Description of Medical Condition
An intoxication producing paralytic disease caused by neurotoxins of Clostridium botulism and is the most toxic substances known to science. The toxin prevents acetylcholine release at presynaptic membranes, blocking neuromuscular transmission in cholinergic nerve fibers.
Four forms exist:
- Foodborne botulism
- Infantile botulism
- Wound botulism
- Classification undetermined
System(s) affected: Endocrine/Metabolic, Gastrointestinal, Nervous
Genetics: N/A
Incidence/Prevalence in USA:
- Rare 0.34/100,000 with 75% the infantile form
- Foodborne — 24 cases/year
- Infantile-71 cases/year
- Wound botulism — less than 100 cases in literature
- Indeterminate — very rare but incidence unknown
Predominant age:
- Foodborne — all ages
- Infantile — 2 to 4 months (rare after 6 months)
- Wound- usually younger adult
- Undetermined-older than one year
Predominant sex:
- Foodborne, infantile and undetermined — Male=Female
- Wound — Male > Female
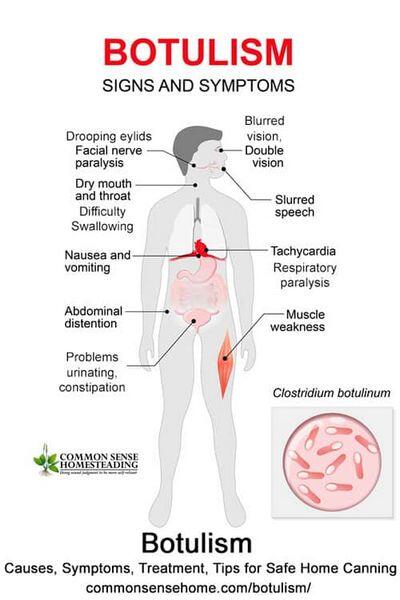
Medical Symptoms and Signs of Disease
- Foodborne
- Onset 12-48 hours after ingestion, as long as 14 days
- Nonspecific findings early (nausea, vomiting, malaise, dizziness, abdominal distension)
- Dry mouth
- Constipation, urinary retention
- Symmetric descending weakness or paralysis of motor and autonomic nerves, usually beginning with the cranial nerves
- Cranial nerve paralysis (ptosis; extraocular muscle paresis; fixed, dilated pupils; dysphagia)
- Postural hypotension
- Muscle weakness, respiratory paralysis (no sensory deficits)
- Afebrile
- Progression over several days
- Infantile
- Constipation — early sign
- Loss of head control
- Loss of suck
- Loss of facial expression and verbalization
- Symmetric descending weakness and cranial nerve paresis similar to foodborne form
- Diminished or absent deep tendon reflexes
- Autonomic dysfunction
- Afebrile
- Usual progression over 2-5 days, can be as short as few hours
- Wound
- Onset 4-14 days post injury
- Findings similar to foodborne botulism, but Gl symptoms less common
- May be febrile
- Undetermined
- Possible adult variant of infant botulism
- Findings similar to infant botulism
What Causes Disease?
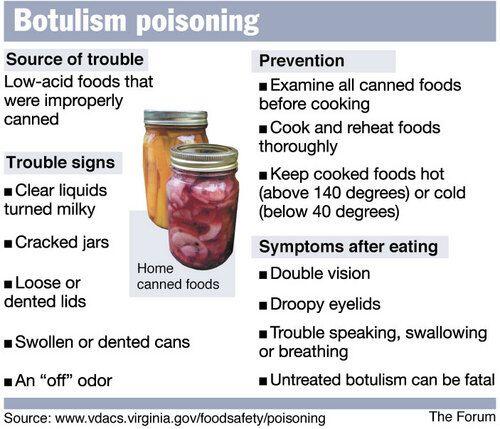
- Ingestions of C. botulinum neurotoxins (A, B, and E most common)
- Foodborne usually from home-canned vegetables, prepared foods or foods incubated in anaerobic conditions
- Infantile from ingestion of spores in environment or occasionally in honey
- Wound due to contamination with toxin-producing C. botulinum
- Undetermined — cause unknown
Risk Factors
- Foodborne — ingestion of home-canned or prepared foods
- Infantile from ingestion of honey. Breast feeding (controversial)
- Wound-IV drug use (e.g., black tar heroin) or “skin popping”
Diagnosis of Disease
Differential Diagnosis
- Guillian-Barre syndrome
- Encephalitis
- Tick paralysis
- Myasthenia gravis
- Eaton Lambert myasthenic syndrome
- Basilar artery stroke
- Congenital neuropathy or myopathy
- Sepsis
- Hypokalemic periodic paralysis
- Polio
- Other poisonings (organophosphate, shellfish, Amanita mushrooms, atropine, aminoglycoside)
Laboratory
- Routine tests — check for hypokalemia
- CSF testing — normal helps differentiate from Guillian-Barre
- Toxin detected in gastric contents, blood, feces. suspected food and containers
- Confirmation available at CDC and some state laboratories
- Pulmonary function testing
Drugs that may alter lab results: N/A
Disorders that may alter lab results: Underlying myoneural disease
Pathological Findings
- Nonspecific
Special Tests
- Stool contains organism and toxin
- Serum toxin present in foodborne form
Diagnostic Procedures
Electro my ogram (EMG) shows characteristic brief, low voltage compound motor-unit, small amplitude, overly abundant action potentials (BSAPs), incremental response to repetitive stimulation. Findings not definitive for botulism.
Treatment (Medical Therapy)
Appropriate Health Care
Inpatient, with maximal monitoring capabilities, especially for respiratory failure
General Measures
- Meticulous airway management
- Monitor pulmonary function
- Physical therapy with range of motion exercise and assisted ambulation as tolerated
- Prevention of decubiti
Surgical Measures
Wound excision debridement
Activity
Bedrest initially
Diet
- Nasogastric feedings, if needed
- Fluid restriction if inappropriate antidiuretic hormone (ADH) syndrome
Patient Education
- When preserving food at home, kill Clostridium botulism spores by pressure cooking at 250°F (120°C) for 30 minutes
- Toxin can be destroyed by boiling for 10 minutes or cooking at 175°F (80°C) for 30 minutes
- Avoid honey in first year of life
Medications (Drugs, Medicines)
Drug(s) of Choice
- Antitoxin therapy with trivalent A-B-E antitoxin (available at CDC (404) 639-3670 or 639-2888), one vial IV and one vial IM, repeat IV in 2-4 hours if symptoms persist
- Penicillin therapy of unclear value
- Infantile
- Antitoxin therapy not needed
- Penicillin therapy of unclear value
- Enemas may assist in removal of toxin
- Wound
- Antitoxin therapy with trivalent A-B-E antitoxin, one vial IV and one vial IM, repeat in 2-4 hours if persistent symptoms
- Penicillin therapy of unclear value
- Contradictions: Aminoglycosides — may potentiate paralysis
Precautions: Serum sickness or hypersensitivity reactions in 20% of antitoxin recipients. Test before treating.
Contraindications: N/A
Precautions: N/A
Significant possible interactions: N/A
Alternative Drugs
N/A
Patient Monitoring
Cardiorespiratory monitoring during illness
Prevention / Avoidance
- Avoid giving honey to infants
- Do not eat or taste food from bulging cans, or if food is off smelling
Possible Complications
- Aspiration pneumonia
- Nosocomial infection
- Hypoxic tissue damage
- Death
Expected Course / Prognosis
- Foodborne and wound
- Mortality 25% (<10% under 20 years of age), usually due to delayed diagnosis and respiratory failure
- Full recovery may require months
- Sequelae due to hypoxic insults
- Infantile
- Mortality < 10%
- Extended recovery period and sequelae as above
Miscellaneous
Associated Conditions
N/A
Age-Related Factors
Pediatric: Avoid honey first year
Geriatric: N/A
Pregnancy
N/A
Synonyms
• Sausage poisoning
• Kerner’s disease
International Classification of Diseases
005.1 Botulism
See Also
Food poisoning, bacterial Tick paralysis
Other Notes
Organism present in stools of 1 -2% of healthy individuals. Release of toxins in the gut may worsen symptoms of infantile botulism by bacterial lysis.


 (1 votes, average: 4.00 out of 5)
(1 votes, average: 4.00 out of 5)
