Description of Medical Condition
Single or multiple abscesses within the brain, usually occurring secondary to a focus of infection outside the central nervous system. May mimic brain tumor but evolves more rapidly (days to a few weeks). It starts as a cerebritis, becomes necrotic, and subsequently becomes encapsulated.
System(s) affected: Nervous
Genetics: No known genetic pattern
Incidence/Prevalence in USA: Infrequent
Predominant age: Median age 30-40
Predominant sex: Male > Female (2:1)
Medical Symptoms and Signs of Disease
- Recent onset of headache becoming severe
- Nausea and vomiting
- Mental changes progressing to stupor and coma
- Afebrile or low-grade fever
- Neck stiffness
- Seizures
- Papilledema
- Focal neurological signs depending on location
What Causes Disease?
- Direct extension from otitis, mastoiditis, sinusitis or dental infection
- Cranial osteomyelitis
- Penetrating skull trauma
- Prior craniotomy
- Bacteremia from lung abscess, pneumonia
- Bacterial endocarditis
- Fungal infection of the nasopharynx
- Toxoplasma gondii (in AIDS patients)
- Cyanotic congenital heart disease
- Intravenous drug use
- No source found in 20%
- Most common infective organisms — streptococci, staphylococci, enteric gram-negative bacilli and anaerobes (usually same as source of infection), Nocardia
Risk Factors
- AIDS
- Immunocompromised
- IV drug abuse
Diagnosis of Disease
Differential Diagnosis
- Brain tumors
- Cysticercosis
- Stroke
- Resolving intracranial hemorrhage
- Subdural empyema
- Extradural abscess
- Encephalitis
Laboratory
- WBC may be normal or mildly elevated
- Culture of abscess contents, predominant organisms include Toxoplasma (AIDS), Staphylococcus (trauma), aerobic or anaerobic bacteria, fungi (rare)
- Blood studies — mild polymorphonuclear leukocytosis. elevated sedimentation rate
Drugs that may alter lab results: Prior administration of antibiotics
Disorders that may alter lab results: N/A
Pathological Findings
- Suppuration, liquefaction, encapsulation, depending on stage of evolution
- Fibrosis
Special Tests
Surgical burr hole with aspiration to make a specific bacteriologic diagnosis
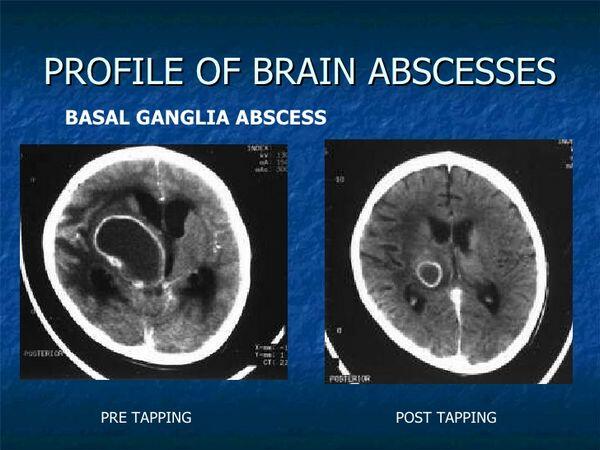
Imaging
- CT or MRI are diagnostic methods of choice — findings are dependent on stages of the abscess
- Radionuclide 117 IN-labeled leukocytes may distinguish abscess from neoplasm
Diagnostic Procedures
- History, physical exam
- Lumbar puncture often contraindicated
- Search for primary source of infection (chest x-ray, skull film for fracture, sinus films, etc.)
Treatment (Medical Therapy)
Appropriate Health Care
Inpatient for close observation, diagnostic evaluation, and specialty consultation (neurology, neurosurgery, infectious disease)
General Measures
- Palliative and supportive
- Medical therapy
- For surgical inaccessible, multiple abscesses
- For abscesses in early cerebritis stage
- Small (< 2.5 cm) abscess
- Therapy directed toward most likely organism
Surgical Measures
- Surgical therapy
- Mandatory when neurologic deficits are severe or progressive
- Used when the abscess is in the posterior fossa
- Abscess drainage — (via needle) under stereotactic CT guidance through a burr hole under local anesthesia, is most rapid and effective method. May be repeated if needed.
- Craniotomy — if abscess is large or multilocular
- Abscess resulting from trauma
Activity
Bedrest until infection controlled and abscess evacuated or resolving, then up as tolerated
Diet
IV fluids if nausea and vomiting present
Patient Education
For patient education materials favorably reviewed on this topic, contact: Brain Research Foundation, 208 S. LaSalle Street. Suite 1426, Chicago, IL 60604, (312)782-4311
Medications (Drugs, Medicines)
Drug(s) of Choice
- Antibiotics according to organism if known
- If organism unknown, begin with penicillin G and metronidazole, or chloramphenicol (Chloromycetin), if metronidazole cannot be used
- Add oxacillin or nafcillin if trauma or IV drug user (use vancomycin in penicillin-sensitive patients)
- If gram-negative organism suspected (otic, Gl, GU organ) add third-generation cephalosporin
- Abscess associated with HIV infection assumed to be due to Toxoplasma gondii — daily doses of sulfadiazine and pyrimethamine. Therapy will be life-long in AIDS patients.
- Anticonvulsants — phenytoin until abscess resolved or perhaps longer. Obtain anticonvulsant levels.
- Following surgical procedure — corticosteroids to reduce edema. Dexamethasone. Taper rapidly. Use usually limited to 1 week. Continue antibiotics for 6-8 weeks.
Contraindications: Sensitivity or allergy to any prescribed medications
Precautions:
- Sulfadiazine poorly water soluble. Patients must maintain adequate hydration or risk developing crystalluria.
- Decrease dosage of penicillins in patients with renal dysfunction
- Monitor serum levels of anticonvulsants
- Dose of pyrimethamine required for treatment of toxoplasmosis may approach toxic levels. Should observe for folic acid deficiency and treat with folinic acid (leucovorin) 5-15 mg (orally, IM, IV) if necessary
Significant possible interactions: Refer to manufacturer’s literature
Alternative Drugs
N/A
Patient Monitoring
- Postsurgical monitoring as needed
- Serial CT or MRI — to confirm progressive resolution, early detection and management of complications
Prevention / Avoidance
- Adequate treatment of otitis media, mastoiditis, dental abscess, other predisposing factors
- Prophylactic antibiotics after compound skull fracture or penetrating head wound
Possible Complications
- Permanent neurological deficits
- Surgical complications
- Recurrent abscess
- Seizures
Expected Course / Prognosis
Survival > 80% with early diagnosis and treatment
Miscellaneous
Associated Conditions
- AIDS
- Congenital heart disease
Age-Related Factors
Pediatric:
- About one third of cases in pediatric age group. Rarely found in infants under 1 year of age.
- Cyanotic congenital heart disease frequently associated
Geriatric: Age does not affect outcome as much as abscess size and state of neurological dysfunction at presentation
Pregnancy
N/A
Synonyms
Cerebral abscess
International Classification of Diseases
324.0 Intracranial abscess



