Description of Medical Condition
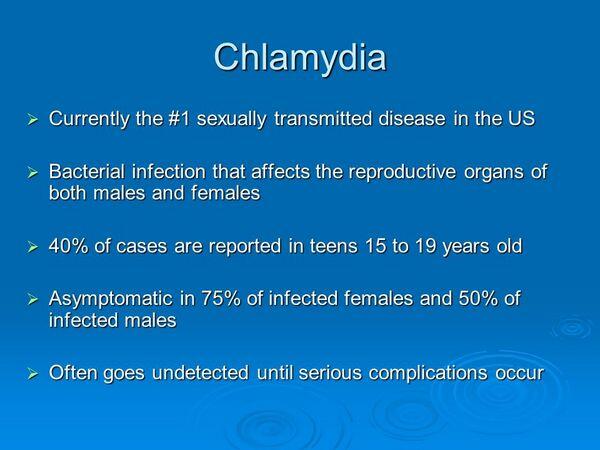
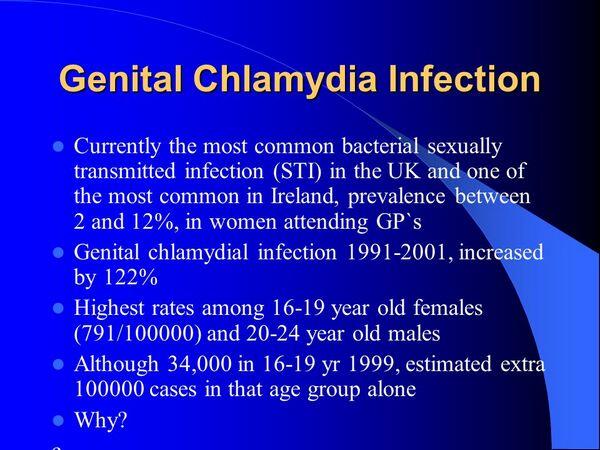
An obligate intracellular membrane-bound prokaryotic organism, chlamydia trachomatis causes an estimated 3 million new sexually transmitted infections in the US each year. The estimated cost of chlamydia STDs in 1994 was $2 billion per year in the U.S., largely due to costly complications such as PID, infertility, and ectopic pregnancy. Studies indicate that 75-90% of women and 50-90% of men with chlamydial STD are asymptomatic. Persons with asymptomatic infection can remain infectious for years. Currently many more women than men are screened, leaving a large male reservoir of infection.
System(s) affected: Reproductive
Genetics: Unknown
Incidence/Prevalence in USA: 3-5% general medical population, 5-15% of teens and young adults, 10-20% STD clinics
Predominant age: 15-25
Predominant sex: Male = Female
Medical Symptoms and Signs of Disease
A substantial majority of cases are asymptomatic. Of those with symptoms, the following are most common:
- Males
- Urethritis
- Epididymitis
- Proctitis OReiter syndrome
- Females
- Cervicitis — typically mucopurulent
- Urethral syndrome
- Bartholinitis
- Endometritis
- Salpingitis/pelvic inflammatory disease (PID)
- Fitz-Hugh-Curtis perihepatitis syndrome
- Infants
- Conjunctivitis
- Pneumonitis
- Carriage-phatynx/GI tract
- Symptoms most strongly associated with chlamydia include urethral or cervical discharge, and pelvic or testicular pain. Persons with such symptoms, or with rectal pain, discharge, ortenesmus, should be tested for chlamydia.
- While chlamydia (and gonorrhea) can cause mucopurulent cervicitis (MPC), these organisms cannot be isolated from most cases of MPC, and most women who have these organisms do not have MPC. Therefore, neither women with mucopurulent cervicitis nor their partners should be treated empirically for chlamydia in the absence of other evidence supporting such treatment.
What Causes Disease?
Chlamydia trachomatis serovars D-K
Risk Factors
- Risk correlates with number of sexual partners
- Risk correlates inversely with age
Diagnosis of Disease
Differential Diagnosis
Neisseria gonorrhea
- Urethritis
- Proctitis
- Epididymitis
- Cervicitis
- PID
- Bartholin’s abscess
- Perihepatitis
Ureaplasma urealyticum
- Urethritis, epididymitis
- Reiter disease
- PID
Chlamydia trachomatis (Serovars LI-3)
- Lymphogranuloma venereum
- Proctitis
Laboratory
- Chlamydial cell culture — sensitivity 50-70%, specificity 100%, takes up to 7 days
- Antigen detection and enzyme immunoassay — sensitivity 50-90%
- Direct fluorescent antibody detection (DFA) — sensitivity =75% in an experienced lab technician’s hands; specificity > 99%
- Amplified molecular testing (e.g., PCR, LCR, SDA, HCS, TMA) — sensitivity = 95%, specificity = 99%, rapid turnaround times, urine or swab specimens, relatively expensive
Drugs that may alter lab results: Amplified molecular tests may remain positive for as long as three weeks after successful treatment
Disorders that may alter lab results: Many amplified molecular tests are not approved for rectal or pharyngeal chlamydia
Pathological Findings
N/A
Diagnostic Procedures
Specimens should contain cell scrapings rather than inflammatory discharge, since the organism lives only inside the epithelial cells
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient, unless moderately or severely ill with PID or other complications
General Measures
- All patients with known or suspected chlamydia should be tested for gonorrhea, syphilis, and HIV (the latter requires individual counseling and consent)
- Some experts recommend that all patients treated for chlamydia should be treated empirically for gonorrhea simultaneously, unless they are known to be negative for gonorrhea by sensitive lab testing
- All partners of patients treated for chlamydia should be tested if possible but treated empirically regardless, rather than waiting for test results
- Some experts recommend treating partners of men being treated for non-specific urethritis, others recommend testing partners and waiting for test results
- Neither women with mucopurulent cervicitis nor their partners should be treated empirically for chlamydia in the absence of other evidence supporting such treatment
Activity
Abstain from sexual contact until diagnosis and treatment complete for patient and all partners
Patient Education
- Risk-reduction counseling
- Safe sex practices, such as barrier protection
- Serious sequelae of chlamydial disease such as tubal infertility, chronic pelvic pain
- Stress need to finish entire course of antibiotics
- For a listing of sources for patient education materials favorably reviewed on this topic, physicians may contact: American Academy of Family Physicians Foundation, P.O. Box 8418, Kansas City, MO 64114. (800)274-2237, ext. 4400
Medications (Drugs, Medicines)
Drug(s) of Choice
Urethritis, cervicitis, sexual partners of infected persons
- Doxycycline -100 mg po bid x 7 days
- Azithromycin -1 gm orally in a single dose
- Pregnant women — erythromycin base, 250 mg po qid x 14 days
Other chlamydial syndromes
- Epididymitis — tetracycline, doxycycline, erythromycin for 10-14 days as above.
- Pelvic inflammatory disease — doxycycline for 10-14 days to cover the chlamydial component of PID (gonorrhea and anaerobic organisms must be treated as well; see CDC recommendations: ceftriaxone 250 mg IM once, cefoxitin, other 3rd generation cephalo-sporin, or a quinolone), erythromycin for 10-14 days may be needed in pregnant or tetracycline intolerant females to treat chlamydial component.
Contraindications: Tetracyclines (e.g., doxycycline) and quinolones (e.g., ofloxacin, levofloxacin) contraindicated in children and pregnant women
Precautions: Tetracyclines: may cause photosensi-tivity; sunscreen recommended
Significant possible interactions:
- Tetracyclines: avoid concurrent administration with antacids, dairy products, or iron
- Broad-spectrum antibiotics: may reduce the effectiveness of oral contraceptives; barrier method recommended
Alternative Drugs
- Erythromycin base 500 mg po qid x 7 days
- Erythromycin ethylsuccinate 800 mg po qid x 7 days
- Ofloxacin 300 mg po bid x 7 days
- Levofloxacin 500 mg po daily x 7 days
Patient Monitoring
- Test of cure is not routine, although it is reasonable to retest persons treated with erythromycin one to two months after treatment
- Sexual partners need to be evaluated and treated empirically if necessary, to prevent passing the disease back and forth between partners. Partnerships with community health departments should be fostered to assist with partner tracing.
- Lack of resolution or recurrence of symptoms must be immediately reported to the physician
- Severe cases of urethritis/cervicitis as well as the chlamydial syndromes should be seen in followup after completion of therapy
- Up to 25% of asymptomatic patients screened for chlamydia may not return for treatment post-chlamydia culture results. Strategies must be developed to ensure treatment can be instituted.
Prevention / Avoidance
Populations with prevalence >5% should be screened at least annually. These include:
Onew or more than one sex partner in last 6 months
- Attending adolescent or family planning clinic
- Attending an STD or abortion clinic
- Attending a jail or other detention center or clinic
- Rectal pain, discharge, ortenesmus
- Testicular pain
- All sexually active woman <25 years old
- Consider for all sexually active men <25 years old (studies are pending)
Only sure way to avoid infection is abstinence, which is not a viable option for many patients. Risk reduction counseling is an effective prevention measure, emphasizing using barrier protection (e.g., condoms) and minimizing the number of different sex partners. Modifiable risk behaviors related to number of sex partners include alcohol or drug use.
Possible Complications
- Enhances transmission of and susceptibility to HI V in both sexes
- Males
- Transient oligospermia
- Post epididymitis urethral stricture (rare)
- Females OTubal infertility
- Tubal pregnancy
- Chronic pelvic pain
Expected Course / Prognosis
Prognosis good with early and compliant therapy. However, due to the asymptomatic nature of early disease and the population affected, symptomatic PID still accounts annually for 2.5 million outpatient visits and more than one quarter million hospitalizations.
Miscellaneous
Associated Conditions
- Pelvic inflammatory disease, epididymitis, cervicitis. urethritis
- Other diseases caused by other chlamydial species:
- Psittacosis — Chlamydia psittaci
- Pneumonia — Chlamydia pneumoniae — Chlamydia trachomatis (infants)
- Lymphogranuloma venereum — Chlamydia trachomatis serovars L1-L3
- Trachoma — Chlamydia trachomatis serovars A-C
Age-Related Factors
Pediatric: N/A
Geriatric: N/A
Others: Prevalence inversely proportional to age (after onset of sexual activity)
Pregnancy
Perinatal acquisition may result in neonatal pneumonia and/or conjunctivitis. Tetracycline and ofloxacin contraindicated in pregnancy; erythromycin or azithromycin should be used in this situation.
International Classification of Diseases
615.9 Unspecified inflammatory disease of uterus, except cervix
616.0 Cervicitis and endocervicitis
616.10 Vaginitis and vulvovaginitis, unspecified
See Also
- Pelvic inflammatory disease (PID)
- Epididymitis
- Cervicitis
- Urethritis
- HIV infection & AIDS
- Gonococcal infections
- Syphilis
Abbreviations
- STD = sexually transmitted disease
- PID = pelvic inflammatory disease
- HIV = human immunodeficiency virus
- MPC = mucopurulent cervicitis



