VIBRIO CHOLERAE INFECTIONS
Essentials of Diagnosis
- History of exposure, particularly travel to endemic or epidemic locales.
- Acute onset of voluminous, watery diarrhea, with low-grade fever and mild abdominal pain, which are disproportionate to the amount of diarrhea.
- During outbreaks, the presence of straight-to-curved gram-negative bacilli, with a single polar flagellum, in the stool of infected patients.
- In wet preparations, these organisms demonstrate a characteristic darting or “shooting star” motility. The identification may be confirmed by motility inhibition with specific antisera.
- Cultures of V cholerae from stool with differential media, such as thiosulfate-citrate-bile salts-sucrose (TCBS) medium.
- Bacterial growth in nutrient broth, without 1% NaCl supplementation. This characteristic is useful for separating V cholerae from most other Vibrio species.
- Detection of V cholerae toxin by latex agglutination or enzyme-linked immunosorbent assay (ELISA) or the detection of V cholerae-specific nucleic acid sequences by polymerase chain reaction (PCR)-based methods.
General Considerations
Epidemiology
Cholera is a disease of antiquity and probably represents some of the diarrheal illnesses described by Hippocrates and other early physicians. Robert Koch discovered V cholerae in 1884. Since the 17th century, at least eight epidemics of cholera have swept the globe. At least seven of the eight pandemics originated from the Ganges River delta, where cholera is endemic. V cholerae is transmitted by the fecal-oral route, often by way of contaminated water supplies.
The areas where cholera remains endemic lack adequate sewage disposal systems and water treatment facilities. Cholera epidemics often occur during war, when basic human needs are not met. Throughout the past 30 years, cholera epidemics have repeatedly occurred in overcrowded refugee camps. In the 1994 Rwandan refugee camps, a significant proportion of the deaths were caused by cholera. During this time, 600,000 people are believed to have been infected with V cholerae 01, which resulted in ~ 45,000 deaths.
Microbiology
The Vibrionaceae share many characteristics with the Pseudomonadaceae and the Enterobacteriaceae. Genera in this family that cause human disease include Vibrio, Aeromonas, and Plesiomonas. The genus Vibrio consists of gram-negative bacilli that are straight or curved and are motile usually by means of a single polar flagellum. Most species are oxidase producers, have the ability to ferment glucose, and can grow in the presence or absence of oxygen.
During cholera outbreaks, the clinical diagnosis may be supported by examination of the stool. In cholera, a preponderance of straight-to-curved gram-negative bacilli with a single polar flagellum may be seen. In wet preparations, these exhibit a characteristic darting or “shooting star” motility. Motility inhibition, after exposure to type-specific antiserum, confirms the identity of these organisms.
The culturing of V cholerae from stool is most effectively achieved with TCBS agar. The colonies of V cholerae are able to ferment the sucrose in TCBS and appear yellow. Suspicious colonies should be subcultured to a nonselective agar, such as blood or chocolate agar, and after sufficient growth is present, oxidase testing and agglutination testing with polyvalent V cholerae antiserum can be performed.
V cholerae and a closely related species, V mimicus, unlike other Vibrio species, are able to grow in nutrient broth without 1% NaCl supplementation. Additional biochemical features, such as the ability to decarboxylate lysine and ornithine and the inability to hydrolyze arginine, are characteristics that may help to separate V cholerae and V mimicus from other vibrios. V cholerae and V mimicus may be easily separated, since V cholerae ferments sucrose, while V mimicus does not.
Vibrio Cholerae Infections: Clinical Syndromes
OTHER VIBRIO INFECTIONS
Essentials of Diagnosis
- History of ingestion of raw or possibly undercooked shellfish and/or exposure to seawater.
- Enteritis: acute onset of predominantly watery diarrhea, which may contain blood and/or neutrophils.
- Extraintestinal: cellulitis, wound infections, or septicemia, which may be associated with multiple bullous to ulcerative skin lesions, especially in patients with liver cirrhosis.
- Culture of etiologic agent, with enhanced growth of most species after NaCl supplementation.
General Considerations
Epidemiology
In the United States and other developed countries, Vibrio-associated disease is caused almost exclusively by species other than V cholerae. These vibrios are normal inhabitants of marine environments and are transmitted to humans through the ingestion of raw or undercooked shellfish, through the contamination of foods by seawater, or through exposure to seawater. These organisms may cause gastroenteritis, soft tissue infections, or both. Diseases caused by these organisms usually occur during summer or early fall. The warmer summer waters may enhance the growth of vibrios and water-associated recreational activities increase the risk of exposure.
Microbiology
As may be expected, the vast majority of these marine vibrios require NaCl for optimal growth. In many instances, these organisms may grow suboptimally on general agar media, unless they are supplemented with NaCl. They grow better on media that contain salt, such as MacConkey and TCBS agar. On MacConkey agar, most of these organisms do not ferment lactose and would be considered possible enteric pathogens. Notable exceptions are Vibrio mimicus and Vibrio vulnificus, which are lactose positive and may be overlooked as normal enteric flora. V mimicus has many biochemical characteristics similar to V cholerae and also grows readily without additional NaCl. V mimicus is readily differentiated from V cholerae on TCBS agar, by its inability to ferment sucrose. The most common vibrio enteric pathogen in the United States, V parahaemolyticus, also is sucrose negative.
If a vibrio infection is suspected, TCBS agar should be used for the detection of possible pathogens. This selective and differential medium inhibits growth of many commensal organisms by the presence of bile (oxygall), sodium cholate, and sodium citrate, while the presence of sucrose and the indicator bromthymol blue allow for the differentiation of sucrose fermenters and nonfermenters. V cholerae, V alginolyticus, and a few other less commonly encountered vibrios are sucrose positive, whereas V parahaemolyticus, V vulnificus, and most of the remaining clinically significant isolates are sucrose negative.
Vibrios are facultative anaerobic gram-negative bacilli, which may appear pleomorphic in Gram stains. The clinically relevant Vibrio species may be subcategorized into six groups based on their growth requirements and ability to perform certain biochemical tests. The key biochemical reactions necessary to separate the vibrios into these six groups include the following: (1) the requirement of NaCl for growth in nutrient broth; (2) oxidase production; (3) nitrate reductive capacity; (4) myo-inositol fermentation; and (5) the presence or absence of arginine dehydrolase, lysine decarboxylase, and ornithine decarboxylase. Additional biochemical reactions may be used for complete speciation.
These tests are used in the microbiology laboratory to exclude certain diagnostic possibilities. Most vibrios are oxidase positive, with the exception of V metschnikovii. With the exception of V cholerae and V mimicus, isolates require 1% NaCl supplementation to adequately perform biochemical tests. The six groups are as follows:
- Group 1 consists of V cholerae and V mimicus. These are readily distinguished from the other vibrios by their ability to grow in nutrient broth, without NaCl supplementation.
- Group 2 consists of V metschnikovii, which is differentiated from other vibrios by its inability to produce oxidase and reduce nitrate to nitrite.
- Group 3 consists of V cincinnatiensis, which is differentiated from other vibrios by its ability to ferment myo-inositol.
- Group 4 consists of V hollisae, which is differentiated from other vibrios by its inability to hydrolyze arginine and to decarboxylate lysine and ornithine.
- Group 5 consists of V damsela, V fluvialis, and V furnissii. Unlike some of the other vibrios, this group produces arginine dihydrolase.
- Group 6 consists of V alginolyticus, V parahaemolyticus, V vulnificus, and V carchariae. These organisms are differentiated from other vibrios by a combination of their ability to produce lysine decarboxylase and their inability to hydrolyze arginine.
CLINICAL SYNDROMES
Noncholera vibrios cause both enteritis and extraintestinal disease (Box 3). In the United States, Vibrio species other than V cholerae are far more common causes of Vibrio-associated gastroenteritis. These agents include V parahaemolyticus, V mimicus, V hollisae, and others. The enteritis caused by these organisms is characterized by fever, mild-to-moderate abdominal pain and cramping, and diarrhea, which may be either watery or bloody. Many of the pathogenic, noncholera vibrios are also halophilic (NaCl enhances growth) and have been associated with the consumption of raw or undercooked shellfish. V parahaemolyticus is the most common cause of shellfish-associated gastroenteritis in the United States. In most instances, the enteritis is self-limited, but complications may occur. Septicemia with severe morbidity and death has occurred following noncholera Vibrio gastroenteritis.
Extraintestinal disease may be caused by V vulnificus or V alginolyticus. These organisms are also halophilic and are associated with shellfish ingestion and saltwater exposure. Manifestations of extraintestinal disease may include wound infections, cellulitis, bullous skin lesions, or septicemia. Patients with cellulitis and wound infections caused by these organisms often report exposure to saltwater. In immunocompromised patients, such as those with cirrhosis or diabetes mellitus, fatal septicemia may occur. If these organisms are suspected clinically, the clinician should notify the laboratory, since NaCl supplementation is required for optimal growth.
CAMPYLOBACTER ENTERITIS
Clinical Findings
Signs and Symptoms
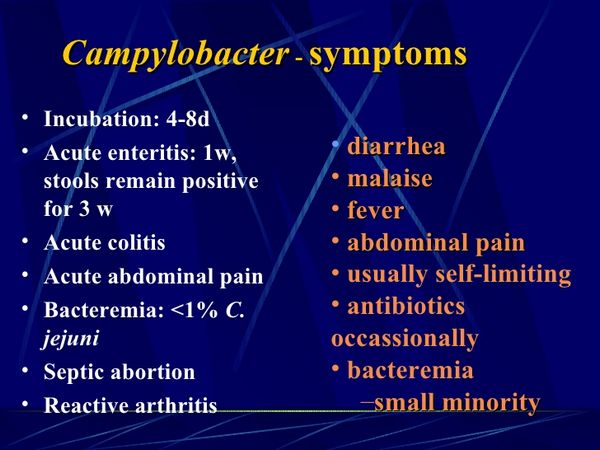
The incubation period for Campylobacter enteritis is between 1 and 7 days. The rapidity of onset and the severity of disease appear to be related to the inoculating dose. Prodromal fever, headache, malaise, and myalgias are often present 1-2 days before the onset of diarrhea. Campylobacter-induced diarrhea is variable in consistency and ranges from watery to bloody. The diarrhea is often accompanied by a low-grade to moderate fever and moderate-to-severe abdominal cramping, which is relieved by defecation. The disease is usually self-limited over several days; however, relapses can occur in 5-10% of untreated patients.
Laboratory Findings
Direct examination of stool specimens often demonstrate curved, vibriolike rods with a characteristic darting motility. Leukocytes are present in 75% of patients with Campylobacter enteritis. Culture on selective media with incubation at 42 °C, in a microaerophilic environment, is used for the enhanced detection of most of the enteropathic Campylobacter species. The most common causes of Campylobacter enteritis, C jejuni and C coli, both grow well at 42 °C in a microaerophilic environment and are resistant to cephalothin. Therefore a selective antibiotic media containing cephalothin is often used. Under these conditions, colonies appear gray and spreading and are oxidase positive. Gram stain reveals gram-negative, curved organisms. The differentiation of C jejuni from C coli depends principally on the ability of the isolate to hydrolyze hippurate (C jejuni subspecies jejuni hydrolyzes hippurate and C coli do not). These techniques, however, will not identify the far rarer cases of enteritis caused by C fetus and some other Campylobacter species, which do not grow well at 42 °C and are inhibited by cephalothin.
Extraintestinal Campylobacteriosis
BOX 1. Clinical Syndromes of Cholera
More Common
- Exposure to unsafe drinking water, particularly in areas where cholera is endemic or epidemic
- Acute onset of watery diarrhea
- Low-grade fever and minimal abdominal pain distinctly out of proportion to the degree of diarrhea
Less Common
- Ileus
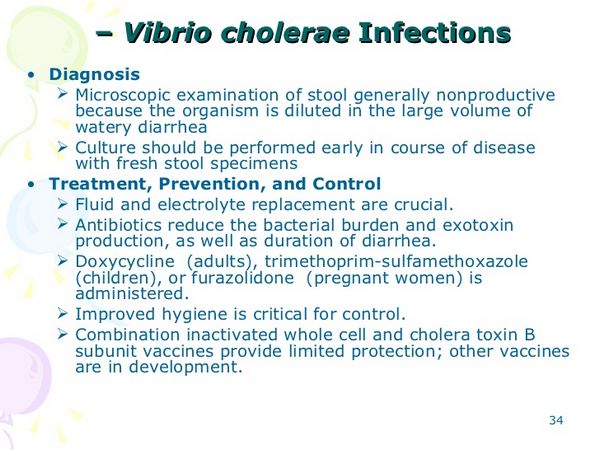
BOX 2. Treatment of Cholera
Fluid and Electrolyte Replacement,
Acid-Base, and Glucose Management
Principal Consideration
Children1
Adults
First Choice
- Ampicillin, 250 mg orally or IV every 6 h for 5 d
- Tetracycline, 250 mg orally or IV every 6 h for 5 d
- During pregnancy, ampicillin is the drug of choice (dosage as below)
Second Choice
- TMP/SMX2 orally or IV (>2 months old); TMP, 3-6 mg, + SMX, 15-30 mg/kg every 12 h for 5 d
- Ampicillin, 250 mg orally or IV every 6 h for 5 d
Penicillin Allergic
- TMP/SMX2 (dosage as above)
OR
- Furazolidone (liquid = 3.33 mg/ml): >5 years old, 7.5-15 ml; 1-4 years old, 5.0-7.5 ml; 1 month-1 year old, 2.5-5.0 ml orally every 6 h for 5 d
- Tetracycline (dosage as above)
OR
- TMP/SMX2 orally or IV: TMP, 160 mg, + SMX, 800 mg orally or IV every 12 h for 5 d
OR
- Furazolidone, 100 mg orally every 6 h for 5 d
1) Tetracycline and the quinolones are generally not given to children because of potential toxicity; however, in cases in which strains of V cholerae are resistant to other drugs and severe disease is present, tetracycline or quinolones may be considered.
2) TMP/SMX, Trimethoprim sulfamethoxazole; treatment may be changed based on susceptibility studies.
BOX 3. Clinical Syndromes of Other Vibrio Species
Enteric Disease
- Recent ingestion of raw or undercooked shellfish
- Acute onset of diarrhea, which is usually watery, but may be bloody and dysenteric
- Low-grade fever, chills, and mild-to-moderate abdominal cramping
Extraintestinal Disease
- Exposure of a wound to seawater or recent ingestion of raw or undercooked shellfish
- Poor wound healing with suppuration, cellulitis, and possibly subcutaneous abscess formation
- A sepsislike syndrome associated with hemorrhagic vesicular or bullous skin lesions, especially in individuals with liver cirrhosis or another immunocompromising condition
BOX 4. Treatment of V vulnificus and V alginolyticus Infections
Surgical Debridement and Abscess Drainage Combined
Principal
Consideration with Antimicrobial
Therapy
Children1
Adults
First Choice
- Cefotaxime IV: newborn to 1 wk, 50 mg/kg/dose every 12 h; 1-4 wk, 50 mg/kg/dose every 8 h; 1 month-12 years & <50 kg, 50-180 mg/kg/d divided every 4-6 h; 1 month-12 years & >50 kg, adult dose until symptoms have subsided
- Tetracycline, 250 mg IV every 6 h until symptoms have subsided
- During pregnancy, cefotaxime is the drug of choice (dosage as below)
Second Choice
- Tetracycline IV: 25-50 mg/kg/d divided every 8-12 h
- Cefotaxime, 2 g IV every 4-8 h until symptoms have subsided
OR
- Ciprofloxacin, 400 mg IV every 12 h until symptoms have subsided
Penicillin Allergic
- Tetracycline (dosage as above)
- Tetracycline (dosage as above)
1) Tetracycline may discolor the teeth of young patients. Treatment may be changed based on susceptibility studies.
BOX 5. Control of Vibrio Infections
Prophylactic Measures
- Clean water and effective sanitation
- Avoidance of raw or undercooked shellfish
- Avoidance of seawater
Isolation Precautions
- Avoidance of stool from infected patients
BOX 6. Clinical Syndromes of Campylobacteriosis
Intestinal (C jejuni)
Extraintestinal (C fetus)
More Common
- Acute onset of diarrhea, which may be watery or bloody
- Associated low-grade-to-moderate fever, nausea, vomiting, malaise, and moderate-to-severe abdominal pain
- Septicemia, fever, chills, and myalgias, without definitive localization
- Endocarditis
- Thrombophlebitis with vessel necrosis
- Fetal loss
Less Common
- Electrolyte abnormalities caused by volume depletion
- Guillain-Barre syndrome
- Pericarditis
- Cellulitis
- Salpingitis
- Reiter’s syndrome
- Meningoencephalitis
- Septic arthritis
- Spontaneous bacterial peritonitis
- Guillain-Barre syndrome
- Osteomyelitis
- Empyema
BOX 7. Treatment of Campylobacteriosis
Children
Adults
First Choice
- Erythromycin, 30-50 mg/kg/d in divided doses
- Erythromycin, 250 mg orally every for 5-7 d 6 h for 5-7 d
Second Choice
- Ciprofloxacin, 500 mg orally every 12 h for 5-7d
BOX 8. Control of Campylobacteriosis
Prophylactic Measures
- Avoidance of undercooked food
- Adequate handwashing


 (1 votes, average: 4.00 out of 5)
(1 votes, average: 4.00 out of 5)


