ampicillin) generally are indicated. Some sulfonamides may be used concomitantly with erythromycin for the treatment of acute otitis media caused by susceptible Haemophilus influenzae. Sulfasalazine, but not other sulfonamides, is used in the treatment of ulcerative colitis. Sulfasalazine also is used in the treatment of Crohn’s disease. Some of the sulfonamides (e.g., sulfisoxazole or sulfabenzamide, sulfacetamide, or sulfathiazole [drugs no longer commercially available in the US]) have been used intravaginally in the treatment of bacterial vaginosis (formerly called Haemophilus vaginitis, Gardnerella vaginitis, nonspecific vaginitis, Corynebacterium vaginitis, or anaerobic vaginosis); however, topical sulfonamides are usually ineffective in the treatment of infections of mucous membranes, possibly because pus and cellular debris inhibit their action. These agents are generally considered as lacking substantial evidence of efficacy in the topical treatment of vaginal infections. In addition, topical application may produce sensitization and preclude later systemic use of sulfonamides.
Dosage and Administration
Administration
Sulfonamides are administered orally.
Dosage
Sulfonamide dosage should be adjusted individually according to the severity of the infection, the pharmacokinetics of the individual sulfonamide being used, and the response and tolerance of the patient. The short-acting sulfonamides must usually be given at 4- to 6-hour intervals; an initial loading dose usually is recommended.
Cautions
Adverse effects of the sulfonamides are numerous and may involve nearly all organ systems. Although serious, in some cases fatal, reactions have been reported, they occur infrequently.
Sensitivity Reactions
Many of the adverse effects that have been attributed to the sulfonamides appear to be hypersensitivity reactions. The incidence of hypersensitivity reactions appears to increase with increased sulfonamide dosage. Although cross-sensitization has been reported to occur between the various anti-infective sulfonamides, some diuretics such as acetazolamide and the thiazides, some goitrogens, and sulfonylurea antidiabetic agents, the association between hypersensitivity to sulfonamide anti-infectives and subsequent sensitivity reactions to non-anti-infective sulfonamides (e.g., thiazides, sulfonylurea antidiabetic agents, furosemide, dapsone, probenecid) appears to result from a predisposition to allergic reactions in general rather than to cross-sensitivity to the sulfa moiety per se. The mechanism of sulfonamide sensitivity is poorly understood, and the contribution of allergens, haptens, and/or other immune mechanisms remains to be established. For additional information on cross-sensitivity. Various dermatologic reactions, including rash, pruritus, urticaria, erythema nodosum, erythema multiforme (Stevens-Johnson syndrome), Lyell’s syndrome (may be associated with corneal damage), Behcet’s syndrome, toxic epidermal necrolysis, and exfoliative dermatitis, have been reported in patients receiving sulfonamides. Because photosensitivity may also occur, patients should be cautioned against exposure to UV light or prolonged exposure to sunlight. A relatively high proportion of fatalities has occurred as a result of the Stevens-Johnson syndrome, especially in children. Although long-acting sulfonamides (which are no longer commercially available) have been associated most often with the Stevens-Johnson syndrome, other sulfonamides also have been reported to cause this reaction. The physician should be alert to the signs, including high fever, severe headache, stomatitis, conjunctivitis, rhinitis, urethritis, and balanitis, which may precede the onset of the cutaneous lesions of the Stevens-Johnson syndrome. If a rash develops during therapy, the sulfonamide should be discontinued at once. In rare instances, a skin rash may precede a more serious reaction such as Stevens-Johnson syndrome, toxic epidermal necrolysis, hepatic necrosis, and/or serious blood disorders. Fever, which may develop 7-10 days after the initial sulfonamide dose, is a common adverse effect of sulfonamide therapy. Serum sickness syndrome or serum sickness-like reactions (e.g., fever, chills, rigors, flushing, joint pain, urticarial eruptions, conjunctivitis, bronchospasm, leukopenia), have been reported; rarely, anaphylactoid reactions and anaphylaxis may occur. Lupus erythematosus-like syndrome, disseminated lupus erythematosus, angioedema, vasculitis, vascular lesions including periarteritis nodosa and arteritis, cough, shortness of breath, chills, pulmonary infiltrates, pneumonitis (which may be associated with eosinophilia), fibrosing alveolitis, pleuritis, pericarditis with or without tamponade, allergic myocarditis, hepatitis, hepatic necrosis with or without immune complexes, parapsoriasis varioliformis acuta, alopecia, conjunctival and scleral injection, periorbital edema, and arthralgia have also been reported. If a hypersensitivity reaction occurs during sulfonamide therapy, the drugs should be discontinued immediately. Desensitization to sulfasalazine has been used when reinstitution of therapy with the drug was considered necessary in patients with inflammatory bowel disease who had hypersensitivity reactions to the drug.Desensitization to sulfadiazine has also been used in several patients with acquired immunodeficiency syndrome (AIDS) when use of sulfadiazine for the treatment of toxoplasmosis was considered necessary in patients who had hypersensitivity reactions to the drug. Specialized references should be consulted for specific information on desensitization procedures and dosage.
Hematologic Effects
Adverse hematologic effects, including methemoglobinemia, sulfhemoglobinemia, granulocytopenia, leukopenia, congenital neutropenia, eosinophilia, hemolytic anemia, agranulocytosis, aplastic anemia, purpura, clotting disorder, thrombocytopenia, myelodysplastic syndrome, hypofibrinogenemia, and hypoprothrombinemia, rarely resulting in death, have been associated with sulfonamide therapy. Acute hemolytic anemia may occur during the first week of therapy as a result of sensitization or glucose-6-phosphate dehydrogenase (G-6-PD) deficiency. This reaction may also occur in the fetus or premature infant in whom G-6-PD is normally deficient. Mild, chronic hemolytic anemia may occur during prolonged sulfonamide therapy. Agranulocytosis may rarely occur 10-14 days after initiation of therapy. Complete blood cell counts should be performed regularly in patients receiving sulfonamides for longer than 2 weeks. If signs of adverse hematologic effects such as sore throat, fever, pallor, purpura, jaundice, or weakness occur, sulfonamide therapy should be discontinued until the possibility of a blood disorder is eliminated.
Hepatic Effects
Functional and morphologic hepatic changes, possibly causing jaundice, may appear within 3-5 days after initiation of sulfonamide therapy. Focal or diffuse necrosis of the liver has been reported rarely.
Renal Effects
Renal damage, manifested by renal colic, nephritis, urolithiasis, toxic nephrosis with anuria and oliguria, hematuria, proteinuria, kidney stone formation, and elevation of BUN and creatinine concentrations, is usually a result of crystalluria caused by precipitation of the sulfonamide and/or its N4-acetyl derivative in the urinary tract. The occurrence of crystalluria is related to the urinary concentration and the solubility characteristics of the sulfonamide and its metabolites. The risk of crystalluria may be decreased by maintaining an adequate urinary output and by increasing urinary pH. Unless the urine is highly acidic and/or the drug is relatively insoluble, alkalinization of the urine is usually not necessary if the urinary output is maintained at a minimum of 1500 mL daily. Urinary alkalinization may be achieved by administering 2.5-4 g of sodium bicarbonate orally every 4 hours. Urinalysis and kidney function tests should be performed weekly to detect any renal complications. If persistent, heavy crystalluria, hematuria, or oliguria occurs, sulfonamide therapy should be discontinued and alkali therapy maintained. Nephritis and hemolytic-uremic syndrome also have been reported.
GI Effects
Nausea and vomiting occur frequently in patients receiving sulfonamides. Abdominal pain, anorexia, glossitis, stomatitis, pancreatitis, gastroenteritis, diarrhea, neutropenic enterocolitis, GI hemorrhage, melena, flatulence, and salivary gland enlargement also have been reported. Clostridium difficile-associated diarrhea and colitis (also known as antibiotic-associated pseudomembranous colitis) caused by toxin-producing clostridia has been reported following sulfonamide therapy. If C. difficile-associated diarrhea and colitis occurs, mild cases may respond to discontinuance of sulfonamide therapy alone, but diagnosis and management of moderate to severe cases should include sigmoidoscopy (or other appropriate endoscopic examination), appropriate bacteriologic studies, and treatment with fluid, electrolyte, and protein supplementation as indicated. If colitis is moderate to severe or is not relieved by discontinuance of sulfonamide therapy alone, appropriate anti-infective therapy effective against C. difficile (e.g., oral metronidazole or vancomycin) should be administered. Isolation of the patient may be advisable. Other causes of colitis also should be considered.
Nervous System Effects
Headache occurs frequently in patients receiving sulfonamides. Dizziness, vertigo, peripheral neuritis, ataxia, mental depression, hallucinations, disorientation, confusion, seizures, intracranial hypertension, tinnitus, hearing loss, anxiety, apathy, and acute psychosis, occur less frequently. Peripheral neuropathy, paresthesia, weakness, fatigue, drowsiness, lassitude, restlessness, insomnia, meningitis, cauda equina syndrome, and Guillain-Barre syndrome also have been reported.
Other Adverse Effects
Other reported adverse effects of sulfonamides include goiter production, hypothyroidism, hypoglycemia, diuresis, pharyngitis, arthralgia, acidosis, and cyanosis. The nonabsorbable sulfonamides reportedly decrease bacterial synthesis of vitamin K1, which may result in hypoprothrombinemia and hemorrhage; these sulfonamides may also reduce fecal output of thiamine.
Precautions and Contraindications
Sulfonamides should be used with caution and in reduced dosage in patients with impaired hepatic function, impaired renal function, or urinary obstruction, since excessive accumulation of the drugs may occur in these patients. The drugs should also be administered with caution in patients with blood dyscrasia, severe allergies or asthma, or G-6-PD deficiency. The development of sore throat, fever, rash, pallor, arthralgia, cough, shortness of breath, purpura, or jaundice during sulfonamide therapy may be an early sign of a serious adverse reaction. Renal function tests and complete blood cell counts should be performed frequently during sulfonamide therapy, especially during prolonged therapy with the drugs. Microscopic urinalyses should be done weekly when patients are treated with a sulfonamide for longer than 2 weeks. Because pseudomembranous colitis has been reported with the use of nearly all anti-infective agents, including sulfonamides, and may range in severity from mild to life threatening, it should be considered in the differential diagnosis of patients who develop diarrhea during the administration of sulfonamides. The frequency of resistant organisms limits the usefulness of sulfonamides as sole therapy in the treatment of urinary tract infections. Since sulfonamides are bacteriostatic and not bacteriocidal, a complete course of therapy is needed to prevent immediate regrowth and the development of resistant urinary pathogens. Sulfonamides are contraindicated in patients with a history of hypersensitivity to sulfonamides or other chemically related drugs (e.g., sulfonylureas, thiazides). The drugs are also contraindicated in patients with marked renal or hepatic impairment. Sulfonamides are contraindicated in patients with porphyria, since the drugs may precipitate an acute attack. Sulfasalazine (but not other sulfonamides) is contraindicated in patients hypersensitive to salicylates and in patients with intestinal or urinary obstruction.
Pediatric Precautions
Kernicterus, caused by displacement of bilirubin from protein binding sites, has occurred in neonates treated with sulfonamides. Unless indicated for the treatment of congenital toxoplasmosis, sulfonamides are generally contraindicated in children younger than 2 months of age. Pending further accumulation of data on use of the drugs in pediatric patients, sulfacytine should not be used in children younger than 14 years of age.
Pregnancy and Lactation
Safe use of sulfonamides during pregnancy has not been established. The teratogenic potential of most sulfonamides has not been adequately studied in humans or animals; however, an increase in the incidence of cleft palate and other bony abnormalities has been reported when some sulfonamides were administered orally in doses 7-25 times the usual human dose to pregnant rats and mice. Sulfonamides are contraindicated in pregnant women at term or whenever the possibility of premature birth exists, since the drugs cross the placenta and may cause kernicterus. Because sulfonamides are distributed into milk, and because of the potential for serious adverse reactions from the drugs in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the woman. Because of the risk of kernicterus in infants younger than 2 months of age, use of sulfonamides is contraindicated in lactating women who are nursing such infants.
Drug Interactions
Folic Acid Antagonists
Because pyrimethamine and trimethoprim also interfere with folic acid synthesis in susceptible organisms, but at different stages, these drugs act synergistically with sulfonamides against some organisms. This synergism is used to therapeutic advantage in the treatment of toxoplasmosis and malaria. Although clinical reports are lacking, it has been suggested that sulfonamides may potentiate the effects of methotrexate by displacing methotrexate from its protein binding sites or inhibiting renal tubular secretion of the antineoplastic agent. Sulfonamides should be administered with caution to patients receiving methotrexate.
p-Aminobenzoic Acid and its Derivatives
Because the antibacterial activity of sulfonamides involves competitive inhibition of p-aminobenzoic acid (PABA), the concomitant use of PABA or local anesthetics which are derivatives of PABA (e.g., chloroprocaine, piperocaine, procaine, propoxycaine [no longer commercially available in the US], tetracaine) reportedly may antagonize the antibacterial activity of sulfonamides. Although the clinical importance of this effect is unclear, PABA and local anesthetics derived from PABA probably should not be used in patients receiving a sulfonamide.
Coumarin Anticoagulants
Sulfonamides may potentiate the effects of coumarin anticoagulants by displacing the anticoagulants from their protein-binding sites. Some sulfonamides also reportedly enhance the hypoprothrombinemic effect of oral anticoagulants by impairing metabolism of the drugs. Patients receiving a sulfonamide and a coumarin anticoagulant concomitantly should be monitored closely.
Sulfonylurea Antidiabetic Agents
Sulfonamides may potentiate the hypoglycemic effects of tolbutamide and chlorpropamide by displacing the antidiabetic agents from their protein-binding sites. In addition, sulfamethizole reportedly inhibits the carboxylation of tolbutamide. Sulfonamides should be used with caution in patients receiving sulfonylurea antidiabetic agents.
Other Drugs
Sulfasalazine reportedly may reduce GI absorption of digoxin and patients receiving the drugs concomitantly should be monitored to ensure adequate serum concentrations of digoxin. Sulfamethizole reportedly may inhibit metabolism of phenytoin and should be used with caution in patients receiving the drug. Sulfisoxazole reportedly may compete with thiopental for plasma protein binding and may reduce the amount of thiopental required for anesthesia. Although the effect does not appear to be clinically important, sulfinpyrazone may displace sulfonamides from protein-binding sites and also inhibit renal tubular secretion of the anti-infectives, resulting in increased serum sulfonamide concentrations. Since salicylates and other nonsteroidal anti-inflammatory agents (e.g., fenoprofen, indomethacin, meclofenamate) are highly protein bound, these drugs theoretically could be displaced from binding sites by sulfonamides, or could displace sulfonamides from binding sites. Although no clinically important drug interactions have been reported, patients receiving sulfonamides concomitantly with nonsteroidal anti-inflammatory agents should be observed for adverse effects. Since methenamine requires acidic urine for its antibacterial effect, the drug should not be used concomitantly with less soluble sulfonamides (e.g., sulfadiazine, sulfapyridine) which may crystallize in acidic urine. In addition, an insoluble precipitate forms between formaldehyde and sulfamethizole in acidic urine; therefore, methenamine or its salts should not be used concomitantly with sulfamethizole. The potential for crystalluria may be increased when sulfonamides are administered concomitantly with paraldehyde because of increased urine acetic acid concentrations which may occur during paraldehyde therapy. The less soluble sulfonamides (e.g., sulfadiazine, sulfapyridine) probably should be given with caution to patients receiving paraldehyde.
Mechanism of Action
Sulfonamides are usually bacteriostatic in action. Sulfonamides interfere with the utilization of p-aminobenzoic acid (PABA) in the biosynthesis of tetrahydrofolic acid (the reduced form of folic acid) cofactors in susceptible bacteria. Sulfonamides are structural analogs of PABA and appear to interfere with PABA utilization by competitively inhibiting the enzyme dihydropteroate synthase, which catalyzes the formation of dihydropteroic acid (a precursor of tetrahydrofolic acid) from PABA and pteridine; however, other mechanism(s) affecting the biosynthetic pathway also may be involved. Compounds such as pyrimethamine and trimethoprim, which block later stages in the synthesis of folic acid, act synergistically with sulfonamides.Only microorganisms that synthesize their own folic acid are inhibited by sulfonamides; animal cells and bacteria which are capable of utilizing folic acid precursors or preformed folic acid are not affected by these drugs. The antibacterial activity of the sulfonamides is reportedly decreased in the presence of blood or purulent body exudates. Spectrum Sulfonamides were originally active against a wide range of gram-positive and gram-negative bacteria; however, the increasing incidence of resistance in bacteria formerly susceptible to sulfonamides has decreased the clinical usefulness of the drugs. Sulfonamides are active in vitro against gram-positive bacteria including some strains of staphylococci, streptococci, Bacillus anthracis, Clostridium tetani, and C. perfringens and many strains of Nocardia asteroides and N. brasiliensis. Although resistance to sulfonamides has been reported with increasing frequency in gram-negative bacteria, the drugs are active in vitro against many Enterobacteriaceae including Enterobacter, Escherichia coli, Klebsiella, Proteus mirabilis, P. vulgaris, Salmonella, and Shigella. Sulfonamides are active in vitro against some strains of Neisseria gonorrhoeae and N. meningitidis; however, many strains of these organisms are resistant to the drugs. Sulfonamides are active in vitro against Chlamydia trachomatis, but are generally inactive against Chlamydia psittaci. Sulfonamides also have some activity against Toxoplasma gondii and Plasmodium.
In Vitro Susceptibility
Testing Results of in vitro susceptibility tests with sulfonamides vary depending on the specific methods and media used; therefore, results of the tests should be carefully correlated with the bacteriologic and clinical response of the patient. When the disk-diffusion procedure is used to test susceptibility to sulfonamides, the National Committee for Clinical Laboratory Standards (NCCLS) recommends that a disk containing 250 or 300 mcg of sulfisoxazole be used and results applied to other sulfonamides. When the disk-diffusion procedure is performed according to NCCLS standardized procedures using the sulfisoxazole disk, urinary tract isolates of Staphylococcus, Enterobacteriaceae, Pseudomonas aeruginosa, or Acinetobacter with growth inhibition zones of 16 mm or greater are susceptible to sulfonamides, those with zones of 13-16 mm have intermediate susceptibility, and those with zones of 12 mm or less are resistant to the drugs. When dilution susceptibility testing (agar or broth dilution) is performed according to NCCLS standardized procedures using sulfisoxazole, urinary tract isolates of Staphylococcus, Enterobacteriaceae, Ps. aeruginosa, and other non-Enterobacteriaceae gram-negative bacilli (e.g., other Pseudomonas spp., Acinetobacter, Stenotrophomonas maltophilia) with MICs of 256 mcg/mL or less are susceptible to sulfonamides and those with MICs of 512 mcg/mL or greater are resistant to the drugs. Resistance Organisms initially sensitive to sulfonamides may develop resistance both in vitro and in vivo; sulfonamide-resistant strains emerge frequently when therapy is continued for 15 days or longer. Organisms made resistant to one sulfonamide, either in the laboratory or in clinical use, are usually cross-resistant to other sulfonamides. Organisms which are highly resistant to sulfonamides are usually permanently resistant; however, a slight or moderate degree of resistance may be reversible.
Pharmacokinetics
Absorption
Individual sulfonamides differ markedly in their absorption, distribution, and elimination. With the exception of sulfapyrimidine and sulfasalazine, which are only slightly absorbed, sulfonamides are generally well absorbed from the GI tract. Approximately 70-90% of an oral dose of the absorbable sulfonamides is reportedly absorbed from the small intestine; small amounts may also be absorbed from the stomach. Sulfamethizole and sulfisoxazole are absorbed rapidly; peak blood concentrations are usually obtained within 2-4 hours. Sulfadiazine and sulfapyridine are absorbed at a slower rate with peak blood concentrations occurring within 3-7 hours. Administration of oral sulfonamides with food appears to delay, but not reduce, absorption of the drugs. Absorption of sulfonamides from the vagina, respiratory tract, or abraded skin is variable and unreliable; however, enough drug may be absorbed to induce sensitization or toxicity. Although only free (unmetabolized and unbound) sulfonamides are microbiologically active, blood concentrations are often determined on the basis of total sulfonamide concentration. Generally, sulfonamide plasma concentrations are approximately twice the blood concentrations. Wide variations in blood concentrations have been reported in different individuals receiving identical doses of the same sulfonamide. Blood total sulfonamide concentrations of 12-15 mg/dL have been reported to be optimal; blood concentrations greater than 20 mg/dL have been associated with an increased incidence of adverse reactions.
Distribution
Absorbable sulfonamides are widely distributed in the body. Although most sulfonamides appear to cross cell membranes, sulfisoxazole appears to be distributed only in extracellular fluid. Sulfonamides may appear in pleural, peritoneal, synovial, amniotic, prostatic, and seminal vesicular fluid, and aqueous humor. Concentrations of some sulfonamides in the CSF may reach 35-80% of blood concentrations. Small amounts of sulfonamides are also distributed into sweat, tears, saliva, and bile. Sulfonamides readily cross the placenta; fetal plasma concentrations may exceed 50% of maternal plasma concentrations. Sulfonamides are distributed into milk. Sulfonamides are bound in varying degrees to plasma proteins. Sulfadiazine and sulfapyridine are reportedly 32-70% bound to plasma proteins and sulfamethizole and sulfisoxazole are reportedly 85-90% bound to plasma proteins. All sulfonamides are loosely bound, mainly to albumin, but small amounts of the drugs may be bound by serum globulin. Protein-bound sulfonamides do not have antibacterial activity and there is evidence that the concentration of sulfonamide in tissues is related to the concentration of unbound sulfonamide in serum.
Elimination
Sulfonamides are generally classified as short-acting, intermediate-acting, or long-acting depending on the rate at which they are absorbed and eliminated. Sulfamethizole, sulfasalazine, and sulfisoxazole are generally considered to be short-acting sulfonamides and reportedly have plasma half-lives of about 4-8 hours. Sulfadiazine and sulfapyridine are generally considered to be intermediate-acting sulfonamides and reportedly have plasma half-lives of about 7-17 hours. Although the liver is the major site of metabolism, sulfonamides may also be metabolized in other body tissues. Most sulfonamides are metabolized mainly by N 4-acetylation. The degree of acetylation, which is a function of time, varies from less than 5% for sulfamethizole to up to 40% for sulfadiazine. The N 4-acetyl metabolites, which do not possess antibacterial activity, have greater affinity for plasma albumin than does the nonacetylated drug and are usually less soluble than the parent sulfonamide, particularly in acidic urine. Like acetyl derivatives, glucuronide derivatives do not possess antibacterial activity; however, glucuronide derivatives are water soluble, appear to resemble the nonacetylated sulfonamide in plasma binding capacity, and have not been associated with adverse effects. Sulfonamides and their metabolites are excreted mainly by the kidneys via glomerular filtration, but the drugs vary widely in their rates of excretion and solubility characteristics at various urinary pH values. Although alkalinization of urine increases the solubility of sulfonamides and their metabolites (except sulfamethazine and N 4-acetylsulfamethazine), alkalinization decreases tubular reabsorption, resulting in increases renal excretion of the drugs and decreased sulfonamide blood concentrations. The metabolites do not appear to be reabsorbed by the tubules and their concentration in urine is greater than in blood. Protein-bound sulfonamides cannot be filtered by the glomeruli. Except for the poorly absorbed sulfonamides (sulfapyridine, sulfasalazine) only small amounts of sulfonamides are excreted in feces.
Chemistry and Stability
Chemistry
Sulfonamides are synthetic derivatives of p-aminobenzenesulfonamide (sulfanilamide). Compounds are classified as anti-infective sulfonamides if they possess antibacterial activity that is antagonized by p-aminobenzoic acid or p-aminobenzoyl glutamic acid and if they exhibit cross-resistance with sulfanilamide. A benzene ring with a sulfonamido group and a primary amino group (N 4) para to the sulfur side-chain are essential for antibacterial activity of sulfonamides. If the N 4-amino group is replaced with radicals that can be converted to a free amino group in the body, the compound retains antibacterial activity. Substitution in the N 1-amide group produces compounds varying in solubility, protein binding, tissue distribution, and rate and mode of metabolism and excretion. The most active sulfonamides have been obtained by substitution of heterocyclic groups in the N 1 position. Sulfonamides generally are insoluble in water. The drugs are weak acids and form salts with bases; their sodium salts are very soluble in water.
Stability
Solutions of the sodium salts of most sulfonamides are strongly basic and deteriorate rapidly. Most sulfonamides slowly darken on exposure to light and should be stored in tight, light-resistant containers.



