Histoplasmosis
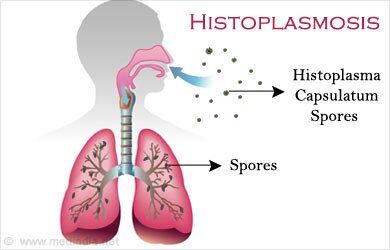
- Histoplasmosis is caused by inhalation of dust-borne microconidia of the dimorphic fungus Histoplasma capsulatum.
- In the United States, most disease is localized along the Ohio and Mississippi river valleys.
Clinical Presentation
- In the vast majority of patients, low-inoculum exposure to H. capsulatum results in mild or asymptomatic pulmonary histoplasmosis. The course of disease is generally benign, and symptoms usually abate within a few weeks of onset. Patients exposed to a higher inoculum during a primary infection or reinfection may experience an acute, self-limited illness with flulike pulmonary symptoms, including fever, chills, headache, myalgia, and nonproductive cough.
- Chronic pulmonary histoplasmosis generally presents as an opportunistic infection imposed on a preexisting structural abnormality such as lesions resulting from emphysema. Patients demonstrate chronic pulmonary symptoms and apical lung lesions that progress with inflammation, calcified granulomas, and fibrosis. Progression of disease over a period of years, seen in 25% to 30% of patients, is associated with cavitation, bronchopleural fistulas, extension to the other lung, pulmonary insufficiency, and often death.
- In patients exposed to a large inoculum and in immunocompromised hosts, progressive illness, disseminated histoplasmosis, occurs. The clinical severity of the diverse forms of disseminated histoplasmosis (Table Clinical Manifestations and Therapy of Histoplasmosis) generally parallels the degree of macrophage parasitization observed.
- Acute (infantile) disseminated histoplasmosis is seen in infants and young children and (rarely) in adults with Hodgkin’s disease or other lymphoproliferative disorders. It is characterized by unrelenting fever; anemia; leukopenia or thrombocytopenia; enlargement of the liver, spleen, and visceral lymph nodes; and gastrointestinal symptoms, particularly nausea, vomiting, and diarrhea. Untreated disease is uniformly fatal in 1 to 2 months.
- Most adults with disseminated histoplasmosis demonstrate a mild, chronic form of the disease. Untreated patients are often ill for 10 to 20 years, with long asymptomatic periods interrupted by relapses.
- Adult patients with AIDS demonstrate an acute form of disseminated disease that resembles the syndrome seen in infants and children.
| TABLE. Clinical Manifestations and Therapy of Histoplasmosis | |||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
Diagnosis
- Identification of mycelial isolates from clinical cultures can be made by conversion of the mycelium to the yeast form (requires 3 to 6 weeks) or by the more rapid (2-hour) and 100% sensitive DNA probe that recognizes ribosomal DNA.
- In most patients, serologic evidence remains the primary method in the diagnosis of histoplasmosis. Results obtained from complement fixation, immunodiffusion, and latex antigen agglutination antibody tests are used alone or in combination.
- In the AIDS patient with progressive disseminated histoplasmosis, the diagnosis is best established by bone marrow biopsy and culture, which yield positive cultures in 90% of patients.
Treatment
- Recommended therapy for the treatment of histoplasmosis is summarized in Table Clinical Manifestations and Therapy of Histoplasmosis.
- Asymptomatic or mildly ill patients and patients with sarcoid-like disease generally do not benefit from antifungal therapy. Therapy may be helpful in symptomatic patients whose conditions have not improved during the first month of infection.
- Patients with mild, self-limited disease, chronic disseminated disease, or chronic pulmonary histoplasmosis who have no underlying immunosuppression can usually be treated with either oral ketoconazole or intravenous amphotericin B.
- In AIDS patients, intensive 12-week primary (induction and consolidation therapy) antifungal therapy is followed by lifelong suppressive (maintenance) therapy with itraconazole.
- In AIDS patients, amphotericin B should be administered in patients who require hospitalization. Itraconazole 200 mg twice daily may be used to complete a 12-week course.
- Response to therapy should be measured by resolution of radiologic, serologic, and microbiologic parameters and improvement in signs and symptoms of infection.
- Once the initial course of therapy for histoplasmosis is completed, lifelong suppressive therapy with oral azoles or amphotericin B (1 to 1.5 mg/kg weekly or biweekly) is recommended, because of the frequent recurrence of infection.
- Relapse rates in AIDS patients not receiving preventive maintenance are 50% to 90%.
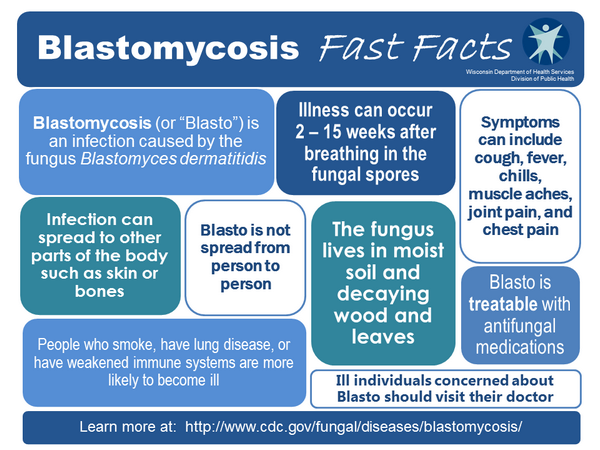
Blastomycosis
- North American blastomycosis is a systemic fungal infection caused by Blastomyces dermatitidis.
- Pulmonary disease probably occurs by inhalation conidia, which convert to the yeast forms in the lungs. It may be acute or chronic and can mimic infection with tuberculosis, pyogenic bacteria, other fungi, or malignancy.
- Blastomycosis can disseminate to virtually every other body organ including skin, bones and joints, or the genitourinary tract without any evidence of pulmonary disease.
Clinical Presentation
- Acute pulmonary blastomycosis is generally an asymptomatic or self-limited disease characterized by fever, shaking chills, and a productive, purulent cough.
- Pulmonary blastomycosis may present as a more chronic or subacute disease, with low-grade fever, night sweats, weight loss, and a productive cough resembling that of tuberculosis rather than bacterial pneumonia.
- Chronic pulmonary blastomycosis is characterized by fever, malaise, weight loss, night sweats, and cough.
Diagnosis
- The simplest and most successful method of diagnosing blastomycosis is by direct microscopic visualization of the large, multinucleated yeast with single, broad-based buds in sputum or other respiratory specimens, following digestion of cells and debris with 10% potassium hydroxide.
- Histopathologic examination of tissue biopsies and culture of secretions should be used to identify B. dermatitidis.
Treatment
- In patients with mild pulmonary blastomycosis, the clinical presentation of the patient, the immune competence of the patient, and the toxicity of the antifungal agents are the main determinants of whether or not to administer antifungal therapy. All immunocompromised patients and patients with progressive disease or with extrapulmonary disease should be treated (Table Therapy of Blastomycosis).
- Some authors recommend ketoconazole therapy for the treatment of self-limited pulmonary disease, with the hope of preventing late extrapulmonary disease.
- Itraconazole, 200 to 400 mg/day, is an effective as a first-line agent in the treatment of non-life-threatening non-central nervous system blastomycosis.
- All patients with disseminated blastomycosis and those with extrapulmonary disease require therapy (ketoconazole, 400 mg/day orally for 6 months). Central nervous system disease should be treated with amphotericin B for a total cumulative dose greater than 1 g.
- Patients who fail or are unable to tolerate itraconazole therapy, or who develop central nervous system disease, should be treated with amphotericin B for a total cumulative dose of 1.5 to 2.5 g.
- HIV-infected patients should receive induction therapy with amphotericin B and chronic suppressive therapy with an oral azole antifungal. Itraconazole is the drug of choice for non-life-threatening histoplasmosis.
Coccidioidomycosis
Coccidioidomycosis is caused by infection with Coccidioides immitis. The endemic regions encompass the semi-arid regions of the southwestern United States from California to Texas, known as the Lower Sonoran Zone.
Clinical Presentation
- Most of those infected are asymptomatic or have nonspecific symptoms that are often indistinguishable from those of ordinary upper respiratory infections, including fever, cough, headache, sore throat, myalgias, and fatigue. A fine, diffuse rash may be appear during the first few days of illness.
- «Valley fever» is a syndrome characterized by erythema nodosum and erythema multiforme of the upper trunk and extremities in association with diffuse joint aches or fever. Valley fever occurs in approximately 25% of infected persons, although, more commonly, a diffuse mild erythroderma or maculopapular rash is observed.
- Pulmonary coccidioidomycosis can also present as acute pneumonia or develop into a chronic, persistent pneumonia complicated by hemoptysis, pulmonary scarring, and the formation of cavities of bronchopleural fistulas.
| TABLE. Therapy of Blastomycosis | |||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||
- Disseminated infection occurs in less than 1% of infected patients. Dissemination may occur to the skin, lymph nodes, bone, meninges, spleen, liver, kidney, and adrenal gland.
Diagnosis
- Most patients develop a positive skin test within 3 weeks of the onset of symptoms.
- Infection is characterized by the development of IgM to C. immitis, which peaks within 2 to 3 weeks of infection and then declines rapidly, and immunoglobulin G, which peaks in 4 to 12 weeks and declines over months to years.
- Recovery of C. immitis from infected tissues or secretions for direct examination and culture provides an accurate and rapid method of diagnosis.
Treatment
- Only 5% of infected persons require therapy. Candidates for therapy include those with severe primary pulmonary infection or concurrent risk factors (e.g., HIV infection, organ transplant, or high doses of glucocorticoids), particularly patients with high complement fixation antibody titers in whom dissemination is likely.
- Specific antifungals (and their usual dosages) for the treatment of coccidioidomycosis include amphotericin B intravenous (0.5 to 0.7 mg/kg/day), ketoconazole (400 mg orally daily), intravenous or oral fluconazole (usually 400 to 800 mg daily, although dosages as high as 1200 mg/day have been utilized without complications), and itraconazole (200 to 300 mg orally twice daily as either capsules or solution). If itraconazole is used, measurement of serum concentrations may be helpful to ascertain whether oral bioavailability is adequate. Amphotericin B is generally preferred as initial therapy in patients with rapidly progressive disease, whereas azoles are generally preferred in patients with subacute or chronic presentations. Treatments for primary respiratory disease (mainly symptomatic patients) are 3- to 6-month courses of therapy.
Cryptococcosis
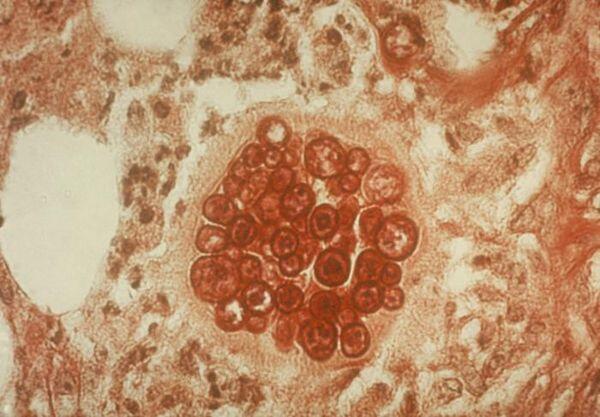
Cryptococcosis is a noncontagious, systemic mycotic infection caused by the ubiquitous encapsulated soil yeast Cryptococcus neoformans.

Clinical Presentation
- Primary cryptococcosis in humans almost always occurs in the lungs. Symptomatic infections are usually manifested by cough, rales, and shortness of breath that generally resolve spontaneously.
- Disease may remain localized in the lungs or disseminate to other tissues, particularly the central nervous system, although the skin can also be affected.
- In the non-AIDS patient, the symptoms of cryptococcal meningitis are nonspecific. Headache, fever, nausea, vomiting, mental status changes, and neck stiffness are generally observed.
- In AIDS patients, fever and headache are common, but meningismus and photophobia are much less common than in non-AIDS patients.
Diagnosis
- Examination of cerebrospinal fluid in patients with cryptococcal meningitis generally reveals an elevated opening pressure, cerebrospinal fluid pleocytosis (usually lymphocytes), leukocytosis, a decreased cerebrospinal fluid glucose, an elevated cerebrospinal fluid protein, and a positive cryptococcal antigen.
- Antigens to C. neoformans can be detected by latex agglutination.
- C. neoformans can be detected in approximately 60% of patients by India ink smear of cerebrospinal fluid and cultured in more than 96% of patients.
Treatment
- Treatment of cryptococcosis is detailed in Table Therapy of Cryptococcocosis.
- For asymptomatic, immunocompetent persons with isolated pulmonary disease and no evidence of central nervous system disease, careful observation may be warranted. With symptomatic infection, fluconazole or amphotericin B is warranted.
| TABLE. Therapy of Cryptococcocosisa,b | ||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
- The combination of amphotericin B with flucytosine for 6 weeks is often used for treatment of cryptococcal meningitis. An alternative is amphotericin B for 2 weeks followed by fluconazole for an additional 8 to 10 weeks.
- The use of intrathecal amphotericin B is not recommended for the treatment of cryptococcal meningitis except in very ill patients or in those with recurrent or progressive disease despite aggressive intravenous amphotericin B therapy. The dosage of amphotericin B employed is usually 0.5 mg administered via the lumbar, cisternal, or intraventricular (via an Ommaya reservoir) route 2 or 3 times weekly.
- Amphotericin B with flucytosine is the initial treatment of choice for acute therapy of cryptococcal meningitis in AIDS patients. Many clinicians will initiate therapy with amphotericin B, 0.7 mg/kg/ day intravenous (with flucytosine, 100 mg/kg/day). After 2 weeks, consolidation therapy with either itraconazole 400 mg/day orally or fluconazole 400 mg/day orally can be administered for 8 weeks or until cerebrospinal fluid cultures are negative. Lifelong therapy with fluconazole is then recommended.
Relapse of C. neoformans meningitis occurs in approximately 50% of AIDS patients after completion of primary therapy. Fluconazole (200 mg daily) is currently recommended for chronic suppressive therapy of cryptococcal meningitis in AIDS patients.


