Essentials of Diagnosis
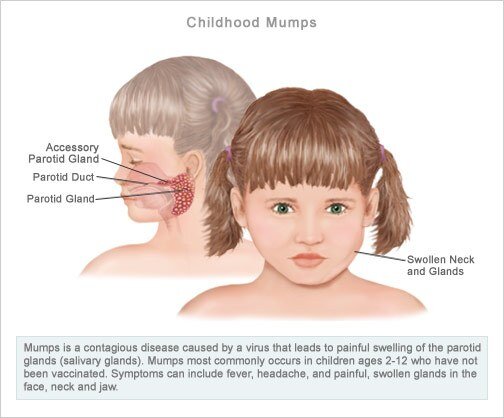
- Epidemic parotitis, usually seen in childhood.
- Most common heralding symptom is painful parotid swelling.
- Headache and meningismus common.
- Orchitis is uncommon late complication seen in post-pubertal males; rarely leads to sterility.
- Other glandular tissue may be inflamed.
General Considerations
Epidemiology
Mumps, historically known as epidemic parotitis, was one of the most common early childhood infections before the routine use of mumps vaccination starting in 1968. Reported cases of mumps have dropped 98% when compared with the prevaccine era. It is spread primarily during the late winter and early spring. Before the vaccination era, mumps epidemics occurred in 3- to 4-year cycles.
Microbiology
Mumps virus is a 150-nm paramyxovirus. It is composed of single-stranded RNA contained in a helical nucleocapsid. The viral envelope contains hemolysin, hemagglutinin, and neuraminidase.
Pathogenesis
Mumps virus is spread via respiratory secretions, with humans being the only natural reservoir. The latent phase of the virus is from 12 to 25 days. The host is communicable from 2 days before to 9 days after the onset of parotid swelling. Mumps is often inappropriately thought to be “less communicable” than other pediatric viruses. This concept is probably owing to the high incidence (20-40%) of subclinical infections.
Clinical Findings
Signs and Symptoms
Mumps virus typically infects the parotid glands but has the ability to infect other glandular tissue (Box 1). Mumps parotitis rarely has prodromal symptoms. Children can have a prodrome of fever, myalgia, and headache. In two-thirds of infections, parotid pain and swelling are the heralding symptoms. Headache and meningismus are common. Fever and parotid swelling usually begin resolving within 1 week.
Laboratory Findings
Infection can be confirmed by viral culture or serology. Culture samples can be obtained by pharyngeal swab or from urine or cerebrospinal fluid during the febrile course of disease. The virus can be cultured on a variety of cell lines including embryonated chicken egg and chick embryo fibroblast. Serology can be confirmed via enzyme immunoassay, complement fixation, or hemagglutination inhibition. Acute and convalescent serologies are helpful to monitor the course of disease.
Differential Diagnosis
The differential diagnosis of mumps parotitis includes suppurative parotitis and salivary calculus. Anterior cervical lymphadenitis can often be confused with parotitis.
Complications
Orchitis is an uncommon complication of mumps in adults and adolescents, with the highest rate found in the 15- to 29-year age group. It is rare in children. Orchitis is suspected when the patient has a high fever at the end of the first week of illness. This is soon accompanied by swelling, tenderness, and severe pain in the testis. Roughly 75% of mumps orchitis is unilateral. Rarely, testicular atrophy follows orchitis. Sterility is rare and is seen in cases of bilateral orchitis. Orchitis usually lasts 4-6 days.
Mumps infection during the first trimester of pregnancy confers an increased risk of spontaneous abortion but no increased risk of fetal malformation. Other uncommon complications include meningoencephalitis, deafness, arthritis, pancreatitis, thyroiditis, mastitis, and oophoritis.
Diagnosis
Diagnosis is based on physical findings and culture or serology. History of a mumps contact can be difficult to find owing to the significant number of subclinical cases. Cerebrospinal fluid will demonstrate a lymphocytic pleocytosis if meningitis is present.
Treatment
Therapy is aimed primarily at analgesia (Box 2). Opioids are often needed for the pain of orchitis, which can be quite severe. Local application of cool compresses may also help relieve some of the orchitis pain. Intravenous hydration may be needed for some patients. Lumbar puncture may be therapeutic for patients with severe headache. Mumps immune globulin has little clinical value. It is no longer available in the United States.
Prevention & Control
Virus is shed 1 day before onset of symptoms and continues to shed for 9 days after the onset of parotitis. Droplet isolation should be maintained on hospitalized patients during this period. Children should be excluded from school and daycare during this period.
The live virus vaccine is usually given in combination with the MMR vaccine (measles, mumps, and rubella). The first vaccine should be given between 12 and 15 months of age. The second dose is usually given between ages 4 and 6 years. If the second dose is missed, it should be given before age 12 years. Various contraindications exist for the vaccine (Box 3).
BOX 1. Mumps Clinical Syndromes
More Common
- Parotitis (present in 2/3 of infections; usually the heralding symptom)
- Mild fever
- Meningismus, often with severe headache
- Orchitis (rare in prepubescent boys)
Less Common
- Meningoencephalitis
- Deafness
- Arthritis
- Pancreatitis
- Thyroiditis
- Mastitis
- Oophoritis
BOX 2. Treatment of Mumps
- Maintain hydration
- Analgesics
- Opioids often needed for severe orchitis
- Lumbar puncture can be therapeutic for severe headache
- Mumps immune globulin is of little value, and no longer available in the United States
BOX 3. Control of Mumps
Vaccine
- Live-virus mumps vaccine is administered 0.5 cc SQ; commonly given in combination with MMR (measles, mumps, rubella) vaccine
- First dose is recommended at from 12 to 15 months of age
- Second dose is recommended at school entry (age 4 to 6 years)
- If no preschool dose is given, the second dose should be administered before age 12
MMR Vaccine Contraindications
- Pregnancy
- Febrile illness
- Planned pregnancy within 3 months
- Severe immunocompromised state
- Blood product or immune globulin within 3 to 6 months (dose dependent)
- Anaphylaxis to neomycin
MMR Vaccine Should Be Used with Caution in These Situations
- Seizure disorder
- Thrombocytopenia
- Egg allergy
Isolation Precautions
- Respiratory isolation should be maintained for 9 days after onset of parotitis
- Infected children should be excluded from school and daycare during this period

