Overview
Amoxicillin/Clavulanate.Piperacillin/Tazobactam
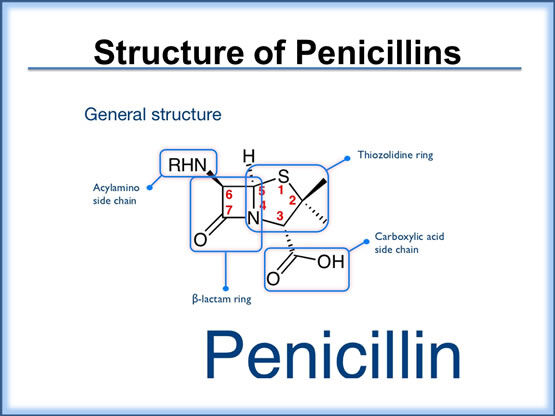
The penicillins comprise several subgroups of agents with a wide range of bacterial coverage and efficacy. Each penicillin molecule contains a basic β-lactam structure fused to a five-membered ring. Because of their broad spectrum of activity and availability in oral form, the penicillins are commonly used in the treatment of acute exacerbations of chronic bronchitis and have become the drugs of choice in treating many common infections.
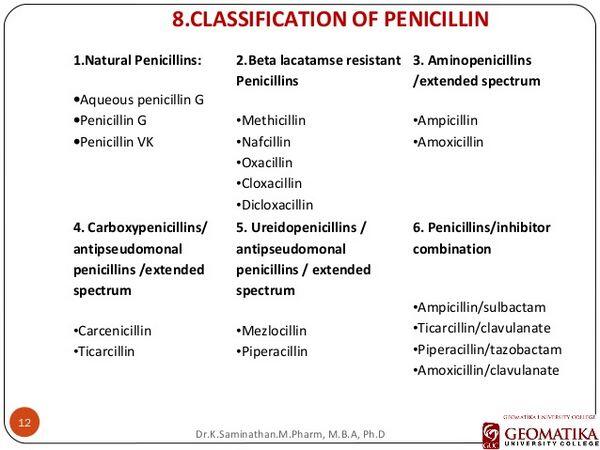
The penicillins are further divided into the following groups: natural penicillins, aminopenicillins, and the extended-spectrum penicillins. The natural penicillins (e.g., penicillin G) have the narrowest spectrum. They are active only against the gram-positive cocci and, with regard to acute exacerbations of chronic bronchitis, active essentially only against S. pneumoniae.
The aminopenicillins (such as ampicillin and amoxicillin) are natural penicillin derivatives with an expanded spectrum of activity that includes some gram-negative organisms that do not produce β-lactamases-enzymes that destroys the ring structure of the antibiotic rendering it ineffective — including H. influenzae. The aminopenicillins have been in use since the 1970s, and they continue to be valuable therapeutic agents for the treatment of many bacterial infections. These drugs are sometimes used as first-line agents in the treatment of mild-to-moderate acute exacerbations of chronic bronchitis when no other risk factors are apparent. However, the usefulness of aminopenicillins is increasingly limited in countries such as France and Spain because of resistance among the common respiratory pathogens but they continue to be used owing to their inexpensiveness.
The extended-spectrum penicillins (such as pipericillin and ticarcillin) are semisynthetic and have a broad range of activity including many gram-negative organisms, such as Escherichia coli and K. pneumoniae. These drugs are more active than natural penicillins and aminopenicillins because they are more resistant to inactivation by β-lactamases and/or because they more readily penetrate the outer membranes of gram-negative bacilli. Nonetheless, their rate of bactericidal action and the completeness of this effect can be inconsistent.
As a class, the penicillins are among the safest antibiotics. However, one potentially life-threatening adverse effect associated with their use is immediate or delayed hypersensitivity reactions in a small percentage of patients. These reactions can present in a variety of forms, such as mild skin rash, interstitial nephritis, hematological disturbances (e.g., neutropenia), vasculitis, and anaphylactic shock. The overall incidence of hypersensitivity reactions ranges between 0.7% and 10% of patients treated with penicillins. Other more common, yet minor, side effects caused by penicillins are GI disturbances (e.g., nausea, vomiting, diarrhea).
A growing concern over the past two decades has been the development of bacterial resistance to the penicillins — particularly in penicillin-resistant S. pneumoniae (PRSP). Penicillin drug resistance is caused by altered penicillin binding proteins in the cell wall of resistant organisms that result in decreased affinity of the antibacterials to their targets. Resistance to penicillins (as well as their dosing schedule and frequency of GI side effects) has resulted in switching to newer-generation drugs such as the fluoroquinolones, which have better activity against resistant strains of pathogens. In many cases, however, physicians are instead employing higher doses of penicillins and/or using penicillin/penicillinase inhibitors to provide adequate coverage and overcome potential resistance issues.
Ticarcillin/clavulanate (GlaxoSmithKline’s Timentin) is an injectable extended-spectrum penicillin/beta-lactamase inhibitor used in severe, complicated hospitalized cases of acute exacerbations of chronic bronchitis. For acute exacerbations of chronic bronchitis, it is used in similar settings as pipericillin/tazobactam (Wyeth/Taisho’s Zosyn) and will not be discussed in greater detail because of its limited use. Likewise, ampicillin/sulbactam (Pfizer’s Unasyn, generics), an injectable aminopenicillin/beta-lactamase inhibitor that has activity against gram-positive and some gram-negative organisms similar to amoxicillin/clavulanate, will not be discussed further.
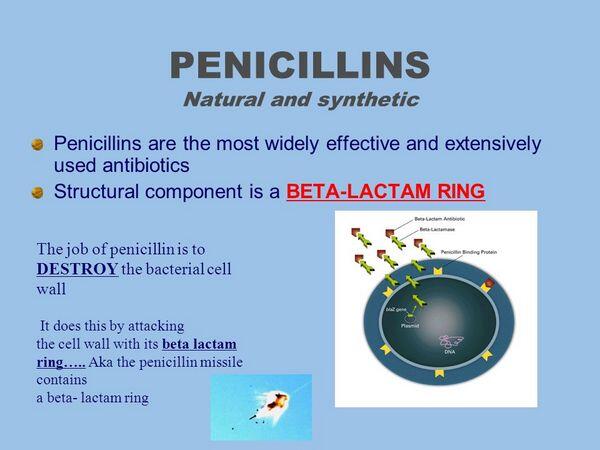
Mechanism Of Action
Penicillins and related β-lactam antibacterials bind to penicillin binding proteins in bacteria and prevent bacterial cell-wall formation. The penicillin binding proteins are enzymes that reside on the inner wall of the bacterial cell membrane and serve to maintain cell-wall homeostasis, including structural integrity, cell shape, cell division, capsule synthesis, phage resistance, and regulation of autolysis. The β-lactam ring of penicillins interacts with penicillin binding proteins and inhibits cell-wall synthesis, thereby killing the cell. Most bacteria contain between four and eight different penicillin binding proteins; hence antibiotics against the penicillin binding proteins have to target several different proteins. Organisms that are metabolically inactive and those lacking bacterial cell walls (e.g., Mycoplasma) are not susceptible to β-lactam antibacterials.
Amoxicillin
Amoxicillin (GlaxoSmithKline’s Amoxil, generics) is available in a capsule, chewable tablet, or oral suspension. It is an amino penicillin derivative that is active against gram-positive organisms and some gram-negative strains that do not produce β-lactamases, such as H. influenzae, but not K. pneumoniae or P. aeruginosa. Amoxicillin has been commercially available since 1974 and continues to be a valuable therapeutic agent for the treatment of many bacterial infections. As a β-lactam antibiotic, amoxicillin binds to penicillin binding proteins in bacteria and prevents bacterial cell-wall formation. Amoxicillin is not often used for acute exacerbations of chronic bronchitis because of the rising prevalence of β-lactamase-producing H. influenzae.
In a randomized multicenter trial, 143 subjects with acute exacerbations of chronic bronchitis were treated with 250 mg of cefuroxime axetil (GlaxoSmithKline’s Ceftin/Zinnat/Oracef) twice daily and 153 subjects received 250 mg of amoxicillin three times daily. Results showed that 76.2% of subjects treated with cefuroxime axetil were cured or saw clinical improvement compared with 80.4% in the amoxicillin arm.
Side effects associated with amoxicillin are minimal, with some incidence of diarrhea. There are instances of skin rashes, and particularly delayed responses. Amoxicillin is typically well absorbed from the GI tract, has a rapid onset and long duration of action, requires less frequent dosing, and has a favorable side-effect profile. As a generically available product, amoxicillin is also relatively inexpensive. Unfortunately, bacterial resistance to amoxicillin has increased significantly, both among H. influenzae and S. pneumoniae, resulting in a switch toward newer-generation drugs that are active against these pathogens.




