Essentials of Diagnosis
- Patients are usually immunocompetent.
- Found worldwide but usually in tropical or subtropical areas.
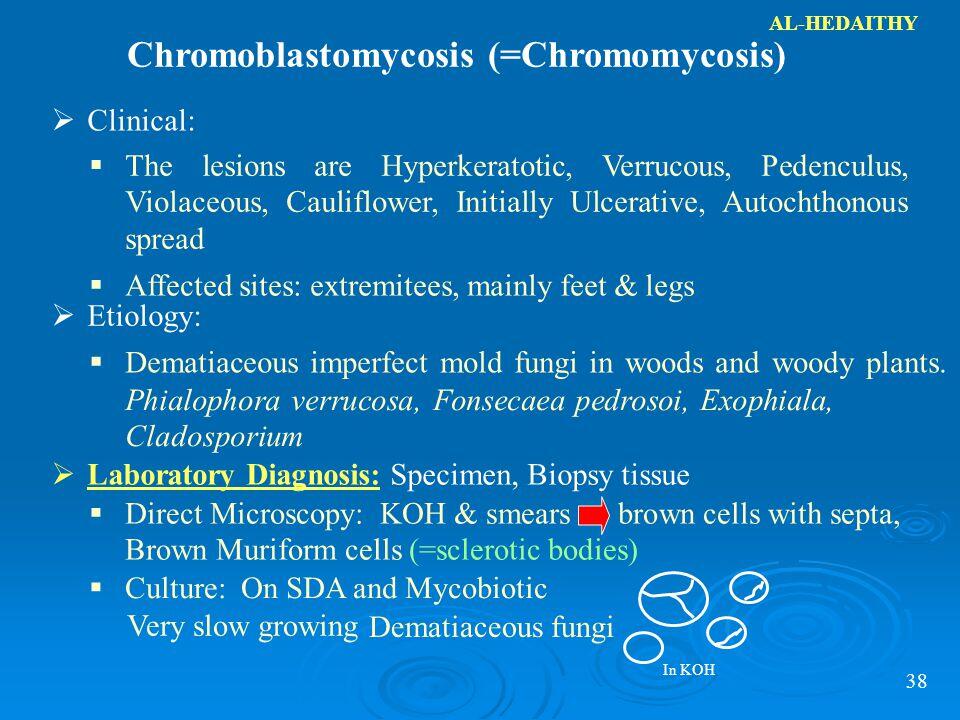
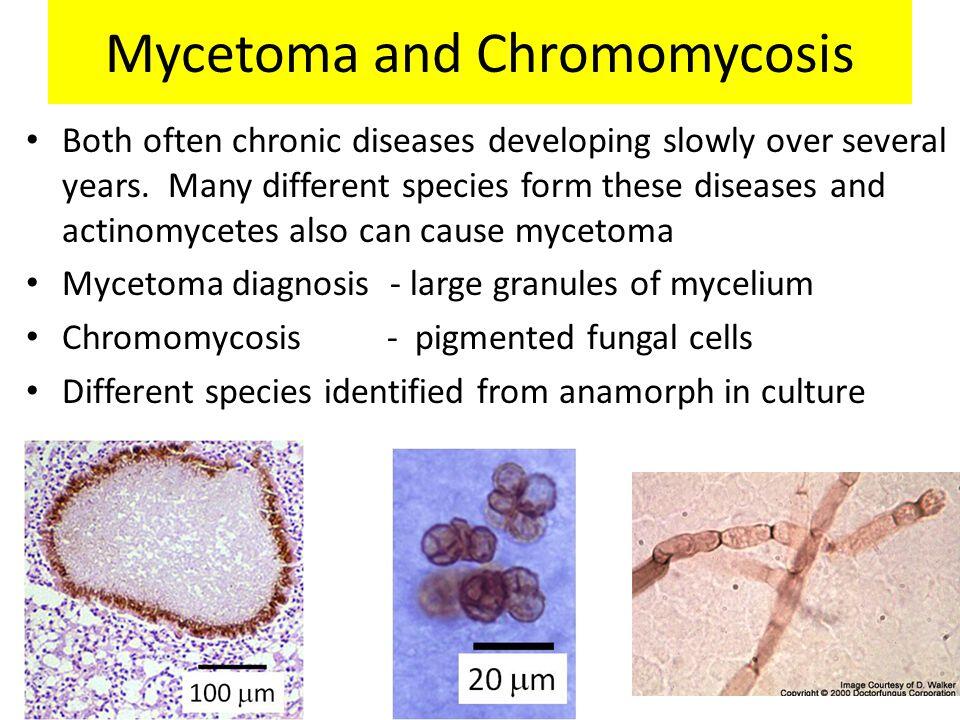
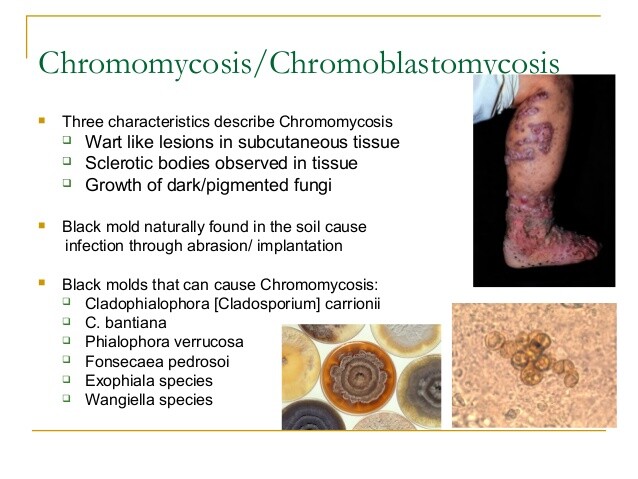
- Mold in culture; forms sclerotic body or muriform cell in tissue.
- Infection results from direct inoculation from contaminated soil or vegetative substances.
- Chronic indolent cutaneous verrucous lesions, most often on the feet.
General Considerations
Chromomycosis, also known as chromoblastomycosis, is a chronic subcutaneous infection caused by several different fungi. Although rarely seen in the United States, it is common worldwide.
Epidemiology
Chromomycosis occurs worldwide but is most frequently encountered in tropical and subtropical regions. The most common occurrence is in barefoot individuals, particularly among agricultural workers. The organisms causing chromomycosis are found commonly in soil, rotting wood, and decaying vegetation. Infection follows only after traumatic exposure to soil or other material, and person-to-person transmission does not occur.
Microbiology
A variety of different agents is capable of producing the clinical syndrome chromomycosis. The most common is Fonsecaea pedrosoi. Others that may be encountered include Fonsecaea compactum, Cladosporium carrionii, Phialophora verrucosa, Botryomyces caespitosus, Rhinocladiella aquaspersa, Exophiala spinifera, and E jeanselmei. These fungi share a number of characteristics. Most are exceedingly slow growing and require 4-6 weeks in the mycology laboratory before growth may be encountered on culture plates. The colonies tend to be dark green to brown or black in color, and the hyphae are septate. Speciation can be difficult and requires an experienced mycologist.
Pathogenesis
After an incubation period of several weeks following traumatic subcutaneous inoculation, clinical infection begins. Histologically, there is a pyogranulomatous reaction and significant pseudoepithelial hyperplasia yielding the characteristic verrucoid appearance. Sclerotic bodies, also known as muriform cells, are the characteristic histologic finding. These are actually brown, round, fungal elements that are thick-walled and septated. Their presence on histologic examination is pathonomonic. Occasionally, there may be associated branched septated hyphae adjacent to the muriform cells.
Clinical Findings
Signs and Symptoms
Chromomycosis is a chronic skin and soft tissue infection that may develop over months, years, or decades (Box 9). Frequently, patients seek medical attention for cosmetic reasons after years of infection. The feet are the most common location after inoculation from being barefoot. The hands, arms, and legs may also be involved. Typically, a lesion will start as a papule and slowly enlarge to develop into a nodule or plaque.
Different morphologic forms of infection have been described. The verrucous form has a bulky, wartlike appearance and can be very disfiguring. It is often described as cauliflowerlike in appearance. Ulceration, crusting, and bacterial superinfection are common. The annular form tends to be more flattened with a slowly advancing edge of infection with central healing and scarring. This form is more likely to lead to lymphedema, which in its extreme manifestation may resemble elephantiasis. Infection remains localized with satellite lesions and only rarely disseminates.
Laboratory Findings
Blood chemistries and cell counts are usually normal in patients with chromomycosis.
Imaging
Plain film roentgenograms of affected sites will show only soft tissue changes. Bony involvement is rarely seen.
Differential Diagnosis
A wide variety of infections can cause a syndrome similar to that of chromomycosis. Blastomycosis, sporotrichosis, and mycetoma are other fungal infections that may present as chronic skin and subcutaneous infection. Yaws, tertiary syphilis, leishmaniasis, tuberculosis, and infection with atypical mycobacterium are other possibilities. Carcinoma, on rare occasion, may resemble chromomycosis.
Diagnosis
The diagnosis of chromomycosis requires scraping or biopsy. The presence of the characteristic sclerotic body is diagnostic. These are easily seen with a KOH stain, particularly when collected from verrucous form of infection. Annular infections tend to have a lower number of organisms and may require biopsy. Scrapings and biopsy specimens submitted to culture should be held in the mycology laboratory for = 4-6 weeks to allow sufficient time for growth to occur. There are no serological tests to assist in the diagnosis of mucormycosis.
Treatment
Treatment of chromomycosis is difficult, and failure to achieve a cure is common (Box 10). Early, localized infection can be treated with wide surgical excision. Cryotherapy with liquid nitrogen has also been successful in eradicating early infection.
More established infection will require antifungal therapy; 5-flucytosine has been extensively used. Many cases will have partial response, but relapse is common, and resistance develops frequently. Retreatment with 5-flucytosine is usually unsuccessful because resistance develops. The role of the azoles in the treatment of chromomycosis continues to evolve. Ketoconazole is ineffective. Both itraconazole and fluconazole have been used with some success. The optimal duration of therapy has not been established, and failures and relapses are common. Amphotericin B has been tried in resistant cases but is generally not recommended. Terbinafine has been used in a very small number of patients with promising results. More experience with this agent is needed before it can be recommended. The optimal therapeutic approach to chromomycosis remains to be determined.
Prognosis
Untreated chromomycosis leads to a disfiguring, slowly enlarging lesion. Elephantiasis can develop as a result of the disruption and obstruction of lymphatics.
Prevention & Control
Chromomycosis of the feet can be prevented by wearing shoes (Box 11). Agricultural workers and other at-risk individuals should attempt to limit trauma to their hands and extremities. Because the organisms causing this infection are ubiquitous in soil and vegetative material, control efforts directed at reducing or eradicating the organisms are impractical.
Useful Links
https://en.wikipedia.org/wiki/Chromoblastomycosis
https://www.ncbi.nlm.nih.gov/pubmed/701532
http://jamanetwork.com/journals/jama/article-abstract/263447