Clinical Findings
Signs and Symptoms
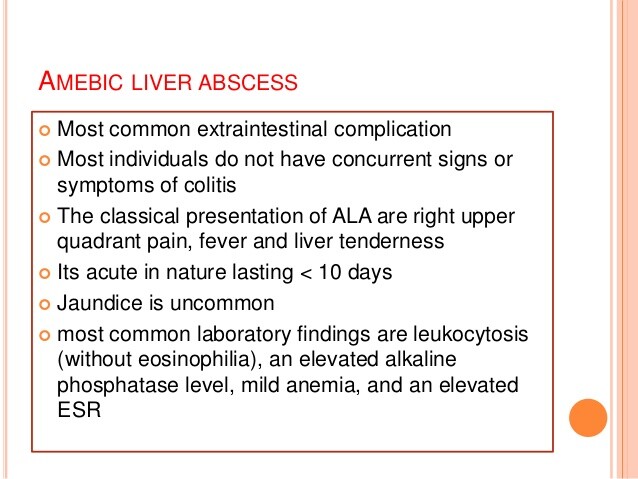
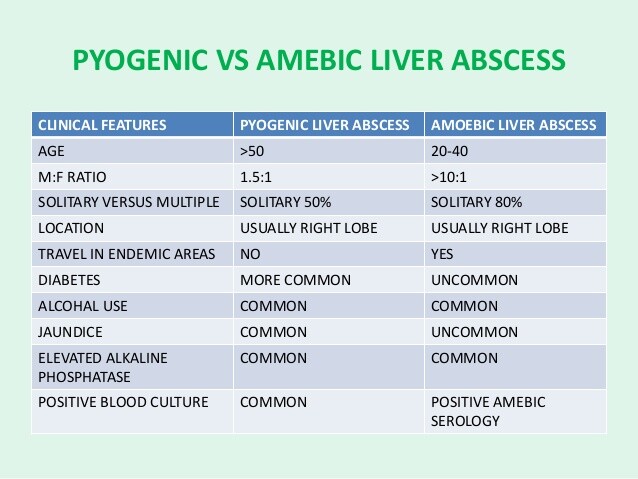
Amebic liver abscess is the most common extraintestinal manifestation of amebiasis. Patients may note right-upper-quadrant pain that is either dull or pleuritic in nature. Often pain is referred to the right shoulder. Less than 50% of patients have an enlarged liver. In the acute setting, patients typically manifest fever. If symptoms have been present for > 2 weeks, fever is present in less than half of patients. Respiratory symptoms, such as cough, can occur even in the absence of pulmonary disease and may be the only complaint. In the subacute setting, weight loss is common. Diarrhea is found in less than one-third of patients with amebic liver abscess.
Exam may reveal abdominal tenderness, tender hepatomegaly, and crackles at the right lung base. Jaundice is uncommon.
Laboratory Findings
Patients with amebic liver abscess may have leukocytosis without eosinophilia, elevated alkaline phosphatase, and mild anemia. The transaminases are elevated in severe disease. Other findings include a high erythrocyte sedimentation rate and proteinuria.
Imaging
Ultrasound of the liver may show a round or an oval hypoechoic area contiguous with the liver capsule and without significant wall echoes. This is often a single lesion in the right hepatic lobe. Computer tomographic scanning and magnetic resonance imaging are sensitive studies for hepatic involvement, but the finding of a mass is not specific for amebic abscess. Each of these studies allows definition of the number of lesions as well as their size, and this information may be used to monitor a patient’s course.
Differential Diagnosis
An amebic liver abscess needs to be differentiated from other mass lesions of the liver, which include bacterial abscess, echinococcal cyst, hepatoma, and metastatic cancer.
Complications
Amebic liver abscesses may rupture and thereby extend into surrounding tissues, including the pleural space, lung parenchyma, and pericardium. Pleural effusion may be present without frank rupture of the abscess.
Pleuropulmonary amebiasis. Pleuropulmonary disease is the most common complication of amebic liver abscess and usually presents with cough and pleuritic chest pain. Findings may reveal serous effusion, which does not imply disseminated disease. Amebic empyema, with “anchovy paste” material present upon drainage, occurs with rupture of the abscess into the pleural space and has an increased mortality. Consolidation of the lung parenchyma may occur with contiguous spread from a liver abscess. A patient who develops a hepatobronchial fistula will have a cough productive of large amounts of sputum and necrotic material, with the sputum possibly containing detectable amebas.
Peritoneal amebiasis. Peritoneal amebiasis occurs in 2-7% of patients with amebic liver abscess and represents the second most common complication of amebic liver abscess. Presentation may be dramatic enough to simulate a perforated viscus or may be more indolent with a slow leak of organisms into the peritoneal space.
Pericardial amebiasis. Pericardial disease is a rare but serious complication of amebic liver abscess. It usually results from the rupture of an abscess in the left lobe of the liver and presents with fever and chest pain and progresses to congestive heart failure, tamponade, and shock.
Cerebral amebiasis. Cerebral amebiasis is rare, with reports from clinical series of < 0.1% of patients. Autopsy series of patients with known amebiasis show central nervous system involvement of 1-2%. Cerebral abscess should be suspected in a person with known amebiasis who presents with mental status changes or focal neurologic signs.
Genitourinary amebiasis. Renal infection may occur either from direct extension of hepatic disease or by hematogenous or lymphatic spread. Genital lesions typically arise from fistulae from hepatic or colonic disease and present with painful ulcers with profuse discharge.
Diagnosis
The diagnosis of intestinal infection with E histolytica or E dispar is made by demonstration of cysts or trophozoites in the stool or by examination of biopsy specimens of mucosal tissue. Amebic trophozoites are destroyed by many agents, including antibiotics, antidiarrheal agents, barium, and tap water. Therefore, stool specimens should be examined by preparing wet mounts of specimens within 20 min of collection and examining immediately. Staining with iodine and trichrome maximizes the yield of positive specimens. Pathogenic trophozoites of E histolytica may be distinguished from nonpathogenic species by the presence of ingested erythrocytes within the organism.
Serology is useful in diagnosis of E histolytica infection. Antibodies to ameba develop only with infection by E histolytica and do not develop with E dispar infection. With invasive colitis or hepatic abscess, antibodies may be negative initially but become positive by 7-10 days in > 85-95% of patients. Antibodies cannot distinguish current infection from remote infection, as the antibodies may remain positive for years.
Monoclonal antibodies and polymerase chain reaction technology are newer technologies being used for diagnosis of amebic infection and appear to allow differentiation of E histolytica from E dispar. An enzyme-linked immunoabsorbent assay with monoclonal antibodies to a region that contains epitopes unique to E histolytica has been used to make this distinction in preliminary studies.
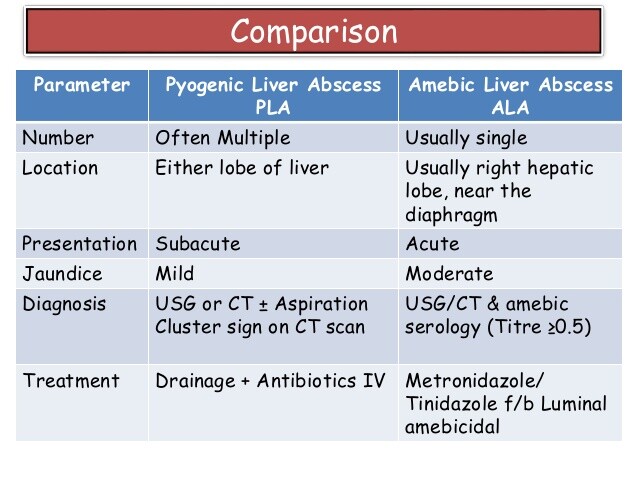
Amebic liver abscess should be suspected in any patient with an abnormal abdominal exam and appropriate risk factors, such as recent travel to an endemic area. Once a hepatic fluid collection is demonstrated radiographically, it is important to distinguish amebic abscess from pyogenic abscess. Serology once again is useful but may be negative for the first week of the infection. Often, percutaneous sampling of the fluid is required to look for cysts and trophozoites. Amebas may not be found in the liquefaction center of an abscess, but the results of Gram stain, culture, and serology will usually distinguish amebic abscess from other causes.
Diagnosis of other extraintestinal sites of infection requires clinical suspicion in the appropriate setting, such as a patient with known amebic abscess. Demonstration of amebas in these extrahepatic sites is not universally required but is often obtained, because drainage is required for empyema, peritoneal involvement, and, usually, pericardial involvement.
Treatment
Treatment of amebic disease requires both the elimination of the trophozoite form from the intestine or extraintestinal sites and the elimination of cysts from the intestine. If a luminal agent is not used to eradicate cysts, disease may recur.
Metronidazole is the agent of choice for treatment of amebic colitis. Doses of 750 mg three times daily for 5-10 days are extremely effective, and the drug can be given orally or intravenously. Side effects are generally gastrointestinal: nausea, vomiting, and abdominal discomfort. If ingested with alcohol, metronidazole produces a disulfiram-like reaction. The drug carries a potential risk of teratogenicity if used in pregnant women; however, because amebic disease is often more serious in pregnant women, treatment is generally recommended. No teratogenic effects were seen in > 2500 women inadvertently given metronidazole during pregnancy. In Europe, two additional nitroimidazole antibiotics (tinidazole and ornidazole) are available, are effective therapy, and are associated with fewer adverse effects than metronidazole. These drugs are not available in the United States.
Tetracycline or erythromycin is effective therapy for milder cases of colitis. Because these drugs will not eradicate ameba in the liver, their use should probably be restricted to patient who cannot tolerate metronidazole. Emetine and dehydroemetine have relatively high toxicity and must be given in a monitored environment. They offer no benefit over standard metronidazole therapy.
Three luminal agents are available for eradication of cysts after treatment with metronidazole or other agents. Diloxanide furoate has a > 90% efficacy but must be obtained from the Centers for Disease Control and Prevention in the United States. Iodoquinol (diiodohydroxyquin) requires 20 days of therapy and is in limited supply in the United States. Because of its high iodine content, it may interfere with thyroid function tests and should be avoided in those allergic to iodine. Other side effects include gastrointestinal discomfort, fever, and headache. Paromomycin is a nonabsorbable aminoglycoside that may cause loose stools. It is often preferred for circumstances in which systemic absorption is undesirable, such as in pregnancy.
Amebic liver abscess is responsive to medical therapy, and, as with intestinal disease, metronidazole is the preferred agent. Given as a 5- to 10-day treatment, metronidazole has a cure rate of > 95%. The role of aspiration or drainage is unclear but usually is not necessary. Because of the high response rate to medical therapy, aspiration is probably best used only in a few defined circumstances. In the patient who is not clinically improved within 3 days of initiation of therapy, aspiration is used to confirm the diagnosis and to exclude other causes of abscess, such as bacterial infection. Aspiration is also indicated for a ruptured abscess and in an abscess that is in danger of rupture, as characterized by a large fluid collection surrounded by a thin rim of hepatic tissue. If a left-lobe abscess is in danger of involving the pericardium, aspiration should be performed.
Medical therapy is generally sufficient for amebiasis involving the genitourinary tract, central nervous system, and lung parenchyma. Involvement of the pericardium and pleural space may require drainage because of the development of loculations. Treatment of amebiasis is outlined in Boxes 82-2 and 82-3.
Prognosis
Although infection with E histolytica can be debilitating, it is generally not life threatening. Once infection is identified, effective treatment exists. Relapse or reinfection is not unusual. Only a small minority of patients develops severe complications, such as colonic perforation, toxic megacolon, ruptured hepatic abscess, or cerebral amebiasis.
Prevention & Control
Prevention of amebic infection is greatly enhanced by effective sanitation and a clean water supply. Cysts are resistant to destruction by chlorine, but iodine or boiling is sufficient to kill the organism. Health education and public health efforts to identify and treat carriers may limit disease spread (Box 4). Travelers to endemic areas should avoid unpeeled fruits and vegetables and should avoid drinking water unless it has been properly treated. Several vaccines to E histolytica are under development and may provide the most effective means of disease control once released.