Essentials of Diagnosis
- Progressive mentation abnormalities leading to disorders of gait and myoclonus.
- Occurs in sixth and seventh decades in previously normal patients.
- May be history of corneal transplant, neurosurgical procedures, or use of human growth hormone.
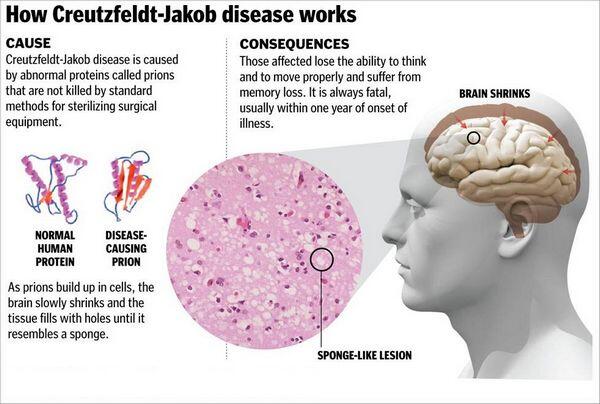
- Characteristic brain biopsy abnormalities of spongiform degeneration, neuron loss, and astrogliosis.
General Considerations
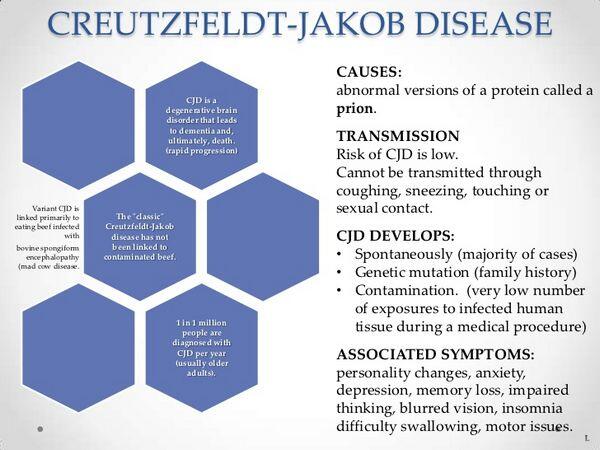
Creutzfeldt-Jakob disease is a progressive, fatal illness of the central nervous system that is seen most frequently in the sixth and seventh decades of life. The disease is sporadic and found worldwide, with an incidence of disease of 1 case/million people per year. The mode of acquisition is unknown, but a higher incidence of the disease among Israelis of Libyan origin who eat sheep eyeballs has led to speculation that the disease may be transmitted by the ingestion of scrapie-infected tissue. Infection has been transmitted by corneal transplants, by contact with infected electrodes used in a neurosurgical procedure, and by pituitary-derived human growth hormone. In these cases, the incubation period of the disease was ~15-20 months.
Other evidence suggests that a longer latency may follow natural infection. It has been transmitted to chimpanzees, mice, and guinea pigs by inoculation of infected brain tissue, leukocytes, and certain organs. High levels of infectious agent have been found, especially in the brain, where they may reach 107 infectious doses per gram of brain. Nonpercutaneous transmission of disease has not been observed, and there is no evidence of transmission by direct contact or airborne spread.
Clinical Findings
Signs and Symptoms
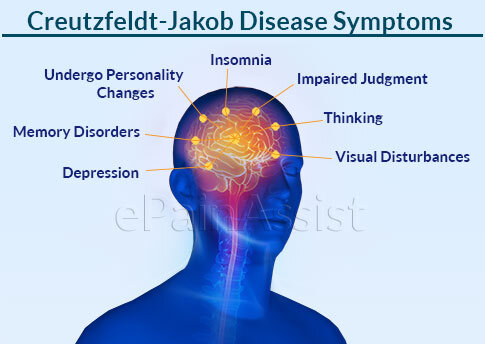
The initial clinical manifestation is a change in cerebral function, usually diagnosed initially as a psychiatric disorder. Forgetfulness and disorientation progress to overt dementia, with the development of changes in gait, increased tone in the limbs, myoclonus, and seizures. The disorder runs a course of 12 months to 4-5 years, eventually leading to death.
Laboratory Findings
Brain biopsy provides definitive diagnosis and includes spongiform degeneration, neuron loss, and astrogliosis. There are also birefringent rods and fibrillar structures similar to those in scrapie. Identification of Creutzfeldt-Jakob prion protein (PrP CjD) by fluorescent antibody directed against it is a useful diagnostic adjunct to neuropathologic examination of brain tissue.
Imaging
EEG is abnormal and characteristic in more than 75% of patients with periodic, symmetric, biphasic or triphasic sharp wavers. Computed tomography (CT) scan or MRI reveals brain atrophy.
Differential Diagnosis
Cases of Creutzfeldt-Jakob disease may resemble PML, but the latter occurs in immunocompromised patients, including those with AIDS, whereas Creutzfeldt-Jakob disease occurs in older, nonimmunocompromised individuals.
Treatment
There is no effective therapy of Creutzfeldt-Jakob disease, and all cases have been fatal.
Prevention
The small risk of nosocomial infection is related only to direct contact with brain tissue. Stereotactic neurosurgical equipment, especially that used in patients with undiagnosed dementia, should not be reused. In addition, organs from patients with undiagnosed neurologic disease should not be used for transplants. Growth hormone from human tissue has now been replaced by a recombinant genetically engineered product. The agent of Creutzfeldt-Jakob disease has not been transmitted to animals by inoculation of body secretions, and no increased risk of disease has been noted in family members or medical personnel caring for patients. Disinfection of potentially infectious material can be accomplished by treatment for 1 h with 0.5% sodium hypochlorite solution or by autoclaving at 121 °C for 1 h.
KURU
Kuru was a subacute, progressive neurologic disease of the Fore people of the Eastern Highlands of New Guinea. In the local Fore dialect, kuru means to tremble with fear or to be afraid. The disease was brought to the attention of the western world by Gadjusek and Zigas in the mid-1950s. Although the illness was localized and decreasing in incidence, its study has thrown light on the infectious nature of similar transmissible encephalopathies. Epidemiologic studies indicated that kuru usually afflicted adult women or children of either sex. The disease was rarely observed outside of the Fore region, and outsiders in the region did not contract the disease. The symptoms and signs were ataxia, hyperreflexia, and spasticity, which led to progressive starvation and death. Mental alertness was unaffected until the late stages of illness.
Pathologic examination revealed changes only in the CNS, with diffuse neuronal degeneration and spongiform changes of the cerebral cortex and basal ganglia. No inflammatory response was noted. Inoculation of infectious brain tissue into primates produced a disease that caused similar neurologic symptoms and pathologic manifestations after an incubation period of approximately 40 months.
Epidemiologic studies indicated that transmission of the disease in humans was associated with ritual cannibalism, practiced mainly by women and young children and occasionally by men. This ritual involved the handling and ingestion of organs of deceased relatives. Inoculation through lesions in the skin and mucous membranes was shown to be the most likely mode of transmission, with clinical disease developing 4-20 years after exposure. Since the elimination of cannibalism from the Fore culture, kuru has disappeared.


