Description of Medical Condition
The systemic response to infection; it encompasses a broad array of clinical manifestations and overlaps with inflammatory reactions to other clinical insults (e.g., severe trauma or burn)
- Bacteremia: Bacteria in the blood; may have no accompanying symptoms
- Systemic inflammatory response syndrome (SIRS) inflammatory reaction to different clinical insults manifest by two of the following: (1) temperature >38°C or<36°C, (2) heart rate >90/min; (3) respiratory rate >20/min or PaC02 <32 mm Hg, and (4) WBC count >12,000/mm3, <4,000/mm3 or >10% immature forms (bands)
- Sepsis: SIRS with documented infection (typically bacterial)
- Septic shock: Sepsis induced hypotension (systolic BP <90 mmHg or >40 mmHg drop from baseline) despite adequate fluid resuscitation plus hypoperfusion abnormalities (oliguria, lactic acidosis, acute change in mental status)
- Multiple organ dysfunction syndrome (MODS): altered organ function in an acutely ill patient — requires intervention to maintain homeostasis
System(s) affected: Cardiovascular, Endocrine/ Metabolic, Hemic/Lymphatic/lmmunologic, Renal/Urologic, Nervous, Pulmonary, Gastrointestinal Genetics: Single nucleotide polymorphisms i.e., cytokine and cytokine receptor genes influence risk for development of sepsis and risk of mortality from sepsis Incidence/Prevalence in USA: 300/100,000 persons/year Predominant age: All ages Predominant sex: Male> Female (1.28:1)
Medical Symptoms and Signs of Disease
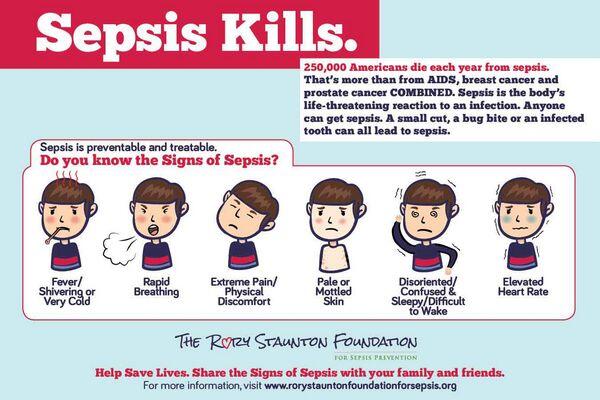
- Fever
- Chills, rigors
- Myalgias
- Changes in mental status — restlessness, agitation, confusion, delirium, lethargy, stupor, coma
- Tachycardia
- Tachypnea
- Hypotension
- Skin lesions — erythema, petechiae, ecthyma gangrenosum, embolic lesions
- Signs and symptoms related to site of primary infection
- Respiratory tract — cough, sputum production, dyspnea, chest pain
- Urinary tract — dysuria, flank pain, frequency, urgency
- Intra-abdominal source — nausea, vomiting, diarrhea, constipation, abdominal pain
- Central nervous system — stiff neck, headache. photophobia, focal neurologic signs
- Signs and symptoms related to end organ failure
- Pulmonary — cyanosis
- Renal — oliguria, anuria
- Hepatic — jaundice
- Cardiac — congestive heart failure

What Causes Disease?
Specific etiologic agents include:
- Gram positive organisms — most commonly Staphylococcus spp, Streptococcus spp. Enterococcus spp
- Gram negative organisms — most commonly Escherichia coli, Klebsiella spp, Proteus spp.,Pseudomonas spp
- Fungi — most commonly Candida spp
- Other agents — anaerobes. Also, see Differential diagnosis.
Common sources of septicemia include
- Lungs
- Urinary tract
- Intra-abdominal focus — biliary tree, abscess, peritonitis
- Intravascular catheters
- Skin — cellulitis, decubitus ulcer, gangrene
- Heart valves
Risk Factors
- Age extremes (very old and very young)
- Impaired host (see associated conditions)
- Indwelling catheters- intravascular, urinary, biliary, etc.
- Complicated labor and delivery — premature and/or prolonged rupture of membranes, etc.
- Certain surgical procedures
Diagnosis of Disease
Differential Diagnosis
- Viral diseases (influenza, dengue and other hemorrhagic viruses, Coxsackie B virus)
- Rickettsial diseases (Rocky Mountain spotted fever, endemic typhus)
- Spirochetal diseases (leptospirosis, relapsing fever [Borrelia sp], Jarisch-Herxheimer reaction in syphilis)
- Protozoal diseases (Toxoplasma gondii, Trypanosoma cruzi, Pneumocystis carinii, Plasmodium falciparum)
- Collagen vascular diseases, vasculitides, myocardial infarction, pulmonary embolus, thromboticthrombocyto-penic purpura/hemolytic-uremic syndrome, thyrotoxico-sis, adrenal insufficiency (Addison disease), dissecting aortic aneurysm, multiple trauma, third-degree burn
Laboratory
- Positive blood cultures
- Positive cultures from other sites (sputum, urine, cerebrospinal fluid [CSF], etc.)
- Gram stain of clinical specimens (sputum, urine, CSF. etc.)
- Common:
- Leukocytosis
- Proteinuria
- Hypoxemia
- Eosinopenia
- Hypoferremia
- Hyperglycemia
- Hypocalcemia
- Mild hyperbilirubinemia
- Less common:
- Lactic acidosis
- Leukopenia
- Azotemia
- Thrombocytopenia
- Prolonged prothrombin time
- Anemia
- Hypoglycemia
Drugs that may alter lab results: Prior antibiotic use Disorders that may alter lab results: N/A
Pathological Findings
- Inflammation at primary site of infection
- Disseminated intravascular coagulation
- Non-cardiogenic pulmonary edema
Special Tests
- Antigen detection systems — counterimmunoelectrophoresis (CIE) and latex agglutination tests (pneumococcus, H. influenzae type B, group B streptococcus, meningococcus)
- Gram stain of buffy coat smears occasionally useful
Imaging
- X-rays (e.g., chest)
- Ultrasound, CT scan, or MRI may be useful in delineating sites of infection
Diagnostic Procedures
- Aspiration of potentially infected body fluids (pleural. peritoneal, CSF) when appropriate
- Biopsy, drainage of potentially infected tissues (abscess, biliary tree, etc.) when appropriate
Treatment (Medical Therapy)
Appropriate Health Care
- Hospitalization
- Intensive care treatment of patients with shock, respiratory failure
General Measures
- Removal or drainage of septic foci
- Correction of metabolic abnormalities (hypoxemia, hyperglycemia, hypoglycemia, severe acidemia [pH < 7.10])
- Mechanical ventilation for respiratory failure
- Transfusion of RBC, platelets, and/or fresh frozen plasma for bleeding
- Volume replacement followed by pressors for hypotension
- Stress ulcer and deep venous thrombosis prophylactic measures
- Insulin therapy to keep serum glucose < 150 mg/dl
Surgical Measures
Drainage of infected sites, debridement of necrotic tissues
Activity
Bedrest
Diet
NPO initially; intravenous hyperalimentation appropriate in some severely malnourished patients and in patients who will be unable to receive enteral alimentation within the week
Patient Education
N/A
Medications (Drugs, Medicines)
Drug(s) of Choice
- Antibiotic coverage should be broad initially and directed against organisms associated with identified septic foci. After culture results are available, treatment should be more organism-specific. Knowledge of the antibiotic susceptibility patterns of local pathogens extremely important.
- Neonatal (< 7 days old) sepsis — ampicillin 300 mg/kg/d in 3 divided doses and gentamicin (Garamycin) 5 mg/kg/d in 2 divided doses
- Non-immunocompromised child — cefotaxime (Claforan) 200 mg/kg/d in 4 divided doses
- Non-immunocompromised adult — cefotaxime (Claforan) 1-2 gm q8-12 orticarcillin-clavulanate (Timentin) 3.1 g q6h plus gentamicin 5 mg/kg/day in 1 -3 divided doses
- Neutropenic host — cefepime (Maxipime) 1 -2 gm q12h, and gentamicin (Garamycin) ortobramycin 3-5 mg/kg/d in 2-3 divided doses; vancomycin (Vancocin) is added when there is an obvious catheter-related infection or a known gram positive bacteremia or if there is an increased likelihood of infection with resistant gram positive organisms.
Contraindications: History of anaphylaxis or other allergic reaction to the antibiotic Precautions: Dose adjustments required in renal failure Significant possible interactions:
- Aminoglycosides — increased nephrotoxicitywith enflurane, cisplatin and possibly vancomycin; increased ototoxidty with loop diuretics; increased paralysis with neuromuscular blocking agents
- Ampicillin — increased frequency of rash with allopurinol
Alternative Drugs
- Intravenous hydrocortisone, 200-300 mg/day in 3-4 divided doses may benefit patients who require vasopressor therapy to maintain an adequate blood pressure. Higher doses of corticosteroids should not be used.
- Many other drug combinations are possible to get adequate coverage
- Antifungals
- Antimicrobials for anaerobic infections
- Antipseudomonals
- Drotrecogin alfa (Xigris) — 24 mcg/kg/hr for 96 hrs in patients with severe sepsis (APACHE score >24). Do not use in patients with increased risk of bleeding, thrombocytopenia with platelets < 30,000, sepsis-induced organ dysfunction for >24 hours, hypercoagu-lable states, chronic renal or hepatic failure, children or pregnancy. Very expensive.
Patient Monitoring
- Depends upon source of infection, underlying disease(s)
- Peak and trough drug levels for aminoglycosides
- BUN, creatinine, electrolytes and complete blood counts at least twice weekly; more frequently if unstable
Prevention / Avoidance
- Vaccination — pneumococcal (geriatric patients, patients with certain chronic diseases), Haemophilus influ-enzae type B (infants, young children)
- Gamma globulin (for hypo- or agammaglobulinemic patients)
- Hand washing by hospital personnel, appropriate catheter care, etc., for hospitalized patients
Possible Complications
- Death
- Adult respiratory distress syndrome (ARDS)
- Multi-organ failure (cardiac, pulmonary, renal, hepatic)
- Disseminated intravascular coagulation (DIC)
- Gastrointestinal hemorrhage
Expected Course / Prognosis
Even with optimal care, mortality will be 10-50% overall; this is increased in patients with neutropenia, diabetes, alcoholism, renal failure, respiratory failure, hypogammaglobulinemia, certain etiologic agents (e.g., Pseudomonas aeruginosa), a delay in appropriate antimicrobial therapy, and those patients at the age extremes
Miscellaneous
Associated Conditions
- Neutropenia
- Diabetes mellitus
- Alcoholism
- Leukemia, lymphoma, and solid tumors
- Cirrhosis
- Burns
- Multiple trauma
- Intravenous drug abuse
- Malnutrition
- Complement deficiencies
- Hypo-oragammaglobulinemia
- Spienectomy
- HIV infection
Age-Related Factors
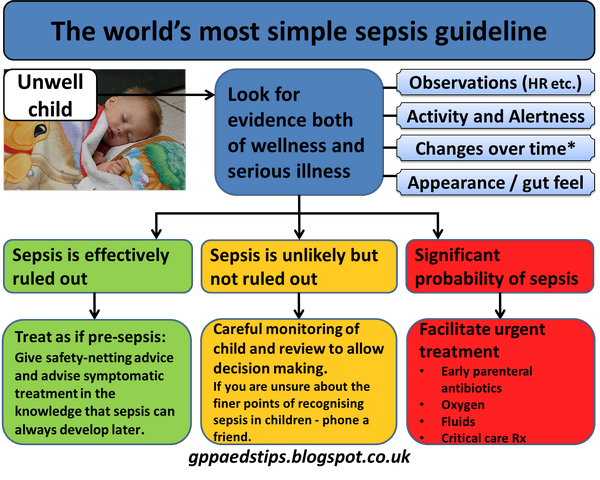
Pediatric: Screen newborns for infection due to prolonged rupture of membranes (> 24 h), maternal fever, prematurity Geriatric:
- Often more difficult to diagnose clinically in the elderly
- Change in mental status/behavior may be only early manifestation
Pregnancy
Beta lactam antibiotics, aminoglycosides, erythromycin are considered safe
Synonyms
- Septicemia
- Sepsis neonatorum
International Classification of Diseases
038.9 Unspecified septicemia
See Also
- Pneumonia, bacterial
- Pyelonephritis
- Meningitis, bacterial
- Endocarditis, infective
- Toxic shock syndrome
- Rocky Mountain spotted fever
- Candidiasis
- Listeriosis
- Tularemia
Other Notes
High dose steroids of no benefit


