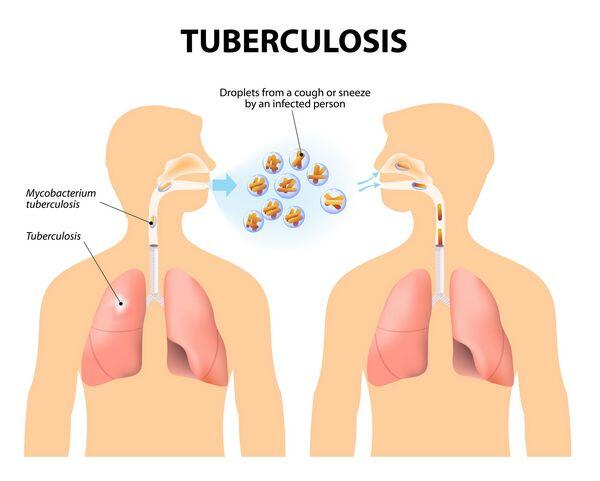
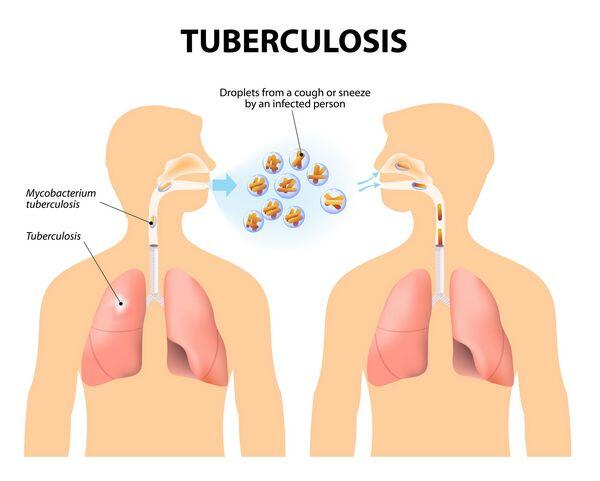
- Tuberculosis is a communicable infectious disease caused by Mycobacterium tuberculosis. It can produce silent, latent infection as well as progressive, active disease.
- Globally, 2 billion people are infected and 2 to 3 million people die from tuberculosis each year.
- M. tuberculosis is transmitted from person to person by coughing or sneezing. Close contacts of Tuberculosis patients are most likely to become infected.
- Fifty-one percent of Tuberculosis patients in the United States are foreign born, most often from Mexico, the Philippines, Vietnam, India, China, Haiti, or South Korea. In the United States, Tuberculosis disproportionately affects ethnic minorities (blacks and Hispanics).
- HIV is the most important risk factor for active Tuberculosis, especially among people 25 to 44 years of age. An HIV-infected individual with tuberculous infection is over 100-fold more likely to develop active disease than an HIV-seronegative patient.
Pathophysiology
- Primary infection is initiated by the alveolar implantation of organisms in droplet nuclei that are small enough (1 to 5 mm) to escape the ciliary epithelial cells of the upper respiratory tract. Once implanted, the organisms multiply and are ingested by pulmonary macrophages, where they continue to multiply, albeit more slowly. Tissue necrosis and calcification of the originally infected site and regional lymph nodes may occur, resulting in the formation of a radiodense area referred to as a Ghon complex.
- Large numbers of activated macrophages surround the solid caseous (cheeselike) tuberculosis foci (the necrotic area) as a part of cell-mediated immunity. Delayed-type hypersensitivity also develops through activation and multiplication of T lymphocytes. Macrophages form granulomas to contain the organisms.
- Successful containment of M. tuberculosis requires activation of a subset of CD4 lymphocytes, referred to as Th-1 cells, which activate macrophages through secretion of interferon Оі.
- Approximately 90% of patients who experience primary disease have no further clinical manifestations other than a positive skin test either alone or in combination with radiographic evidence of stable granulomas.
- Approximately 5% of patients (usually children, the elderly, or the immunocompromised) experience progressive primary disease at the site of the primary infection (usually the lower lobes) and frequently by dissemination, leading to meningitis and often to involvement of the upper lobes of the lung as well.
- Approximately 10% of patients develop reactivation disease, which arises subsequent to the hematogenous spread of the organism.
- Occasionally, a massive inoculum of organisms may be introduced into the bloodstream, causing widely disseminated disease and granuloma formation known as miliary tuberculosis.
| TABLE. Clinical Presentation of Tuberculosis |
Signs and Symptoms
- Patients typically present with weight loss, fatigue, a productive cough, fever, and night sweats
- Frank hemoptysisPhysical Examination
- Dulness to chest percussion, rales, and increased vocal fremitus are observed frequently on ausculationLaboratory Tests
- Moderate elevations in the white blood cell (white blood cell) count with a lymphocyte predominanceChest Radiograph
- Patchy or nodular infiltrates in the apical area of the upper lobes or the superior segment of the lower lobes
- Cavitation that may show air-fluid levels as the infection progresses
|
|
Clinical presentation
NON-HIV-Infected patients
- The clinical presentation of pulmonary Tuberculosis is nonspecific, indicative only of a slowly evolving infectious process.
- Physical examination is nonspecific, suggestive of progressive pulmonary disease.
- Clinical features associated with extrapulmonary Tuberculosis vary depending on the organ system(s) involved but typically consist of slowly progressive compromise of organ function with low-grade fever and other constitutional symptoms.
HIV-Infected patients
- The clinical features of patients with HIV infection who develop Tuberculosis may be markedly different from those classically observed in immunocompetent individuals. (In AIDS patients, Tuberculosis is much more likely to present as the progressive primary form, to involve extrapulmonary sites, and to involve multiple lobes of the lung.
- Tuberculosis in AIDS patients is less likely to involve cavitary disease, be associated with a positive skin test, or be associated with fever.
Diagnosis
Tuberculin skin test
- The most widely used screening method for tuberculous infection is the tuberculin skin test, which uses purified protein derivative. Populations most likely to benefit from skin testing are listed in Table Criteria for Tuberculin Positivity, by Risk Group.
- The Mantoux method of purified protein derivative administration, which is the most reliable technique, consists of the intradermal injection of purified protein derivative containing 5 TU. The test is read 48 to 72 hours after injection by measuring the diameter of the zone of induration.
- Some patients may exhibit a positive test after an initial negative test, and this is referred to as a booster effect.
Symptomatic disease
Confirmatory diagnosis of a clinical suspicion of Tuberculosis must be made via chest x-ray and microbiologic examination of sputum or other infected material to rule out active disease.
| TABLE. Criteria for Tuberculin Positivity, by Risk Group |
| Reaction 5 mm of Induration |
Reaction 10 mm of Induration |
Reaction 15 mm of Induration |
| Human immunodeficiency virus (HIV)-positive persons |
Recent immigrants (i.e., within the last 5 yr) from high prevalence countries |
Persons with no risk factors for Tuberculosis |
| Recent contacts of tuberculosis (Tuberculosis) case patients |
Injection drug users |
|
| Fibrotic changes on chest radiograph consistent with prior Tuberculosis |
Residents and employeesa of the following high-risk congregate settings: prisons and jails, nursing homes and other long-term facilities for the elderly, hospitals and other health care facilities, residential facilities for patients with acquired immunodeficiency syndrome (AIDS), and homeless shelters |
| Patients with organ transplants and other immunosuppressed patients (receiving the equivalent of 15 mg/d of prednisone for 1 month or more)b |
Mycobacteriology laboratory personnel Persons with the following clinical conditions that place them at high risk: silicosis, diabetes mellitus, chronic renal failure, some hematologic disorders (e.g., leukemias and lymphomas), other specific malignancies (e.g., carcinoma of the head or neck and lung), weight loss of 10% of ideal body weight, gastrectomy, and jejunoileal bypass |
| |
Children younger than 4 yr of age or infants, children, and adolescents exposed to adults at high risk |
| a For persons who are otherwise at low risk and are tested at the start of employment, a reaction of 15 mm induration is considered positive. bRisk of Tuberculosis in patients treated with corticosteroids increases with higher dose and longer duration. |
|
Desired outcome
- Rapid identification of new cases of Tuberculosis
- Isolation of the patient with active disease to prevent spread
- Collection of appropriate samples for smears and cultures
- Prompt resolution of signs and symptoms of disease after initiation of treat- ment
- Achievement of a noninfectious state, thus ending isolation
- Adherence to the treatment regimen
- Cure as quickly as possible (generally with at least 6 months of treatment)
Evaluation of therapeutic outcomes and patient monitoring
- Symptomatic patients should be isolated and have sputum samples sent for AFB stains every 1 to 2 weeks until two consecutive smears are negative.
- Once on maintenance therapy, patients should have sputum cultures performed monthly until negative, which generally occurs over 2 to 3 months. If sputum cultures continue to be positive after 2 months, drug susceptibility testing should be repeated and serum drug concentrations should be checked.
- Patients should have blood urea nitrogen, serum creatinine, aspartate transaminase or alanine transaminase, and a complete blood count determined at baseline and periodically, depending on the presence of other factors that may increase the likelihood of toxicity (advanced age, alcohol abuse, and possibly pregnancy). Hepatotoxicity should be suspected in patients whose transaminases exceed 5 times the upper limit of normal or whose total bilirubin exceeds 3 mg/dL. At this point, the offending agent(s) should be discontinued, and alternatives selected.
- Therapy with isoniazid results in a transient elevation in serum transaminases in 12% to 15% of patients and usually occurs within the first 8 to 12 weeks of therapy. Risk factors for hepatotoxicity include patient age, preexisting liver disease, and pregnancy or postpartum state. Isoniazid also may result in neurotoxicity, most frequently presenting as peripheral neuropathy or, in overdose, seizures and coma. Patients with pyridoxine deficiency, such as alcoholics, children, and the malnourished, are at increased risk, as are patients who are slow acetylators of Isoniazid and those predisposed to neuropathy, such as those with diabetes.
- Elevations in hepatic enzymes have been attributed to rifampin in 10% to 15% of patients, with overt hepatotoxicity occurring in less than 1%. More frequent adverse effects of rifampin include rash, fever, and gastrointestinal distress.
- Rifampin’s induction of hepatic enzymes may enhance the elimination of a number of drugs, most notably protease inhibitors. Women who use oral contraceptives should be advised to use another form of contraception during therapy.
- The red colorizing effects of rifampin on urine, other secretions, and contact lenses should be discussed with the patient.
- Retrobulbar neuritis is the major adverse effect noted in patients treated with ethambutol. Patients usually complain of a change in visual acuity and/or inability to see the color green. Vision testing should be performed on all patients who must receive ethambutol for more than 2 months.
- Impairment of eighth cranial nerve function is the most important adverse effect of streptomycin. Vestibular function is most frequently affected, but hearing may also be impaired. Audiometric testing should be performed in patients who must receive streptomycin for more than 2 months. Streptomycin occasionally causes nephrotoxicity.
- The most serious problem with Tuberculosis therapy is nonadherence to the prescribed regimen. The most effective way to ensure adherence is with DOT.