Essentials of Diagnosis
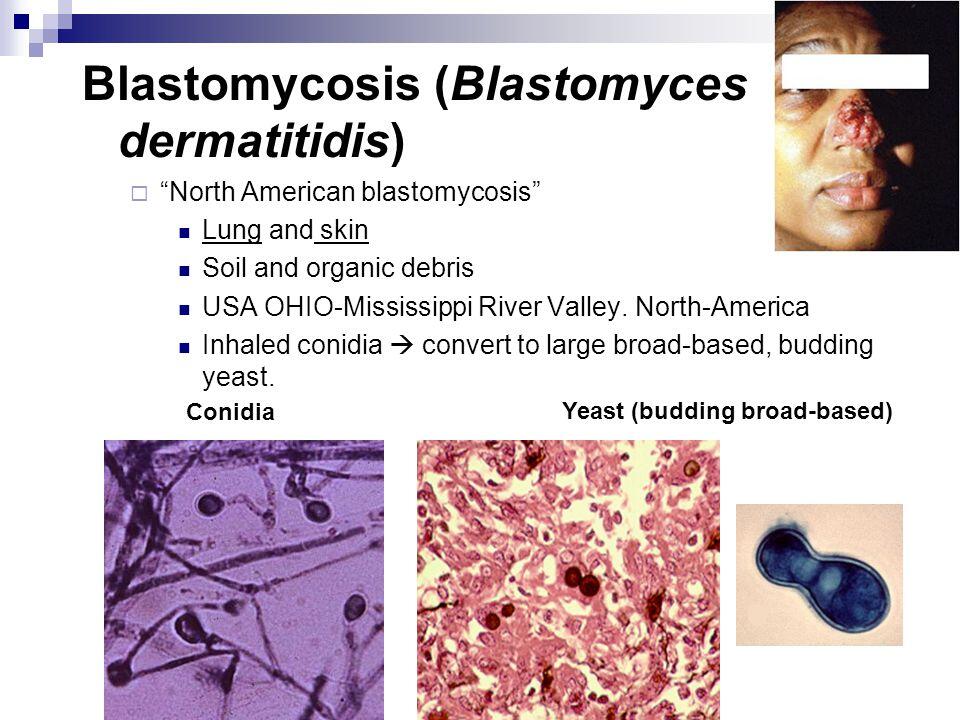
- Round thick-walled yeast with broad-based budding.
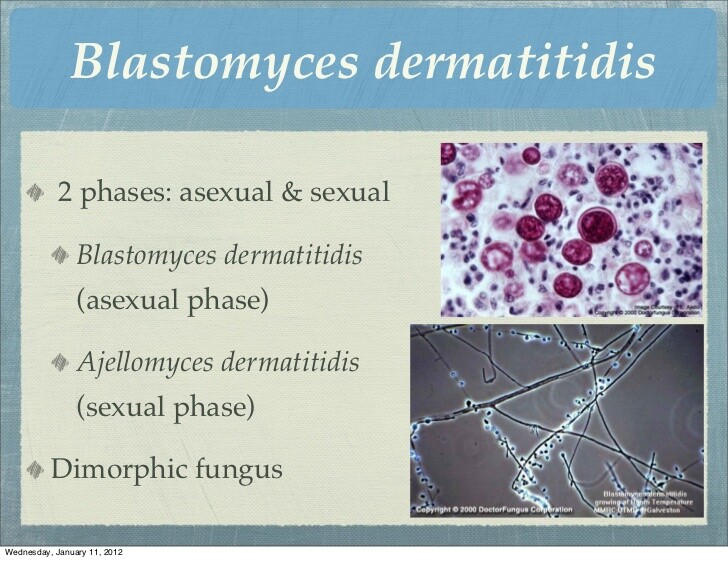
- Dimorphic: mycelial in nature, yeast in tissue.
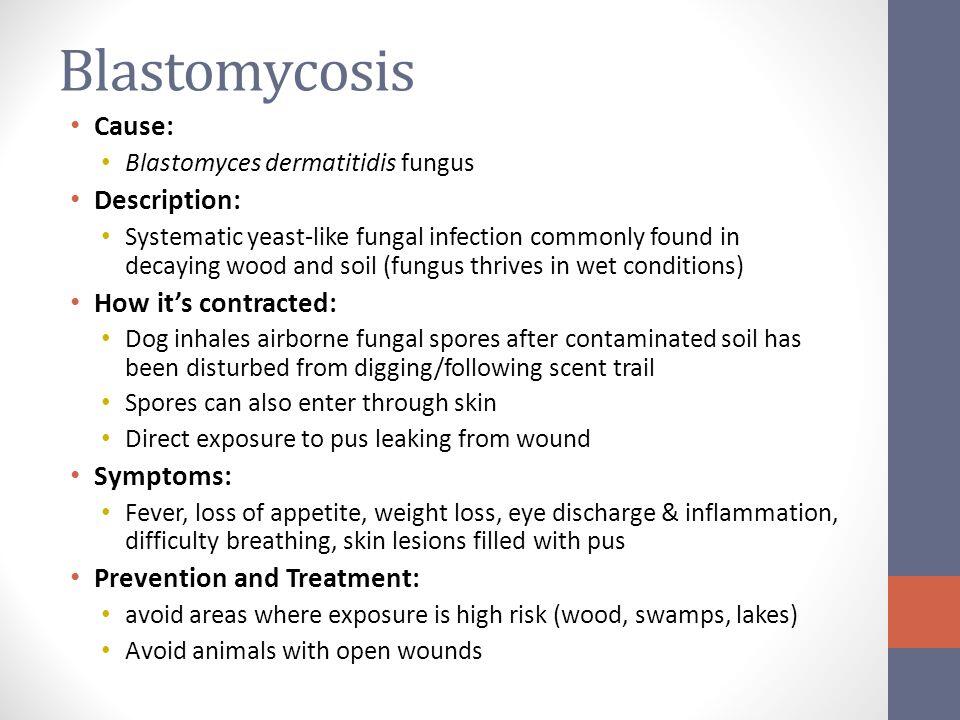
- Associated with activities in proximity to waterways.
- Associated with exposure to dust, eg excavation.
- Endemic in states surrounding the Mississippi and Ohio Rivers.
- Pyogranulomas on histopathological examination.
- Acute or chronic infection of lung, skin, bone, or genitourinary tract.
- Recovery of microorganism from culture of tissue.
General Considerations
Epidemiology
Blastomyces dermatitidis is an endemic fungus that causes acute and chronic infections in humans and other animals. It is found primarily in the south central, southeastern, and midwestern United States, especially in the states surrounding the Mississippi and Ohio Rivers. Outside the United States, cases have been reported from Canadian provinces bordering the Great Lakes, Africa, India, the Middle East, and Central and South America.
Both clusters and sporadic cases of blastomycosis have been reported. Outdoor activities in proximity to waterways as well as exposure to dust from construction and excavation have been noted as possible risk factors for acquiring infection.
Microbiology
B dermatitidis is a dimorphic fungus, which means that it occurs as a mold in nature and in a yeast form in tissue (and at a temperature of 37 °C). The yeast cells are round and thick walled with daughter cells forming from a broad-based bud.
Pathogenesis
The lungs are the initial portal of entry for blastomycosis in humans, although primary cutaneous blastomycosis as a result of accidental skin inoculation in the laboratory or after dog bites has been reported.
Infection begins with inhalation of conidia of the mycelial phase of the organism. In the lungs, the fungus converts to its yeast phase. Inflammatory response occurs in the form of polymorphonuclear leukocyte infiltration followed by macrophage infiltration and granuloma formation. The infection can spread via the bloodstream and lymphatic system to distant sites. Cellular immunity is the major protecting factor in preventing progression of disease in blastomycosis.
CLINICAL SYNDROMES
B dermatitidis may cause disease in virtually every organ of the body. The most common clinical syndromes associated with blastomycosis are described in the following sections (Box 1).
PULMONARY INFECTION
Pulmonary blastomycosis characteristically presents as an acute or chronic pneumonitis.
ACUTE PULMONARY INFECTION
Clinical Findings
Signs and Symptoms
After exposure to B dermatitidis, a significant proportion of individuals have asymptomatic disease. The true frequency of asymptomatic or subclinical disease is unknown. In one large outbreak, 46% of infected individuals were asymptomatic.
Symptomatic acute pulmonary infection presents similarly to an acute bacterial pneumonia with fever, chills, and productive cough, with or without hemoptysis or pleuritic chest pain.
Imaging
The appearance of the chest radiograph is variable and nonspecific. The most common radiological appearance of pulmonary blastomycosis is airspace consolidation. Other radiographic features include nodular masses, interstitial disease, and cavitation. Pleural effusions are occasionally noted, but they are usually small. Hilar and mediastinal adenopathy or calcification of parenchymal lesions is uncommon.
Differential Diagnosis
Differential diagnosis of pulmonary blastomycosis includes other types of pneumonia (eg, bacterial and fungal) and tuberculosis, as well as lymphoma and malignant neoplasms.
Complications
The course of pulmonary infection is variable. The disease may clear with or without treatment or progress to chronic pulmonary disease. Occasionally, overwhelming pulmonary infection with B dermatitidis results in the adult respiratory distress syndrome (ARDS) and respiratory failure, indistinguishable from ARDS caused by bacterial sepsis and characterized by severe impairment of gas exchange and hemodynamic instability.
This syndrome is also associated with significant mortality. In one report, only 13 of 29 patients survived. Although also seen in immunocompetent individuals, it is much more often encountered in immunocompromised individuals, including those with AIDS. Large amounts of B dermatitidis are easily recovered from respiratory cultures, and examination of lung tissue will show histopathological changes characteristic of ARDS, as well as the presence of a large number of the causative organisms. Aggressive therapy with large doses of amphotericin B (0.7-1.0 mg/kg) should be initiated promptly, and many patients require mechanical ventilatory assistance. Survivors may regain good pulmonary function.
CHRONIC PULMONARY INFECTION
Clinical Findings
Signs and Symptoms
The symptoms usually noted in chronic pneumonia caused by blastomycosis include weight loss, fever, night sweats, productive cough, and pleuritic chest pain. These symptoms are usually present for 2-6 months before diagnosis. Chronic pulmonary blastomycosis may be accompanied by extrapulmonary disease.
B. Imaging. The radiological presentation of chronic disease is variable and nonspecific and includes alveolar infiltrates, masses, nodules, and cavities. There is no specific pattern or distribution that corresponds with disease stage.
Differential Diagnosis
Same as for acute pulmonary infection.
Complications
Complications of chronic pulmonary blastomycosis include acute deterioration and respiratory failure, as well as hematogenous dissemination to extrapulmonary sites.
EXTRAPULMONARY INFECTION
Extrapulmonary disease is usually seen in conjunction with pulmonary infection and is the result of hematogenous dissemination of B dermatitidis. The exception is primary cutaneous blastomycosis, which occurs as a result of accidental inoculation in the laboratory, during autopsy, or after dog bites.
CUTANEOUS BLASTOMYCOSIS
Cutaneous blastomycosis is the most commo manifestation of extrapulmonary blastomycosis (40%- 80% of reported cases). Areas of the body not covered by clothing are sites of predilection, but lesions can occasionally be found on mucocutaneous surfaces. The skin lesions start as papules or pustules but later advance to form either verrucous (ie, fungating, heaped up) or ulcerative lesions. The verrucous lesions, both by their gross and microscopic (hyperplasia, acanthosis) appearance, may be mistaken for cancer. Other differential diagnosis includes skin lesions caused by other fungi (eg, Histoplasma capsulatum, Coccidioides immitis, and Sporothrix schenckii), as well as lesions caused by nocardiosis and atypical mycobacteria (eg, Mycobacterium marinum). Both types of skin lesions may be present in the same patient.
SKELETAL BLASTOMYCOSIS
Bone involvement represents the second most frequent manifestation of extrapulmonary disease, having been reported in = 25% of extrapulmonary cases. The most commonly affected bones are the vertebrae, pelvis, sacrum, ribs, and long bones, but any bone can be involved. The usual presenting symptoms consist of soft tissue abscesses or chronic draining sinuses adjacent to areas of osteomyelitis. Vertebral disease, with involvement of the vertebral body and development of large paraspinal abscesses, may be indistinguishable from tuberculosis. The typical radiographic appearance is a well-circumscribed osteo- lytic lesion.
Vertebral disease may be indistinguishable from tuberculosis. In addition, differential diagnosis includes bacterial osteomyelitis, osteomyelitis caused by other fungi, and a Brodie abscess.
GENITOURINARY BLASTOMYCOSIS
Blastomycosis of the genitourinary tract follows skin and bone infection in the frequency of its extrapulmonary involvement. Men are more prone to be infected than women. Prostatic involvement is the most common presentation, followed by epidydimoorchitis. Symptoms include urinary obstruction with an enlarged and tender prostate and pyuria.
Yield of cultures may be improved by collection of urine after prostatic massage. In women, both endometrial infection as a result of sexual contact with a man with blastomycosis on the penis and tuboovarian abscess after hematogenous dissemination have been reported.
BLASTOMYCOSIS OF THE CENTRAL NERVOUS SYSTEM
Central nervous system blastomycosis is an uncommon complication of disseminated disease. It presents either as an abscess or meningitis. Abscesses present as mass lesions, either intracranially or in an epidural location. Meningitis is difficult to diagnose. Cerebrospinal fluid evaluation is usually not diagnostic. Culture of ventricular fluid may on occasion yield the organism. Cultures of large volumes of spinal fluid increase the likelihood of a positive culture.
BLASTOMYCOSIS & AIDS
Blastomycosis is an uncommon infection among patients with AIDS and is not recognized as an AIDS-defining opportunistic infection according to present Centers for Disease Control guidelines. When it occurs, it is a late manifestation of HIV infection, usually affecting individuals with prior diagnosis of an AIDS-defining illness and CD4 lymphocyte counts of < 200 cells/mm3. It can present either with disease limited to the lungs and pleura or with disseminated infection involving multiple visceral organs. There is also more frequent involvement of the central nervous system. Cutaneous lesions appear to be less common.
A higher frequency of diffuse interstitial or miliary pattern is noted on chest radiograms. Relapse is common, necessitating chronic maintenance treatment to prevent recurrent disease.
BLASTOMYCOSIS IN OTHER IMMUNOCOMPROMISED HOSTS
Blastomycosis has been reported to cause infection in other immunocompromised patients including patients on long-term glucocorticoid treatment, solid-organ transplant recipients, patients with hematological malignancies, patients with disorders of neutropenia, patients demonstrating humoral immune dysfunction, and patients with combined immunologic dysfunction. Infection in these individuals differs from that of normal hosts in several ways. The pulmonary involvement is more extensive; a greater frequency of progression to respiratory failure and ARDS is observed.
Diffuse interstitial alveolar changes and pleural effusions are much more common than in normal hosts. Multiple visceral organ disease, with or without central nervous system involvement, is also more common.
Diagnosis
Blastomycosis is diagnosed by identification and isolation of the organism in tissue, exudate, or histopathologic sections.
Direct Examination
Sputum, pus, and body fluids such as urine, pleural fluid, or cerebrospinal fluid can be evaluated by direct microscopic examination. Wet preparation, potassium hydroxide preparation, or calcofluor white stain can be used for this purpose. B dermatitidis is recognized and identified on the basis of its size and characteristic morphologic features (broad-based buds, refractile cell wall).
Histopathologic Examination
Histopathologic sections should be screened for presence of the fungus by using the Gomori methenamine silver stain or the periodic acid-Schiff stain. Fluorescent stains may be helpful when the fungal elements are sparse. Pyogranulomas, if noted, suggest the possibility of blastomycosis.
Culture
B dermatitidis usually requires 5 days to 4 weeks for growth to be detected but may be detected in as little as 2-3 days. Conversion of the mycelial form to the yeast form is required for confirmation of the diagnosis. B dermatitidis may also be identified by nucleic acid probe testing or by the presence of a specific A band in the exoantigen test.
Serology
Several serologic methods, including serum complement fixation tests, immunodiffusion tests, radio immunoassays, and enzyme-linked immunosorbent assays, have been developed. None has been useful because of low sensitivity and specificity rates.
Treatment
Acute pulmonary infection caused by B dermatitidis sometimes resolves spontaneously without specific therapy. However, it is not possible to determine which patients will progress to serious infection or develop extrapulmonary disease. For this reason, many authorities recommend treating all cases of active blastomycosis. If withholding treatment is considered, extrapulmonary disease should be excluded. If treatment is withheld, patients must be carefully monitored for a prolonged period for evidence of relapse, progression, or extrapulmonary infection.
Amphotericin B is the drug of choice for immunocompromised patients, including those with AIDS, patients with life-threatening infections, and patients with central nervous system disease (Box 2). Because relapse of blastomycosis after amphotericin therapy is dose related and rarely occurs in patients who had received > 1.5 g of the drug, a total cumulative dose of amphotericin between 1.5 and 2.5 g is recommended.
Itraconazole, a triazole antifungal agent, is the drug of choice for those patients who do not require amphotericin B (see above). It should be used at a dose of 200 mg/d orally. The dose can be increased to 400 mg/d for persistent or progressive disease. A minimum of 6 months of therapy is recommended by most authorities.
Ketoconazole, another oral antifungal agent with a similar mechanism of action to itraconazole, may be used at a dose of 400 mg/d by mouth. Doses of = 800 mg/d may be required for persistent and unresponsive disease. Treatment should be continued for = 6 months.
Both itraconazole and ketoconazole require gastric acid for absorption. There are significant drug-drug interactions with drugs such as terfenadine, rifampin, phenytoin, and carbamazepine. In addition, neither itraconazole nor ketoconazole is excreted in the urine as an active drug. Therefore treatment of genitourinary blastomycosis with these agents may be inadequate.
Fluconazole, another triazole antifungal agent, has been shown to be moderately effective in the treatment of non-life-threatening blastomycosis at a dose of 200-400 mg/d.
Patients with AIDS and immunocompromised patients with ongoing immunosuppression require chronic oral maintenance treatment (eg, itraconazole, 200 mg/d) to prevent recurrence.
Surgery may be indicated for evacuation of large abscesses, diagnostic biopsy, or removal of central nervous system mass lesions, or debridement of devitalized and necrotic bone in patients with osteomyelitis refractory to pharmacotherapy.
Prognosis
The mortality rate for blastomycosis in HIV-infected patients is much higher than the mortality rate from blastomycosis in the general population. In one report, of 24 patients with HIV and blastomycosis, 15 (63%) had disseminated disease, and 13 (54%) died as a result of their infection. Previous reports have suggested a mortality rate of ~ 10% in those with disseminated blastomycosis but without concomitant HIV infection.
Prevention & Control
Individuals residing in endemic areas who are at increased risk (eg, immunocompromised or HIV-infected individuals) should avoid activities associated with acquiring infection, such as exposure to dust, construction, or excavation. AIDS patients with blastomycosis who have completed initial therapy should receive lifelong suppressive treatment with itraconazole (Box 3).
BOX 1. Clinical Syndromes in Blastomycosis in Adults and Children
More Common
- Pulmonary
Less Common
- Cutaneous
- Skeletal
- Genitourinary
Uncommon
- Central nervous system
- Disseminated
BOX 2. Treatment of Blastomycosis in Adults and Children
Life-Threatening Infection, Central Nervous System Infection, AIDS1
All others
First Choice
- Amphotericin B; daily dose: 0.3-0.6 mg/kg (total dose: 1.5-2.5 mg/kg)
- Itraconazole, 200-400 mg PO daily for a minimum of 6 mo
Second Choice
- Itraconazole, 200-400 mg PO daily for a minimum of 6 mo2
- Ketoconazole, 400-800 mg daily for a minimum of 6 mo
- Fluconazole, 200-400 mg daily for a minimum of 6 mo3
- Amphotericin; daily dose: 0.3-0.6 mg/kg (total dose: 1.5-2.5 mg/kg)
- Ketoconazole; 400-800 mg daily for a minimum of 6 mo
- Fluconazole; 200-400 mg daily for a minimum of 6 mo
- Patients with AIDS require lifelong suppressive treatment with daily itraconazole at a dose of 200 mg orally after completing initial treatment with amphotericin B. The efficacy and safety of itraconazole preparations have not been established in chldren. A few pediatric patients 3-16 years old have been treated with oral itraconazole (100 mg/d) for systemic fungal infections with no serious unexpected adverse effects.
- Itraconazole may not be an effective agent for central nervous system infection. See footnote 1 for pediatric patients.
- Fluconazole should probably not be used, if possible, in treatment of life-threatening blastomycosis.
BOX 3. Control of Blastomycosisx
Precautions
At-risk individuals residing in endemic areas should avoid activities such as exposure to dust, construction, or excavation
Prophylaxis
AIDS patients with blastomycosis should receive lifelong suppressive treatment with 200 mg of itraconazole1 daily by mouth after completionof initial therapy
- The efficacy and safety of itraconazole preparations have not been established in children. A few pediatric patients 3-16 years old have been treated with oral itraconazole (100 mg/d) for systemic fungal infections with no serious unexpected adverse effects.
Read More
http://www.antimicrobe.org/f02.asp
https://microbewiki.kenyon.edu/index.php/Blastomyces_dermatitidis
http://www.mdedge.com/idpractitioner/dsm/1522/infectious-diseases/blastomyces-dermatitidis