Description of Medical Condition
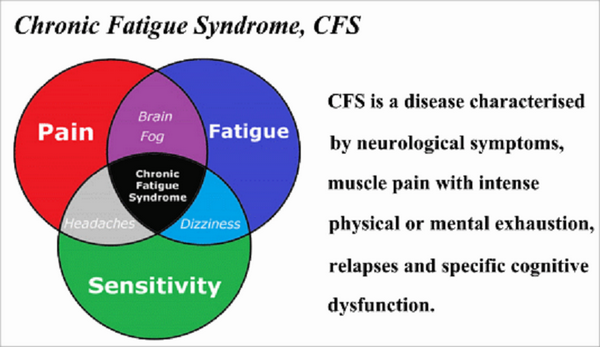
Chronic fatigue syndrome (CFS) is characterized primarily by profound fatigue, in association with multiple systemic and neuropsychiatric symptoms, lasting at least 6 months. The fatigue must have a new or definite onset (i.e., not lifelong), is not relieved by rest, and results in a substantial reduction in previous activities (occupation, education, social, and personal).
System(s) affected: Endocrine/Metabolic, Musculoskeietal
Genetics: N/A
Incidence/Prevalence in USA: 10/100,000
Predominant age: Young adult
Predominant sex: Female > Male (slightly)
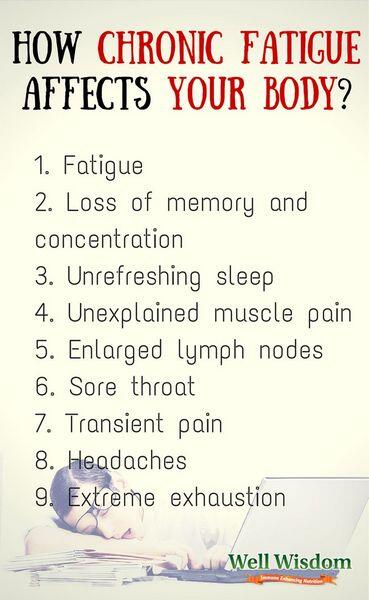
Medical Symptoms and Signs of Disease
- Fatigue (100%)
- Ability to date onset of illness (100%)
- Unexplained general muscle weakness (90%)
- Arthralgias (90%)
- Forgetfulness (90%)
- Inability to concentrate (90%)
- Emotional lability (90%)
- Myalgias (90%)
- Confusion (90%)
- Mood swings (90%)
- Low-grade fever (37.5-38.6°C) (85%)
- Irritability (85%)
- Prolonged fatigue lasting 24 hours after exercise (80%)
- Depression (80%)
- Headaches (76%)
- Photophobia (76%)
- Difficulty sleeping (76%)
- Allergies (70%)
- Vertigo (40%)
- Adenopathy (40%)
- Shortness of breath (33%)
- Chest pain (33%)
- Nausea (33%)
- Weight loss (30%)
- Hot flushes (30%)
- Palpitations (30%)
- Painful lymph nodes (30%)
- Gastrointestinal complaints (30%)
- Night sweats (25%)
- Weight gain (15%)
- Rash (15%)
What Causes Disease?
Unknown. Multiple immunologic abnormalities suggestive of viral reactivation syndrome have been reported. Attention has been to viruses (EBV, HHV-6, enteroviruses), possibly in concert, possibly with environmental factors. No infectious agent has been implicated in the syndrome.
Risk Factors
Some studies have found an increased risk of developing chronic fatigue syndrome in patients who had a history of childhood abuse or trauma
Diagnosis of Disease
Differential Diagnosis
- Malignancies
- Autoimmune disease
- Localized infection (occult abscess, etc.)
- Chronic or subacute bacterial disease (endocarditis)
- Lyme disease
- Fungal disease (histoplasmosis, coccidioidomycosis)
- Parasitic disease (amebiasis, giardiasis, helminths)
- HIV related disease
- Psychiatric disorders
- Drug dependency or abuse (including prescription drugs)
- Depression
- Hypochondriasis
- Anxiety disorders
- Somatization disorder
- Chronic inflammatory disease (sarcoidosis, Wegener granulomatosis)
- Known chronic viral disease (chronic hepatitis)
- Neuromuscular disease (multiple sclerosis, myasthenia gravis)
- Endocrine disorder (hypothyroidism, Addison, Cushing. diabetes mellitus)
- latrogenic (as from medication side effects)
- Toxic agent exposure
- Other known or defined systemic disease (chronic pulmonary, cardiac, hepatic, renal, or hematologic disease)
- Physiologic (inadequate or disrupted sleep, menopause, etc.)
Laboratory
- Initial lab studies
- Chemistry panel OCBC
- Urinalysis
- Thyroid function
- Additional studies OESR
- ANA
- VDRL
- Rheumatoid factor
- Purified protein derivative
- Serum cortisol
- HIV
- lmmunoglobulin
- Epstein-Barr serology
Drugs that may alter lab results: N/A
Disorders that may alter lab results: N/A
Pathological Findings
N/A
Special Tests
None. Diagnosis of exclusion. History, physical exam normal.
Imaging
Experimental at present
Diagnostic Procedures
To establish the diagnosis — 2 major criteria and at least 6 symptoms plus at least 2 physical signs; or at least 8 symptoms
Major criteria:
- new onset fatigue lasting longer than 6 months with a 50% reduction in activity
- No other medical or psychiatric conditions that could cause symptoms
Symptoms:
- Low grade fever
- Sore throat
- Painful cervical or axillary adenopathy
- Generalized muscle weakness
- Myalgias
- Headaches
- Migratory arthralgias
- Sleep disturbances (hypersomnia or insomnia)
Oneuropsychological complaints (one or more of: photophobia, visual scotomas, forgetfulness, irritability, confusion, difficulty concentrating, depression)
Physical signs:
- Low grade fever (37.5-38.6°C)
- Pharyngitis (nonexudative)
- Cervical or axillary adenopathy
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient
General Measures
- Because the cause of CFS is unknown and no specific therapy has shown consistent results, mainstay of therapy is supportive care
- A program of moderate exercise (with rest periods during exacerbations of the disease), a healthy diet, stress reduction, and support groups or counseling is likely to be beneficial and while not necessarily curative will help the patient cope with their disease
- Alternative therapies (chiropractic, homeopathy, acupuncture, enforced rest, guided image hypnosis, yoga, massage therapy) helpful for some; may be worth trying
- Psychiatric symptoms often prominent but generally felt secondary rather than causative, but symptom treatment beneficial
Activity
As tolerated, but strenuous exercise tends to exacerbate symptoms in most
Diet
Rich in vitamins and minerals; fresh fruits and vegetables
Patient Education
- Support groups available. Contact CFS Association. 3521 Broadway, Suite 222, Kansas City, MO 64111 (816)931-4777
- CFIDS Association. P.O. Box 220398, Charlotte, NC 28222-0398
- International Chronic Fatigue Syndrome Society. P.O. Box 230108, Portland, OR 97223
Medications (Drugs, Medicines)
Drug(s) of Choice
- None
- Poly1:polyC12U (Ampligen), essential fatty acid therapy, immune globulin IV, vitamin B12, and bovine liver extract (LEFAC) are used experimentally
- Supportive therapy directed toward symptoms with NSAIDs, antidepressants including fluoxetine, buspi-rone, and others
Contraindications: Refer to manufacturer’s literature
Precautions: Refer to manufacturer’s literature
Significant possible interactions: Refer to manufacturer’s literature
Alternative Drugs
- Anti-inflammatory agents: Omega-3 fatty acids, turmeric, ginger, oregano and barberri
Patient Monitoring
No consensus. Periodic re-evaluation appropriate for support, symptom relief, assessment for other cause.
Prevention / Avoidance
Unknown
Possible Complications
- Depression
- Socioeconomic problems
Expected Course / Prognosis
- Indolent; waxes and wanes
- Generally very slow improvement over months or years
Miscellaneous
Associated Conditions
- Fibromyalgia (70% reported to meet criteria)
- Depression
- Hypochondriasis
Age-Related Factors
Pediatric: Reported in children
Geriatric: Reported in elderly
Pregnancy
No information
Synonyms
- CFS
- Chronic Epstein-Barr syndrome
- Yuppie flu
International Classification of Diseases
300.5 Neurasthenia
780.71 Chronic fatigue syndrome
See Also
- Epstein-Barr virus infections
- Depression
- Fibromyalgia
Other Notes
Controversial topic, data often conflicting
Abbreviations
CFS = chronic fatigue syndrome

