Description of Medical Condition
Atelectasis (lung collapse) is a portion of lung which is non-aerated, but otherwise normal. May be an asymptomatic finding on CXR or associated with symptoms. Pulmonary blood flow to area of atelectasis is usually reduced, thereby limiting shunting and hypoxia. Diagnosis and therapy are directed at basic cause.
System(s) affected: Pulmonary, Cardiovascular
Genetics: Depends on basic condition e.g., cystic fibrosis, COPD, asthma, congenital heart disease, congestive heart failure, etc.
Incidence/Prevalence in USA: Common in general anesthesia and in intensive care with high inspired oxygen concentrations
Predominant age: All ages
Predominant sex: Male = Female
Medical Symptoms and Signs of Disease
- Small atelectasis
- Commonly asymptomatic
- Produces no change in the overall clinical presentation
- Large atelectasis:
- Tachypnea
- Cough
- Hypoxia which resolves in some cases over 24-48 hours — due to ventilation — periusion mismatch
- Dullness to percussion
- Absent breath sounds if airway is occluded
- Bronchial breathing if airway is patent
- Diminished chest expansion
- Tracheal or precordial impulse displacement
- Wheezing may be heard with focal obstruction
What Causes Disease?
- Increased alveolar surface tension due to cardiogenic or non-cardiogenic pulmonary edema, primary surfactant deficiency, or infection
- Resorptive atelectasis due to airway obstruction from lumenal blockage (mucus, tumor, foreign body), airway wall abnormality (edema, tumor, bronchomalacia, deformation), or extrinsic airway compression (cardiac, vascular, tumor, adenopathy)
- Compression of the lung (lobar emphysema, cardiomegaly, tumor)
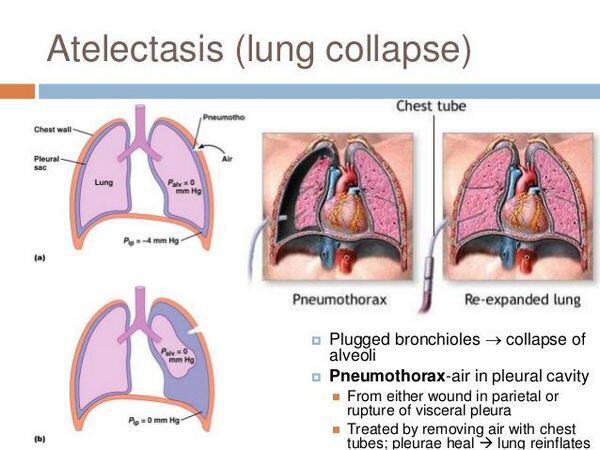
- Increased pleural pressure due to fluid or air in the pleural space (pneumothorax, effusion, empyema. hemothorax, chylothorax)
- Chest wall restriction due to skeletal deformity and/or muscular weakness (scoliosis, neuromuscular disease, phrenic nerve paralysis, anesthesia)
Risk Factors
- Varies with condition producing atelectasis
- Atelectasis following anesthesia is increased in smokers, obese individuals, and individuals with short, wide thoraces
- Asthma — right middle lobe most common
Diagnosis of Disease
Differential Diagnosis
- Atelectasis is not a specific diagnosis, but rather a result of disease or distorted anatomy. The differential is thus found under Causes.
- The roentgenographic differential includes pneumonia, fluid accumulation, lung hypoplasia, or tumor
Drugs that may alter lab results: N/A
Disorders that may alter lab results: N/A
Pathological Findings
- Pathology varies with cause
- Obstructive atelectasis — non-aerated lung without inflammation or infiltration
Imaging
CXR
- May demonstrate linear, round, or wedge shaped densities
- Right middle lobe and lingular atelectasis will obscure the ipsilateral heart border
- Lower lobe atelectasis will obscure the diaphragm
- Air bronchograms are usually absent in obstructive atelectasis
- Evidence of possible airway compression, pleural fluid or air should be sought
- Diffuse microatelectasis in surfactant deficiency may lead to a ground-glass appearance with striking air bronchograms
- Mediastinal structures and the diaphragm move toward the atelectatic region
- Adjacent lung may show compensatory hyperinflation
Diagnostic Procedures
- Bronchoscopy to assess airway patency. (Bronchos-copy as therapy is controversial with the exception of foreign body or other structural causes).
- Echocardiography to assess cardiac status in cardio-megaly
- Chest CT or MRI to visualize airway and mediastinal structures
- Barium swallow to assess mediastinal vascular compression
- Other procedures vary with potential cause
Treatment (Medical Therapy)
Appropriate Health Care
Varies with severity
General Measures
- Varies with severity and cause of atelectasis
- Maximize patient mobility
- Ensure adequate oxygenation and humidification
- Chest physiotherapy with percussion and postural drainage. Consider adding treatments using new airway clearance techniques such as Positive Expiratory Pressure (PEP) mask.
- Incentive spirometry
- Positive pressure ventilation or continuous positive airway pressure in subjects with neuromuscular weakness. In-exsufflator may also be helpful here.
Activity
Encourage activity, mobilization as tolerated
Diet
No special diet
Patient Education
Encourage activity as appropriate. Instruct in basic cause and its therapy.
Medications (Drugs, Medicines)
Drug(s) of Choice
- Bronchodilator therapy (beta-agonist aerosol); efficacy controversial
- Other therapies directed at basic cause — antibiotics, foreign body removal, tumor therapy, cardiac medication, steroids in asthma
Contraindications: Refer to manufacturer’s literature
Precautions: Refer to manufacturer’s literature
Significant possible interactions: Refer to manufacturer’s literature
Alternative Drugs
N/A
Patient Monitoring
- Varies with cause and patient status
- In simple atelectasis associated with asthma or infection, monthly visits are adequate
Prevention / Avoidance
- Avoidance of 100% inspired oxygen (which can rapidly absorb causing atelectasis)
- Foreign body/aspiration precautions
- Postoperative mobilization and/or rotation
- Institute therapies such as chest physiotherapy and incentive spirometry as preventive maneuvers in at-risk patients
Possible Complications
- Infection with chronic lung damage is an unlikely, but unfortunate complication
- Atelectasis is rarely life-threatening and usually spontaneously resolves
Expected Course / Prognosis
- Resolution with medical therapy
- Surgical therapy needed only for certain causes, or if chronic infection and bronchiectasis supervene
Miscellaneous
Associated Conditions
N/A
Age-Related Factors
Very young and very old patients with limited mobility at greater risk
Pediatric: Congenital airway obstruction due to mediastinal cysts, tumor, or vascular rings; foreign body aspiration
Geriatric: Primary and secondary lung tumors sometimes associated
Others: Asthma
Pregnancy
Management is similar to non-pregnant and varies with cause
Synonyms
Lung collapse
International Classification of Diseases
518.0 Pulmonary collapse
See Also
Asthma
Pneumonia, viral Pneumonia, bacterial Pneumonia, mycoplasma
Other Notes
Round atelectasis:
- A pleural based round density on CXR with a comet tail of vessel and airway
- More common in patients with asbestos exposure
- May mimic tumor, but can usually be definitively diagnosed with imaging studies thereby avoiding surgery


