Pneumonia is the most common infectious cause of death in the United States. It occurs in persons of all ages, although the clinical manifestations are most severe in the very young, the elderly, and the chronically ill.
Pathophysiology
- Microorganisms gain access to the lower respiratory tract by three routes: they may be inhaled as aerosolized particles; they may enter the lung via the bloodstream from an extrapulmonary site of infection; or aspiration of oropharyngeal contents may occur.
- Lung infections with viruses suppress the bacterial clearing activity of the lung by impairing alveolar macrophage function and mucociliary clearance, thus setting the stage for secondary bacterial pneumonia.
- The vast majority of pneumonia cases acquired in the community by otherwise healthy adults are due to S. pneumoniae (pneumococcus) or M. pneumoniae (up to 70% and 10% to 20% of all acute bacterial pneumonias in the United States, respectively). Other common bacterial causes include Legionella and C. pneumoniae. Community-acquired pneumonias caused by Staphylococcus aureus and gram-negative rods are observed primarily in the elderly, especially those residing in nursing homes, and in association with alcoholism and other debilitating conditions.
- Gram-negative aerobic bacilli and S. aureus are also the leading causative agents in hospital-acquired pneumonia.
- Anaerobic bacteria are the most common etiologic agents in pneumonia that follows the gross aspiration of gastric or oropharyngeal contents.
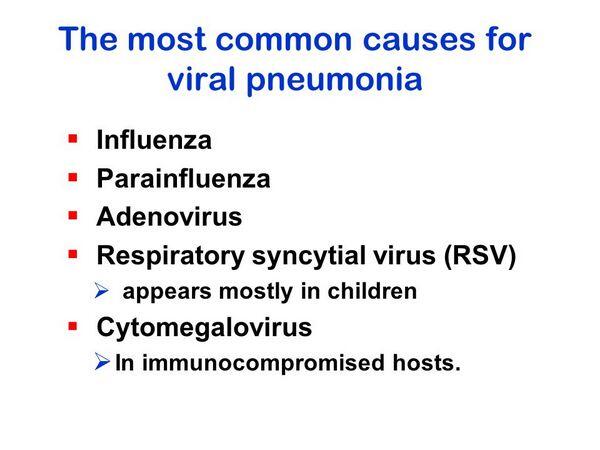
- In the pediatric age group, most pneumonias are due to viruses, especially respiratory syncytial virus, parainfluenza, and adenovirus. Pneumococcus is the most common bacterial cause.
Clinical presentation
Gram-Positive and Gram-Negative Bacterial Pneumonia
See Table Clinical Presentation of Pneumonia.
- Infection with Legionella pneumophila is characterized by multisystem involvement, including rapidly progressive pneumonia. It has a gradual onset, with prominent constitutional symptoms such as malaise, lethargy, weakness, and anorexia occurring early in the course of the illness. A dry, nonproductive cough is initially present that over several days becomes productive of mucoid or purulent sputum. Fevers exceed 40В°C and are typically unremitting and associated with a relative bradycardia. Pleuritic chest pain and progressive dyspnea may be seen, and fine rales are found on lung examination, progressing to signs of frank consolidation later in the course of the illness. Extrapulmonary manifestations remain evident throughout the course of the illness and include diarrhea, nausea, vomiting, myalgias, and arthralgias.
| TABLE. Clinical Presentation of Pneumonia | ||||||||
|
- Substantial changes in a patient’s mental status, often out of proportion to the degree of fever, are seen in approximately one fourth of patients. Obtundation, hallucinations, grand mal seizures, and focal neurologic findings have also been associated with this illness.
- Laboratory findings include leukocytosis with predominance of mature and immature granulocytes in 50% to 75% of patients. Because L. pneumophila stains poorly with commonly used stains, routine microscopic examination of sputum is of little diagnostic value. Fluorescent antibody testing can be performed to diagnose Legionnaires’ disease.
Anaerobic Pneumonia
The course of anaerobic pneumonia is typically indolent with cough, low-grade fever, and weight loss, although an acute presentation may occur. Putrid sputum, when present, is highly suggestive of the diagnosis. Chest radiographs reveal infiltrates typically located in dependent lung segments, and lung abscesses develop in 20% of patients 1 to 2 weeks into the course of the illness.
Mycoplasma pneumoniae
- M. pneumoniae pneumonia presents with a gradual onset of fever, headache, and malaise, with the appearance 3 to 5 days after the onset of illness of a persistent, hacking cough that initially is nonproductive. Sore throat, ear pain, and rhinorrhea are often present. Lung findings are generally limited to rales and rhonchi; findings of consolidation are rarely present.
- Nonpulmonary manifestations are extremely common and include nausea, vomiting, diarrhea, myalgias, arthralgias, polyarticular arthritis, skin rashes, myocarditis and pericarditis, hemolytic anemia, meningoencephalitis, cranial neuropathies, and Guillain-Barr syndrome. Systemic symptoms generally clear in 1 to 2 weeks, while respiratory symptoms may persist up to 4 weeks.
- Radiographic findings include patchy or interstitial infiltrates, which are most commonly seen in the lower lobes.
- Sputum Gram stain may reveal mononuclear or polymorphonuclear leukocytes, with no predominant organism. While M. pneumoniae can be cultured from respiratory secretions using specialized medium, 2 to 3 weeks may be necessary for culture identification.
Viral Pneumonia
- The clinical pictures produced by respiratory viruses are sufficiently variable and overlap to such a degree that an etiologic diagnosis cannot confidently be made on clinical grounds alone. Serologic tests for virus-specific antibodies are often used in the diagnosis of viral infections. The diagnostic fourfold rise in titer between acute and convalescent phase sera may require 2 to 3 weeks to develop; however, same-day diagnosis of viral infections is now possible through the use of indirect immunofluorescence tests on exfoliated cells from the respiratory tract.
- Radiographic findings are nonspecific and include bronchial wall thickening and perihilar and diffuse interstitial infiltrates.
Nosocomial Pneumonia
- The strongest predisposing factor for nosocomial pneumonia is mechanical ventilation. Risk is increased by prior antibiotic use, use of H2-receptor antagonists, and severe illness.
The diagnosis of nosocomial pneumonia is usually established by presence of a new infiltrate on chest radiograph, fever, worsening respiratory status, and the appearance of thick, neutrophil-laden respiratory secretions.
Desired outcome
- Eradication of the offending organism and complete clinical cure are the primary objectives.
- Associated morbidity should be minimized (e.g., renal, pulmonary, or hepatic dysfunction).
Treatment
- The first priority on assessing the patient with pneumonia is to evaluate the adequacy of respiratory function and to determine whether there are signs of systemic illness, specifically dehydration or sepsis with resulting circulatory collapse.
- The supportive care of the patient with pneumonia includes the use of humidified oxygen for hypoxemia, fluid resuscitation, administration of bronchodilators when bronchospasm is present, and chest physiotherapy with postural drainage if there is evidence of retained secretions.
- Important therapeutic adjuncts include adequate hydration (by intravenous route if necessary), optimal nutritional support, and fever control.
- The treatment of bacterial pneumonia initially involves the empiric use of a relatively broad-spectrum antibiotic (or antibiotics) effective against probable pathogens after appropriate cultures and specimens for laboratory evaluation have been obtained. Therapy should be narrowed to cover specific pathogens once the results of cultures are known.
- Appropriate empiric choices for the treatment of bacterial pneumonias relative to a patient’s underlying disease are shown in Table Empirical Antimicrobial Therapy for Pneumonia in Adultsa for adults and Table Empirical Antimicrobial Therapy for Pneumonia in Pediatric Patientsa for children. Dosages for antibiotics to treat pneumonia are provided in Table Antibiotic Doses for the Treatment of Bacterial Pneumonia.
| TABLE. Empirical Antimicrobial Therapy for Pneumonia in Adultsa | ||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
- Antibiotic concentrations in respiratory secretions in excess of the pathogen minimum inhibitory concentration (minimum inhibitory concentration) are necessary for successful treatment of pulmonary infections.
- Drugs recommended for empiric treatment of community-acquired pneumonia are presented in Table Guidelines for the Empirical Treatment of Community-Acquired Pneumonia.
- The benefit of antibiotic aerosols or direct endotracheal instillation has not been consistently demonstrated.
- Prevention of pneumonia is possible through the use of vaccines against S. pneumoniae and H. influenzae type b. In addition, amantadine may be administered for prevention of influenza A infection, beginning as soon as possible after exposure and continuing for at least 10 days.









