Description of Medical Condition
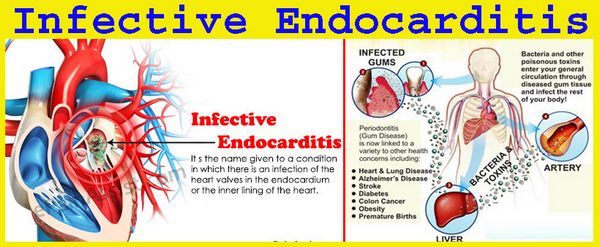
A disease resulting from infection primarily of the valvular endocardium and occasionally the mural endocardium
System(s) affected: Cardiovascular, Skin/Exocrine, Pulmonary, Endocrine/Metabolic, Renal/Urologic, Hemic/Lymphatic /lmmunologic
Genetics: Unknown
Incidence/Prevalence in USA: 1.7-4.2/100,000; 0.32-1.3/1000 hospital admissions
Predominant age: All ages
Predominant sex: Male > Female (slightly)
Medical Symptoms and Signs of Disease
- Fever, may be high, low or absent. May be only symptom in prosthetic valve endocarditis.
- Night sweats, chilly sensation
- Malaise, myalgia, joint pain
- Back pain, may be severe
- Anorexia, weight loss
- Delirium, headache
- Paralysis, hemiparesis, aphasia
- Numbness, muscle weakness
- Cold extremity with pain
- Bloody urine, may be gross or microscopic
- Bloody sputum, from septic pulmonary emboli
- Petechiae
- Conjunctival hemorrhage
- Hemorrhagic or necrotic pustule
- Pain of finger tip, or toe tip (subjective symptom of Osier node)
- Chest pain, shortness of breath, cough
- Roth spot
- Osier node
- Janeway lesion
- Heart murmur, may be absent
- Pericardial rub
- Pleural friction rub
- Splenomegaly
What Causes Disease?
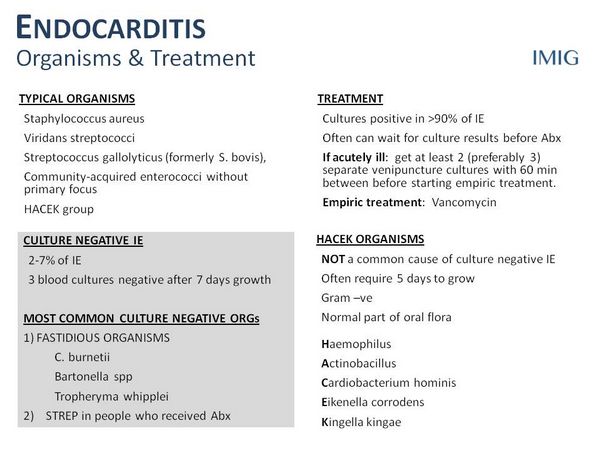
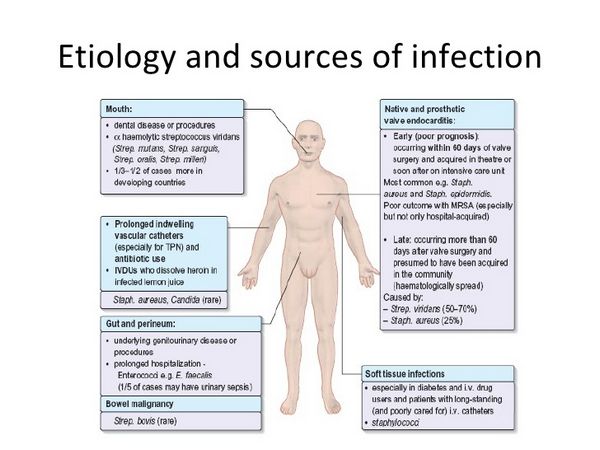
- Acute endocarditis (often an aggrressive course and may not be associated with an underlying valve lesion)
- Staphylococcus aureus
- Streptococcus groups A, B, C, G
- Haemophilus influenzae or parainfluenzae
- Streptococcus pneumoniae
- Staphylococcus lugdunensis
- Enterococcus spp (E. faecalis, E. faecium, £ durans) <) Neisseria gonorrhoeae
- Subacute endocarditis (indolent course, often is setting of structural valve disease)
- Alpha-hemolytic streptococci
- Streptococcus bovis
- Enterococcus spp
- Haemophilus aphrophilus or paraphrophilus
- Actinobacillus actinomycetemcomitans
- Cardiobacterium hominis
- Eikenella corrodens
- Kingella kingae
- Staphylococcus aureus
- Endocarditis in intravenous drug-abusers (often involves the tricuspid valve)
- Staphylococcus aureus
- Pseudomonas aeruginosa
- Burkholderia cepacia
- Other gram-negative bacilli
- Enterococcus spp
- Candida spp
- Early prosthetic valve endocarditis (<60 days after valve implantation) – Staphylococcus aureus – Staphylococcus epidermidis – Gram-negative bacilli – Candida spp – Aspergillus spp
- Late prosthetic valve endocarditis (>60 days after valve implantation)
- Alpha-hemolytic streptococci
- Enterococcus spp
- Staphylococcus epidermidis
- Candida spp
- Aspergillus spp
- Culture-negative endocarditis (5-10%)
- Patients on antibiotics
- Bartonella quintana (homeless people)
- Bartonella henselae (cat owners)
- Fastidious organism: Brucella spp, fungi, Coxiella burnetii (Q fever), Chlamydia trachomatis. Chlamydia psittaci, HACEK organisms (Haemophilus species, Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, Kingella spp)
Risk Factors
- Underlying conditions
- Prosthetic cardiac valves, including bioprosthetic and homograft valves
- Previous bacterial endocarditis, even in the absence of heart disease
- Most congenital cardiac malformations
- Rheumatic and other acquired valvular dysfunction even after valvular surgery
- Hypertrophic cardiomyopathy
- Mitral valve prolapse with valvular regurgitation
- Indwelling intravascular devices
- Associated with transient bacteremia
- Gingival irritation, including professional cleaning
- Tonsillectomy and/or adenoidectomy
- Procedures on intestinal or respiratory mucosa
- Rigid bronchoscopy
- Sclerotherapy of esophageal varices
- Esophageal dilatation
- Gallbladder surgery
- Cystoscopy
- Urethral dilatation
- Urethral catheterization in the presence of infection
- Urinary tract surgery in the presence of infection
- Prostatic surgery
- Incision and drainage of infected tissue
- Vaginal hysterectomy
- Vaginal delivery in the presence of infection
Diagnosis of Disease
Differential Diagnosis
- Connective tissue diseases
- Fever of unknown origin
- Intra-abdominal infections
- Rheumatic fever
- Salmonellosis
- Tuberculosis
Laboratory
- Positive blood cultures taken at different times
- 2-dimensional echocardiography, not always positive for vegetations (transesophageal echocardiography has high sensitivity)
- Leukocytosis in acute endocarditis
- Anemia in subacute endocarditis
- Elevated ESR
- Decreased C3, C4, CH50 in subacute endocarditis
- Hematuria, microscopic or macroscopic
- Rheumatoid factor in subacute endocarditis
- Serologies for Chlamydia, Q fever (Coxiella) and Bartonella may be useful in “culture-negative” endocarditis
Drugs that may alter lab results: Antibiotics may make blood cultures falsely negative
Disorders that may alter lab results: N/A
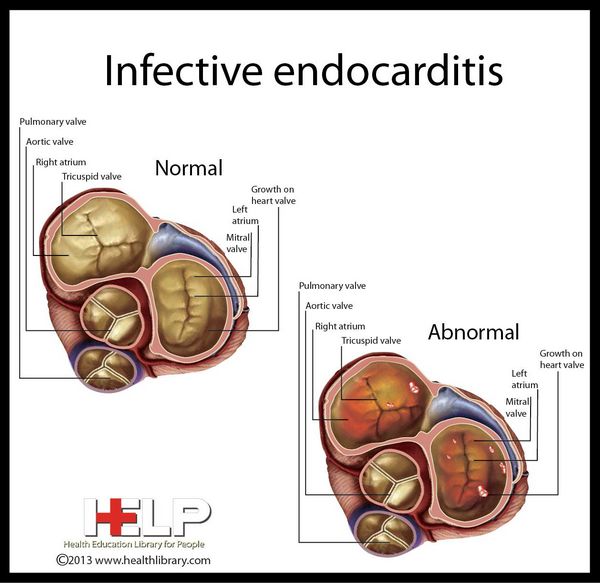
Pathological Findings
- Vegetations are composed of platelets, fibrin and colonies of micro-organisms. Destruction of valvular endocardium, perforation of valve leaflets, rupture of chordae tendineae, abscesses of myocardium, rupture of sinus of Valsalva, pericarditis may occur.
- Emboli, infarction, abscesses and/or infarction may be found in any organ.
- Immune-complex glomerulonephritis possible
Imaging
- Pulmonary ventilation perfusion scan may be useful in right-sided endocarditis
- CT scan may be useful in locating abscesses
Diagnostic Procedures
- Transesophageal echocardiography
- Cardiac catheterization may be indicated to ascertain the degree of valvular damage
- Aortic root injection may be useful when aortic root abscess or rupture of sinus of Valsalva is suspected
Duke criteria for diagnosis of infective endocarditis (2 major criteria, OR 1 major and 3 minor criteria, OR 5 minor criteria)
- Major criteria
- Positive blood culture
- Typical microorganism for infective endocarditis from 2 separate blood cultures, or
- Persistently positive blood culture. Defined as recovery of a microorganism consistent with infective endocarditis from: blood cultures drawn more than 12 hours apart, or all of 3 or a majority of 4 or more separate blood cultures, with first and last drawn at least 1 hour apart
- Positive echocardiogram: (a) oscillating intracardiac mass, on valve or supporting structures, or in the path of regurgitant jets, or on implanted material, in the absence of an alternative anatomic explanation, or (b) abscess, or (c) new partial dehiscence of prosthetic valve
Onew valvular regurgitation (increase or change in pre-existing murmur not sufficient)
- Minor criteria
- Predisposing heart condition or IV drug use
- Fever >38.0°C(100.4°F)
- Vascular phenomena: major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhage, Janeway lesions
- 0Immunologic phenomena: glomerulonephritis, Osier’s nodes, Roth spots, rheumatoid factor
- Microbiologic evidence: positive blood culture, but not meeting major criterion (excluding single positive cultures for coagulase-negative staphylococd and organisms that do not cause endocarditis) or serologic evidence of active infection with organism consistent with infective endocarditis
- Echocardiogram: consistent with infective endocarditis but not meeting major criterion
Treatment (Medical Therapy)
Appropriate Health Care
- Initial hospitalized care
- Intensive care for critically ill patients
- Outpatient home IV antibiotic therapy in selected stable and reliable patients
General Measures
- Treat CHF if it occurs
- Oxygen treatment as needed
- Consider hemodialysis
Surgical Measures
- Valve replacement may be performed before antibiotic treatment course is completed when any of the following are present:
- CHF due to valve incompetence
- Multiple major systemic emboli
- Infection is caused by resistant organisms, e.g. fungus, Pseudomonas aeruginosa
- Dehiscence of infected prosthetic valve
- Relapse of prosthetic valve endocarditis
- Persistent bacteremia despite antibiotics
Activity
- Bedrest is indicated initially
- Ambulation when clinically improved
Diet
No special diet
Patient Education
- Importance of dental hygiene
- Antibiotic prophylaxis when undergoing certain dental/ surgical procedures
- Give patient an AHA wallet card listing antibiotic regimens for prophylaxis. Obtain the AHA wallet card. 78-1005 (CP), from local chapters of American Heart Association.
Medications (Drugs, Medicines)
Drug(s) of Choice
- Penicillin-susceptible streptococci: Penicillin 2-4 million UlV q4h, plus gentamicin for 2 weeks (6 weeks for prosthetic valve endocarditis). In patients with native valve endocarditis: patient > 65 years of age, those with impairment of the eighth nerve or of renal function, or those with central nervous system involvement, use penicillin only, in the same dosage alone for 4 weeks.
- Enterococci: Penicillin 5-10 million U q4h, plus gentamicin or streptomycin for 4-6 weeks (6 weeks for prosthetic valve endocarditis). Test the enterococcal strain in vitro for high-level resistance to gentamicin and streptomycin (minimal inhibitory concentration [MIC] > 2000 /jg/mL). Use streptomycin, 1 gm IM q24h instead of gentamicin if there is high-level resistance to gentamicin and not to streptomycin.
- Staphylococcus of native valve: Oxacillin or nafcillin 2 g IV q4h for 6 weeks. For the first 3-5 days, add gentamicin.
- Staphylococcus of prosthetic valve: Vancomycin 15 mg/kg (usual dose 1 g) IV infused over 1 h q12h, plus rifampin 300 mg po q8h, both for 6 weeks, plus gentamicin for the first 2 weeks
- HACEK organisms: ceftriaxone 2 gm IM or IVq24hfor 4 weeks
Contraindications: For patients who are allergic to penicillin, use alternative drugs
Precautions:
- In patients with renal impairment, dosage adjustment should be made for penicillin G, gentamicin, cefazolin vancomycin
- Rapid infusion of vancomycin (less than one hour) may cause “red-neck syndrome”. This is due to histamine release and not an allergic reaction. It will disappear when the rate of infusion is reduced.
Significant possible interactions:
- Vancomycin plus gentamicin increases renal toxicity
- Rifampin increases the requirement for coumarin and oral hypoglycemic agents
Alternative Drugs
- For patients allergic to penicillin
- Penicillin-susceptible streptococci: ceftriaxone 2 g IM or IV qday for 4 weeks or ceftriaxone 2 g IV plus gentamicin 3 mg/kg qday for 2 weeks (not to be used in patients with immediate type hypersensitivity to penicillin), or vancomycin 15 mg/kg (usual dose 1 g) IV over 1 hr q12h for 4 weeks (6 weeks for prosthetic valve endocarditis)
- Enterococci: Desensitization to penicillin should be considered. Vancomycin 15 mg/kg (usual dose 1 g) IV infused over 1 hr q12h, plus gentamicin (see Other Notes) for 4-6 weeks (6 weeks for prosthetic valve endocarditis).
- Staphlococcus of native valve: Cefazolin 2 gm IV q8h (not to be used in patients with immediate-type hypersensitivity to penicillin), or vancomycin 15 mg/kg (usual dose 1 g) IV infused over 1 hrq12h, for 6 weeks
Patient Monitoring
- Check gentamicin peak (approx 3 /jg/mL) and trough (<1 |Ug/mL) levels if used for more than 5 days, and in patients with renal dysfunction.
- Check vancomycin peak (30-45 /jg/mL) and trough (<10 |Ug/mL) levels in patients with renal dysfunction.
- Perform twice weekly BUN and serum creatinine while the patient is receiving gentamicin
- Consider audiometry baseline and follow-up during long-term aminoglycoside therapy
Prevention / Avoidance
- Treat dental caries while the patient is being treated for endocarditis
- Maintain good oral hygiene
- Give antibiotic prophylaxis to patients undergoing procedures that may cause transient bacteremia
- Antibiotic regimen for dental/oral/upper respiratory tract procedures: (may be used in patients with prosthetic valves)
- Amoxicillin 2 g po (or for penicillin allergic patients, clindamycin 600 mg po) 1 hr before procedure
- Alternative: Ampicillin 2.0 g IV (or IM) (or for penicillin allergic patients clindamycin 600 mg IV) 30 minutes before procedure
- Antibiotic regimen for GU/GI procedures
- Ampicillin 2 g IV (or IM) plus gentamicin 1.5 mg/kg IV (or IM) (not to exceed 120 mg) 30 minutes before procedure
- For patients allergic to penicillin: vancomycin 1.0 g IV infused over 1 hr plus gentamicin 1.5 mg/kg IV (or IM) (not to exceed 120 mg); complete infusion 30 minutes before procedure
- Alternate oral regimen for moderate-risk patients undergoing GU/GI procedures
- Amoxicillin 2.0 g po 1 hr before or ampicillin 2 g IV (or IM) 30 minutes before procedure
- For patients who are allergic to penicillin: vancomycin 1.0 g IV infused over 1 hr; complete infusion 30 minutes before procedure
Possible Complications
- Arterial emboli and infarcts (e.g., Ml, mesenteric splenic, cerebral infarct)
- Infectious emboli (e.g., abscesses of heart, lung, brain, meninges, bone, pericardium)
- Inflammatory/immune disorders (e.g., arthritis, myositis. glomerulonephritis)
- Miscellanous complications (e.g., congestive heart failure, ruptured valve cusp, sinus of Valsalva aneurysm cardiac arrhythmia, ruptured mycotic aneurysm)
Expected Course / Prognosis
- Staphylococcal endocarditis, fever and positive blood cultures may persist up to 10 days after appropriate treatment started
- Streptococcal endocarditis, clinical response expected within 48 hours of antibiotic treatment and blood cultures negative soon after antibiotics
- Prognosis depends largely on complications
Miscellaneous
Associated Conditions
- Substance abuse
- Central vascular access
Age-Related Factors
Pediatric: N/A
Geriatric: Prognosis is worse in elderly
Pregnancy
Use gentamicin with caution
Synonyms
- Bacterial endocarditis
- Subacute bacterial endocarditis
- Acute bacterial endocarditis
International Classification of Diseases
421.0 Acute and subacute bacterial endocarditis
421.9 Acute endocarditis, unspecified
996.61 Infection and inflammatory reaction due to cardiac device, implant, and graft
See Also
Bartonella infections Brucellosis
Abbreviations
IE = Infective endocarditis
ABE = Acute bacterial endocarditis
SBE = Subacute bacterial endocarditis