Penicillin G
Penicillin G is an acid that is combined with sodium, potassium, procaine, or benzathine to increase its stability or to regulate its absorption. The latter two are “long-acting” forms. Penicillin G is useful in the treatment of streptococcal infections due to S. pyogenes (group A), S. agalactiae (group B), S. pneumoniae, viridans streptococci, Corynebacterium diphtheria, N. meningitidis, many strains of N. gonorrhea, Treponema pallidum, and many anaerobic streptococci, such as peptococcus and peptostreptococcus. In combination with aminoglycosides, any penicillin G compounds can be used to treat enterococci and L. monocytogenes infections. These organisms cause many clinical syndromes including cellulitis, pharyngitis, pneumonia, septicemia, endocarditis, meningitis, abscesses in lung, sexually transmitted disease, septic arthritis, and osteomyelitis.
All penicillinlike agents kill susceptible bacteria by interfering with the biosynthesis of the cell wall, eventually lysing the bacteria by autolysis. The penicillins are generally safe except in less than 0.01% of patients who are susceptible to IgE-mediated anaphylaxis. Other types of penicillin toxicity are rare unless renal function has been impaired. In patients with renal failure, large doses of penicillin produce neurologic reactions including seizures. One overlooked problem of high concentrations of penicillin in the blood occurs when aminoglycoside concentrations are measured in vitro. The penicillins autolyze aminoglycosides. Prolonged storage of blood containing these antibiotics at room temperature can result in lower-than-real concentrations of aminoglycoside.
Phenoxymethylpenicillin (penicillin V) is produced by addition of a phenoxyacetic acide. It is more resistant to gastric acid than is penicillin G and is administered orally. Phenoxymethylpenicillin is useful for treatment of minor infections such as streptococcal pharyngitis or cellulitis.
Semisynthetic penicillins
Methicillin, oxacillin, cloxacillin, dicloxacillin, and nafcillin are semisynthetic penicillins that are particularly useful in treating penicillinase-producing staphylococcis.
They are considered the primary empirical and definitive therapy for staphylococcal infections. They kill bacteria in a manner similar to that of penicillin G. Methicillin and nafcillin are the most stable; nafcillin is most often used because of its lower incidence of nephrotoxicity. In contrast to the other semisynthetic penicillins that are excreted primarily by the kidney, nafcillin is 70% inactivated in the liver. Nafcillin does not usually require adjustment of dose in patients with renal failure. Errors in its administration are commonly made by decreasing the dose of nafcillin in patients with renal failure and continuing high doses in patients with hepatic insufficiency.
Depending on subsequent culture results, tailored therapy for staphylococci may include penicillin G (rare) for non-penicillinase-producing strains of staphylococci or vancomycin for nafcillin-resistant staphylococci (usually referred to as MRSA, or methicillin-resistant Staphylococcus aureus because test discs contain methicillin). Dicloxacillin is the most useful agent of this group for oral therapy. Cloxacillin can also be given orally and in many countries is more readily available than is dicloxacillin.
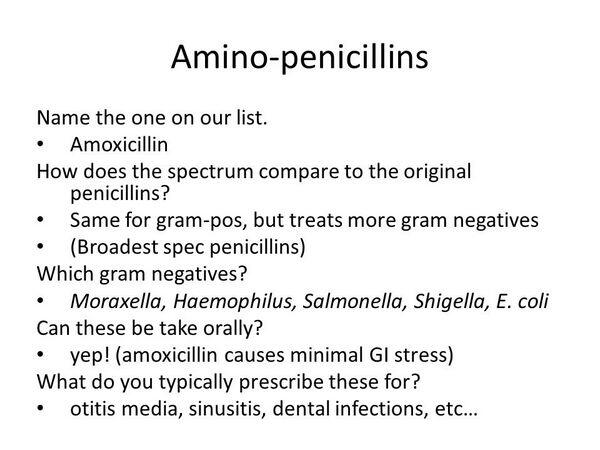
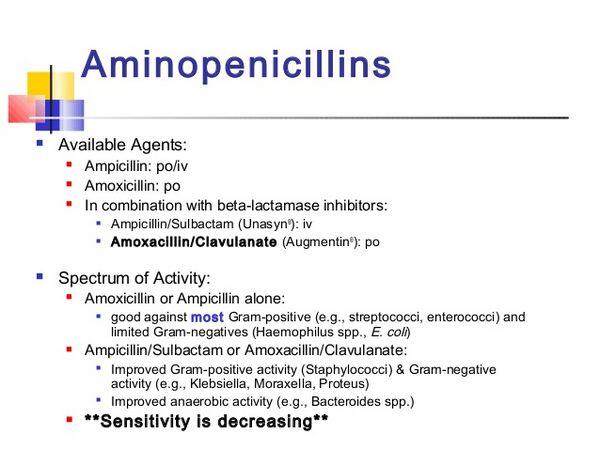
Amino-penicillins
Ampicillin is a semisynthetic penicillin and is unique in that it is active against some gram-negative bacilli that are resistant to penicillin G. Amoxicillin is chemically modified ampicillin. The trihydrate form is administered orally and is much better absorbed than ampicillin, making it the preferred agent for oral administration. Organisms that are susceptible to penicillin G also are susceptible to ampicillin. Ampicillin kills organisms similarly to penicillin G; however, it penetrates into the cell wall better, enabling it to kill many gram-negative bacilli. It is considered appropriate therapy for susceptible E. coli, P. mirabilis, and species of Shigella, Neisseria gonorrhoeae, and N. meningitidis.
The most common error in parenteral ampicillin therapy is administrating it too infrequently. Its relatively short half-life dictates that it should be administered every 4 hours in seriously ill patients. It is especially useful in treating acute and uncomplicated urinary tract infections caused by E. coli and/or Proteus species. Haemophilus influenzae meningitis can be treated with ampicillin if the organisms do not produce β-lactamase.
Extended-spectrum penicillins
Carboxypenicillins (carbenicillin, ticarcillin) and ureidopenicillins (mezlocillin, azlocillin, and piperacillin) are semisynthetic penicillins that must be administered parenterally and are particularly useful to treat serious aerobic gram-negative infections of the lung, abdomen, pelvis, muscle, skeleton, and bloodstream. Ureidopenicillins also have activity against many anaerobes and streptococci, including enterococci. Their primary clinical usefulness relies on their enhanced ability to kill aerobic gram-negative organisms, including species of E. coli, Proteus, P. aeruginosa, other species of Pseudomonas, H. influenzae, and species of Klebsiella. By themselves, these agents usually are sufficient to kill these organisms with the notable exception of P. aeruginosa.
Serious infections with Pseudomonas usually require the synergistic effects of one of the semisynthetic penicillins plus an aminoglycoside. Carbenicillin is now rarely used because it contains considerable amounts of sodium. Ureidopenicillins have better bactericidal activity against species of Pseudomonas and other gram-negative bacteria. All these agents are susceptible in varying degrees to inactivation by bacterial β-lactamases, the means of bacterial resistance to these agents.


 (2 votes, average: 4.50 out of 5)
(2 votes, average: 4.50 out of 5)

