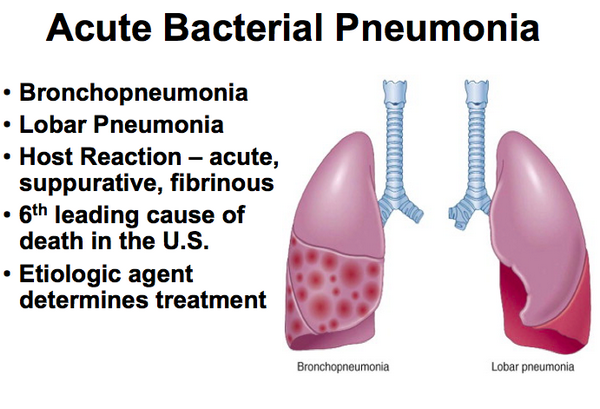
Description of Medical Condition
An acute, bacterial infection of the lung parenchyma. Infection may be community-acquired or nosocomial (hospital acquired by an inpatient for at least 48 hours or inpatient in the previous 90 days). Most commonly, community-acquired disease is caused by Streptococcus pneumoniae or Mycoplasma pneumoniae. Hospital-acquired pneumonia is usually due to gram negative rods (60%, such as Pseudomonas) or Staphylococcus (30%).
System(s) affected: Pulmonary
Genetics: No known genetic pattern
Incidence/Prevalence in USA:
- Incidence-community-acquired: 1200 cases/100,000 population per year
- Incidence — nosocomial: 800 cases/100,000 admissions per year
Predominant age: Age extremes
Predominant sex: Male > Female
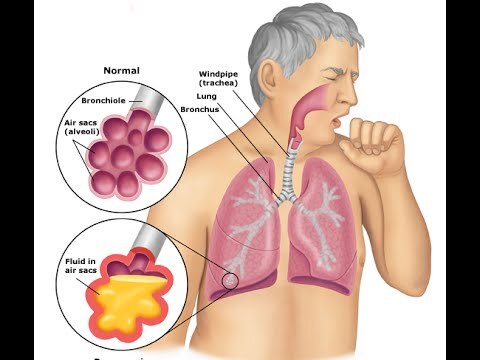
Medical Symptoms and Signs of Disease
- Cardinal signs and symptoms
- Cough and fever
- Chest pain (pleuritic)
- Chill, with sudden onset
- Dark, thick or bloody (rusty) sputum
- Respiratory
- Signs of consolidation
- Rales
- Egophony
- Signs of pleural involvement
- Decreased breath sounds
- Dullness to percussion
- Friction rub
- Signs of respiratory distress
- Tachypnea/tachycardia (or bradycardia)
- Cyanosis
- Central nervous system
- Mentation changes to include anxiety, confusion and restlessness
- Gastrointestinal
- Abdominal pain
- Anorexia
What Causes Disease?
- Sources
- Aspiration from the oropharynx
- Inhalation
- Hematogenous spread
- Bacterial pathogens
- Streptococcus pneumoniae (pneumococcus)
- Haemophilus influenzae
- Mycoplasma pneumoniae
- Staphylococcus aureus
- Legionella pneumophila
- Chlamydia pneumoniae, C. psittaci
- Moraxella catarrhalis (Branhamella catarrhalis)
- Pseudomonas aeruginosa
- Klebsiella pneumoniae (and other gram-negative rods)
- Anaerobes
Risk Factors
- Tobacco smoking
- Recent/concurrent viral infections
- Hospitalization to include mechanical ventilation, antecedent antibiotics, NG tubes
- Age extremes
- Alcoholism
- AIDS or other immunosuppression
- Renal failure
- Cardiovascular disease
- Functional asplenia
- Chronic obstructive pulmonary disease
- Diabetes mellitus
- Malnutrition
- Malignancy
- Altered level of consciousness or gag (e.g., seizures, stroke, neuromuscular disease, etc.)
- Occupational exposure
- Poorly implemented infection control practices (poor handwashing)
- Postoperative atelectasis
Diagnosis of Disease
Differential Diagnosis
Other causes of infectious pneumonitis: Viruses (human metapneumovirus, SARS coronavirus, respiratory syncytial, adenovirus, CMV, parainfluenza, influenzae A and B, varicella, measles, rubella, hantavirus); Nocardia; Fungi (Blastomyces, Cryptococcus, Aspergillus, Histoplasma, Coccidioides, Pneumocystiscarinii); Protozoans (Toxoplasma); Rickettsia (Coxiella burnetii — Q fever). Also tuberculosis, pulmonary embolism with infarction, bronchiolitis obliterans with organizing pneumonia (BOOP), pulmonary contusion, pulmonary vasculitis, acute sarcoid, hypersensitivity pneumonitis, ARDS, pneumothorax, and other causes.
Laboratory
- CBC — leukocytosis with an immature shift on differential; ESR, CRP
- Chem — hyponatremia (SIADH)
- ABG — hypoxemia
- ABG — hypocapnia initially, then hypercapnia
- Blood culture — positive in 10-20% of adult patients and 7% of pediatric patients with community-acquired pneumonia (partially because many have been pre-treated with antibiotics), 8-20% nosocomial pneumonia
Drugs that may alter lab results: Antecedent antibiotics
Disorders that may alter lab results: Refer to lab test reference
Pathological Findings
- Lung:
- Segmental, lobar, or multifocal peribronchial consolidation
- Positive gram stain for bacteria
Special Tests
- Decubitus CXR to investigate for empyema or parapneumonic effusion
- Gram stain and culture of pleural fluid
- pH of pleural fluid (iced, airless sample sent to blood gas laboratory)
- Urine legionella antigen (in ICU/severe cases
- Tuberculin skin test (PPD) — for hilar adenopathy or upper lobe involvement
Imaging
- CXR (with lateral decubitus views if pleural effusion present)
- Lobar or segmental consolidation (air bronchogram)
- Bronchopneumonia
- Interstitial infiltrate
- Pleural effusion (free-flowing or loculated)
- Ultrasound recommended to check for location and presence of loculations before thoracentesis
Diagnostic Procedures
- Gram stain and culture of sputum (induced, if necessary)
- Nasotracheal suctioning for culture
- Transtracheal aspirate for culture
- Bronchoscopy with bronchoalveolar lavage or protected telescoping catheter brushing for culture
- Thoracentesis for pleural fluid studies
- Blood culture, especially if hospitalized — prior to antibiotics
Treatment (Medical Therapy)
Appropriate Health Care
- Community-acquired — outpatient for mild case, inpatient for moderate to severe case such as hypoxemia, altered mental status, hypotension, significant co-morbid illness, and age extremes.
- Nosocomial — patients already hospitalized
General Measures
- Empiric antimicrobial therapy for most likely pathogen(s)
- Consider oxygen for patients with cyanosis, hypoxia, dyspnea, circulatory disturbances or delirium
- Mechanical ventilation for respiratory failure
- Hydration
- Analgesia for pain
- Electrolyte correction
- Respiratory isolation if TB is a possibility
Activity
Bedrest and/or reduced activity during acute phase
Diet
- Nothing by mouth if there is incipient respiratory failure
- Consider soft, easy-to-eat foods
Medications (Drugs, Medicines)
Drug(s) of Choice
Initial therapy
- Usually empiric for most likely pathogens given clinical scenario (if specific etiology is identified, adjust antimicrobial therapy)
- Otherwise healthy young adult with mild community-acquired pneumonia: erythromycin 500 po q6h; in those intolerant of erythromycin and in smokers [to treat H. influenzae], consider the new macrolides or doxycycline 1OOmg bid
- Older patients or patients with preexistent illnesses, with mild community-acquired pneumonia: pneumococcal-active fluoroquinolone, telithromycin or amoxicillin-clavulanate with erythromycin or other macrolide
- Patients with community-acquired pneumonia requiring hospitalization: a specific cephalosporin (cefotaxime, ceftriaxone or cefuroxime) or ampicillin-sulbactam plus macrolide; or a pneumococcal-active fluoroquinolone alone
- For nosocomial pneumonia: either ceftazidime or an antipseudomonal penicillin (piperacillin, orticarcillin) plus an aminoglycoside. Vancomycin should be considered if strong suspicion of Staphylococcus aureus.
Therapy for specific organisms
- S. pneumoniae: penicillin G or oral amoxicillin. If high incidence of penicillin resistant S. pneumoniae in the area, consider pneumococcal-active fluoroquinolone or telithromycin
- H. influenzae: trimethoprim-sulfamethoxazole. For severe infections — cefotaxime, ceftriaxone, or carbapenems
- S. aureus: nafcillin or vancomycin (if high incidence of methicillin resistant S. aureus)
- Klebsiella species: carbapenems or 3rd generation cephalosporin
- Pseudomonas: aminoglycoside plus antipseudomonal penicillin or ceftazidime
Moraxella catarrhalis: 2nd generation cephalosporin (cefuroxime axetil) or B-lactam/B-lactamase inhibitors
- Chlamydia pneumoniae: doxycycline, fluoroquinolone
- Mycoplasma pneumoniae: doxycycline
- Legionella pneumophila: fluoroquinolone or azithromycin
- Anaerobes: clindamycin or B-lactam/B-lactamase inhibitors
Contraindications: Allergy or likely cross-allergy to the prescribed antibiotic
Precautions: Possible significant sodium overload with antipseudomonal penicillins
Significant possible interactions: Refer to manufacturer’s literature
Alternative Drugs
- S. pneumoniae: macrolide, doxycycline; cefotaxime. ceftriaxone or cefuroxime, linezolid, telithromycin
- H. influenzae: cefuroxime; fluoroquinolones; extended macrolides; beta-lactam/beta-lactamase inhibitor, telithromycin
- S. aureus: a first generation cephalosporin; clindamycin; linezolid
- Klebsiella: fluoroquinolone
- Pseudomonas: carbapenems, aztreonam, cefepime
- Moraxella catarrhalis: trimethoprim- sulfamethoxazole; fluoroquinolone; cefixime, extended macrolide; telithromycin
- Chlamydia pneumoniae: clarithromycin; azithromycin; erythromycin; telithromycin
- Mycoplasma pneumoniae: clarithromycin; erythromycin; azithromycin or fluoroquinolone; telithromycin
- Legionella pneumophila: clarithromycin; erythromycin; doxycycline
Patient Monitoring
- If outpatient therapy, daily assessment of the patient’s progress, and reassessment of therapy if clinical worsening or no improvement in 48-72 hours
- CXR take time to clear and may not show clearing, even though patient is improving. Repeat study about 6 weeks after recovery to verify the pneumonia was not caused by an obstructing endobronchial lesion in selected patients (smokers and older patients).
- Repeating the cultures after treatment has been started is unnecessary unless there has been treatment failure or if treating TB
Prevention / Avoidance
- Reduce risk factors where possible (quit smoking)
- Bedridden and postoperative patients — deep breathing and coughing exercises; prevent aspiration during nasogastric tube feedings
- Avoid indiscriminate use of antibiotics during minor viral infections
- Annual influenza vaccine for high risk individuals
- Polyvalent pneumococcal vaccine
Possible Complications
- Empyema
- Pulmonary abscess
- Superinfections
- Multiple organ dysfunction syndrome (MODS)
- Adult respiratory distress syndrome (ARDS)
- Post-pneumonic atelectasis may occur in 5-10% of children
Expected Course / Prognosis
- Usual course — acute. In otherwise healthy individual, improvement seen and fever resolved in 1-3 days; sometimes up to 1 week
- Overall attributable mortality is about 5% in community acquired; (=15% if hospitalized and < 1% if not hospitalized) 25-50% in nosocomial • Poorest prognosis — age extremes, positive blood cultures, low WBC, presence of associated disease, immunosuppression respiratory failure, inappropriate antecedent antibiotics, delayed treatment >8 hours
Miscellaneous
Associated Conditions
- Tobacco smoking
- Alcoholism
- Upper respiratory infection
Age-Related Factors
Pediatric: Morbidity and mortality high in children under age 1
Geriatric: Morbidity and mortality high if > 70, especially with associated disease or risk factor
Pregnancy: N/A
Synonyms
- Lobar pneumonia
- Classic pneumococcal pneumonia
International Classification of Diseases
481 Pneumococcal pneumonia [Streptococcus pneumoniae pneumonia]
486 Pneumonia, organism unspecified
See Also
Pneumonia, viral Pneumonia, mycoplasma Rhodococcus infections
Other Notes
Pneumococcal vaccine for all adults over age 65 and children over 2 years (and adults) with risk (cardio, pulmonary or metabolic disorders); strongly consider in all adults age 50 and older.



