Description of Medical Condition
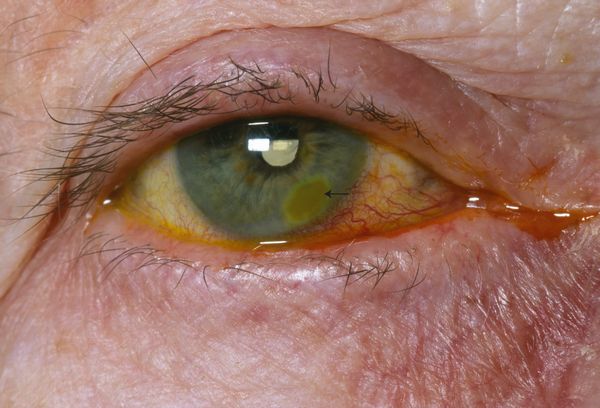
Corneal ulcers represent an infection of the cornea by bacteria, virus or fungi as a result of breakdown in the protective epithelial barrier. If left untreated, corneal ulcers can result in blindness. Ulcerations may be central or marginal.
System(s) affected: Nervous
Genetics: None
Incidence/Prevalence in USA: Common
Predominant age: None
Predominant sex: Male = Female
Medical Symptoms and Signs of Disease
- Eyelid and conjunctiva become inflamed
- Mucopurulent discharge
- The corneal epithelium will be absent with underlying ulceration and infiltration of the corneal stroma with leukocytes
- Foreign body sensation
- Blurred vision
- Light sensitivity
- Pain
What Causes Disease?
Corneal ulcers are predisposed by the presence of an entry to the external eye. Dry eye, burns, abrasion, contact lenses, inappropriate use of topical anesthetics, antibiotics, or antiviral drops, immunosuppressant drugs, diabetes, immunodeficiency.
Causative agents for foreign entry:
- Gram positive organisms (staphylococci, streptococci, and bacilli)
- Anaerobes (cocci, bacilli)
- Gram negative organisms (diplococcus, rods, and anaerobes)
- Pseudomonas
- Viruses such as herpes

Risk Factors
- Any abrasive injury
- Contact lenses (especially soft lenses)
- Chronic topical steroid use
Diagnosis of Disease
Differential Diagnosis
Identify infecting organisms
Laboratory
Culture the ulcer
Drugs that may alter lab results: Pretreatment with topical antibiotics or corticosteroids may delay diagnosis
Disorders that may alter lab results: N/A
Pathological Findings
Scrapings for Gram’s and Giemsa’s stain may demonstrate bacteria, yeast, or intranuclear inclusions which may aid in the diagnosis
Diagnostic Procedures
Scrapings of the corneal ulcer may be necessary to identify the underlying organism. The sample should be plated onto the culture media directly.
Treatment (Medical Therapy)
Appropriate Health Care
- Outpatient or inpatient for severe ulcer or noncompliant patient
- All cases of corneal ulceration should be promptly referred to an ophthalmologist
General Measures
- Aggressive topical antibiotic treatment directed toward the causative agent should be instituted immediately while culture studies are pending
- Supplemental topical cycloplegia reduces the inflammation and aids in patient comfort
- Bandaging the eye should be avoided and topical steroids should never be used. Daily evaluation is necessary and prompt consultation with an ophthalmologist or corneal specialist is advised.
Activity
Reduced, until vision returns to normal and healing is complete
Diet
No special diet
Patient Education
Prevention of abrasions and proper handling of contact lenses can prevent recurrence of corneal ulcers
Medications (Drugs, Medicines)
Drug(s) of Choice
- Sulfacetamide 10% suspension (bacteriostatic) is only good for low grade conjunctival infections
- Topical gentamicin and tobramycin are effective against Pseudomonas, Enterobacter, Klebsiella, and aerobic gram negative organisms, while cephalosporins (e.g. cefazolin 50 mg/mL) may be effective against many gram negative organisms. The combination aminogly-coside and cephalosporin may be the most appropriate initial therapy.
- Topical quinolones, e.g., ciprofloxacin (Ciloxan) 0.3%. ofloxacin (Ocuflox) 0.3%, gatifloxacin (Zymar), levofloxacin (Quixin), moxifloxacin (Vigamox). These may be treatment of choice for Pseudomonas infections.
- Ointments, e.g. bacitracin, erythromycin, polymyxin B/bacitracin combos (Neosporin)
- Fungal keratitis needs to be treated with parenteral amphotericin B for Candida and aspergillus; clotrimazole,miconazole, econazole, and ketoconazole may also be required
Contraindications: Refer to manufacturer’s profile of each drug
Precautions: Refer to manufacturer’s profile of each drug
Significant possible interactions: Refer to manufacturer’s profile of each drug
Alternative Drugs
N/A
Patient Monitoring
The patient should be monitored at least daily until healed
Prevention / Avoidance
Avoid corneal abrasion or injury and improper contact lens handling
Possible Complications
Scarring of the cornea and loss of vision
Expected Course / Prognosis
- Corneal ulcerations should improve daily and heal with appropriate therapy
- If healing does not occur or the ulcer extends, then consideration should be given to an alternative diagnosis and treatment
Miscellaneous
Associated Conditions
Chronic ulcerations may be associated with neurotrophic keratitis due to lack of fifth nerve innervation of the cornea. Individuals with thyroid disease, diabetes, immunosup pressive conditions are particularly at risk.
Age-Related Factors
Pediatric: N/A
Geriatric: Ring ulceration more common
Pregnancy
N/A
International Classification of Diseases
370.00 Corneal ulcer, unspecified



