Essentials of Diagnosis
1) Enteric fever
- Enteric fever is a systemic disease that may or may not be preceded by a diarrheal illness.
- Key signs and symptoms include possible diarrhea or constipation that precedes constitutional symptoms and possible hepatosplenomegaly; other signs and symptoms may include “rose spots,” paroxysmal bradycardia, and mental status changes (so called “typhoid psychosis”).
- Enteric fever is usually associated with the ingestion of water that has been contaminated by human feces.
- “S typhi,” “S paratyphi,” or rarely other Salmonella “species” (see General Considerations section below for clarification of current Salmonella taxonomy) from blood or bone marrow are isolated early in the course of disease and/or from the stool later in the course of disease, or there is molecular evidence of infection.
2) Salmonella enteritis
- Enteritis caused by Salmonella species usually results in watery diarrhea that in some instances may become hemorrhagic or dysenteric.
- Salmonella enteritis is usually associated with the ingestion of contaminated, undercooked foods, particularly undercooked eggs.
- There is microbiologic isolation and identification of Salmonella species or molecular evidence of infection.
General Considerations
For decades, phenotypic studies have been used to identify and categorize the Salmonella species. These organisms have been categorized by antisera directed against particular bacterial somatic (O) and flagellar (H) antigens. Serologic stratification has resulted in the identification of > 2000 Salmonella serotypes. These serotypes have traditionally been treated as individual species. More recently, molecular analysis has revealed significantly less variability among the salmonellae than serologic studies have implied. Newer taxonomy recognizes two Salmonella species, S enterica and S bongori, and six subspecies of S enterica. Although this taxonomy is more precise, many healthcare providers have a greater familiarity with the previous nomenclature. For this reason, reference to previous nomenclature is appropriate and should avoid confusion, facilitate communication, and ensure optimal patient care. Therefore, for the remainder of this chapter, the Salmonella serotypes will be treated traditionally as species.
Epidemiology
Salmonella species cause various clinical manifestations, depending on the infecting serotype, but all commonly begin with oral intake of fecally contaminated food or water. Salmonellosis is usually characterized as enteric fever or enteritis.
Enteric fever
The agents of enteric fever are maintained in a human fecal-oral cycle. Enteric fever, therefore, is most commonly seen in areas of developing countries that lack adequate waste disposal and drinking water treatment facilities. In endemic areas, children and young adults are most commonly affected, but any age and either sex may contract enteric fever. The Indian subcontinent and parts of Africa, Asia, and Central and South America are endemic for enteric fever. In developed countries, clean drinking water and adequate waste disposal have dramatically diminished the prevalence of enteric fever, and most cases of enteric fever are imported from endemic areas.
Enteric fever is distinguished from enteritis if systemic manifestations predominate and there is bacterial dissemination throughout the body and extensive involvement of the reticuloendothelial system. Classically, the enteric fevers are typhoid fever or paratyphoid fever, caused by S typhi or S paratyphi, respectively. Infrequently, other strains may cause enteric fever. S typhi is found exclusively in humans, and S paratyphi is found predominantly in humans. Contraction of disease, therefore, requires the presence of individuals either recovering from enteric fever or harboring the organism. Enteric fever remains a major public health problem in much of the world, and in some areas it ranks among the top five causes of death.
Enteric fever is a severe, life-threatening disease that, despite antimicrobial therapy, still causes significant mortality. Some individuals who have had enteric fever become chronic carriers. These individuals are usually asymptomatic and most frequently harbor the bacteria in the gallbladder, which contains calculi. In areas where Schistosoma haematobium is endemic, the bacteria may also be harbored in the bladder, associated with schistosome eggs. Chronic carriers are public health threats, because they continue to shed pathogenic bacteria into the environment over long periods of time and may substantially contaminate local water supplies, particularly in areas lacking appropriate treatment facilities. If carriers are food handlers and poor hand washers, epidemics may occur through contaminated food.
Salmonella enteritis
Salmonella enteritis is characterized as enteritis if gastrointestinal disease predominates, without extensive involvement of the systemic reticuloendothelial system. Salmonella serotypes, other than S typhi or S paratyphi, are usually responsible for this disorder. Occasionally bacteremia occurs and there may be extraintestinal manifestations caused by seeding of distant organs. In some instances, the intestinal symptomatology may be minimal, and extraintestinal symptomatology may be the primary manifestation.
Although the number of cases of typhoid fever has diminished dramatically over the past 100 years in the United States, the number of cases of nontyphoid salmonellosis continues to increase. These organisms colonize the intestinal tracts of a wide variety of animals and are also transmitted by the fecal-oral route, through the ingestion of contaminated meats and animal products. Some Salmonella serotypes occur in many different animals, whereas others tend to occur in particular animals. For example, S typhimurium and S enteritidis are often associated with chickens, whereas Salmonella arizonae is associated with reptiles.
Person-to-person transmission of Salmonella species among food handlers and healthcare workers is possible but is not a common mode of transmission. Infants and neonates, however, are at an increased risk for infection if exposed to an infected mother or other family members.
Microbiology
Salmonellae are nonfastidious members of the Enterobacteriaceae that will grow on most routine media, including broth-based blood culture systems. Most Enterobacteriaceae ferment lactose, but the vast majority of Salmonella species (99%) do not. This feature has permitted the use of selective and differential agar media to separate these enteric pathogens from the legions of other bacteria present in the stool. MacConkey and EMB agars are the most common media used for this purpose. These agars contain bile salts and/or dyes that suppress the growth of gram-positive bacteria and lactose and pH indicators for the determination of an organism’s ability to ferment lactose. On MacConkey agar, lactose fermenters appear as pink to red colonies, whereas nonlactose fermenters appear clear. On EMB agar, the lactose fermenters appear as blue to violet colonies and may incorporate dyes that are present in the media into the colony, which gives them a green metallic sheen. Bacterial colonies that do not ferment lactose appear light purple to clear.
When plating stool for the detection of Salmonella and/or Shigella species, a moderately or highly selective agar is often used in conjunction with the MacConkey or EMB plates. Moderately selective agars for the isolation of Salmonella and Shigella species include Hektoen-enteric and xylose-lysine-desoxycholate agars. Highly selective media, such as Salmonella-Shigella agar, brilliant green agar, and bismuth-sulfate agar, are most effectively used in outbreak situations. If used appropriately, an enrichment broth, such as selinite broth, may also be used to increase the recovery of Salmonella species from stool.
Bacteria that are suspected to be Salmonella or Shigella species are often then tested in the three-tube set as described above. In the TSI/KIA system, the majority of salmonellae produce an alkaline slant over an acid butt and produce gas. However, strains of S paratyphi A can ferment lactose, which produces an acid over acid reaction. Although most salmonellae produce hydrogen sulfide from sodium thiosulfate metabolism, ~ 90% of S paratyphi A and 50% of S cholerasuis isolates do not. Hydrogen sulfide production is detected by the TSI, KIA, and LIA systems and, when present, reacts with ferric ammonium citrate to form a black precipitate. It is significant that S paratyphi A, which produce an A/A TSI reaction and do not produce hydrogen sulfide, may be discarded as non-Salmonella Enterobacteriaceae.
The LIA system detects lysine decarboxylation, deamination, and the production of hydrogen sulfide. The hydrogen sulfide-producing bacteria genera Morganella, Proteus, and Providencia may be differentiated from Salmonella by their ability to deaminate phenylalanine. Except for S paratyphi A, the salmonellae generate a positive reaction for the decarboxylation of lysine. Salmonella species, like Shigella species, do not produce urease and generate no reaction on CU agar. This medium is included in the three-tube set to help differentiate Salmonella species from some of the other hydrogen sulfide producers and to detect Y enterocolitica.
Isolates with an appropriate biochemical profile in the three-tube set are often serotyped and definitively identified by traditional or automated biochemical testing.
For patients with enteric fever, the percent yield from blood or bone marrow culture vs stool culture varies during the course of disease (see Clinical Findings). Clinicians must be aware of which sites render the highest yield during each phase of the disease and submit appropriate specimens for culture.
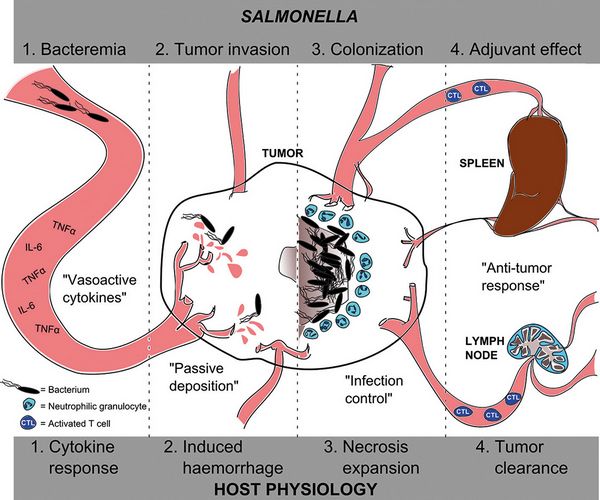
Pathogenesis
Enteric fever
The clinical course of enteric fever may be separated into three phases: an early phase that includes incubation and the onset of symptoms; the middle phase, which is the time of maximal symptomatology; and a late phase that includes diminishing symptoms, recovery, and possible carriage.
The incubation phase begins after ingestion of S typhi and usually lasts between 10 and 14 days. The incubation time, however, is variable and to a certain extent is inversely proportional to the size of the inoculum. Normal stomach acid functions as a physiologic barrier to infection, and ~ 105 organisms are required to survive gastric passage. A smaller inoculum may cause disease in patients with achlorhydria or decreased gastric acid production.
The next phase of the disease is characterized by bacterial invasion of the mucosa. The salmonellae adhere to the lumenal surface of the enterocytes, particularly specialized enterocytes, termed M cells, which overlie the Peyer’s patches. The low number of organisms present in the stool at this stage of disease explains the common occurrence of negative stool cultures.
After adhesion, the enterocyte cell membrane becomes ruffled, and there are cytoskeletal alterations. The bacteria are then internalized by endocytosis and transmigrate through the enterocyte. They exit the basilar aspect of the cell through the basement membrane and are free in the lamina propria. The organisms are phagocytosed by mononuclear phagocytes in Peyer’s patches and/or are drained by terminal lacteals to regional lymph nodes. This is followed by lymphatic and hematogenous dissemination of the bacteria to organs with fixed tissue histiocytes, such as the liver, spleen, and bone marrow. The salmonellae are able to alter the environment within macrophages and survive phagocytosis. This intracellular location also protects the bacteria from phagocytosis by polymorphonuclear leukocytes, to which they are susceptible, and to aminoglycoside antibiotics, which have poor intracellular penetration. Another virulence factor that these organisms possess is a capsule that has antiphagocytic properties and protects them from complement and antibody-mediated killing.
Bacteria, which involve the liver, may be subsequently passed into the bile. These organisms thrive in bile and may colonize the gallbladder, especially if gallstones are present. A bacterial enterohepatic circulation occurs wherein bacteria that have been shed into the bile pass into the small bowel and again adhere to and invade the small intestinal mucosa.
Salmonella gastroenteritis
Although the pathogenic mechanisms by which S typhi causes enteric fever have been well documented, the precise pathophysiology of Salmonella gastroenteritis has yet to be ascertained. The salmonellae that survive food processing and gastric acidity probably adhere to the apical portion of enterocytes by specific pili. Salmonella species may release an enterotoxin similar to the LT enterotoxin of the ETEC or the enterotoxin of V cholerae. Alternatively, these organisms may cause changes in arachidonic acid metabolites and subsequent alterations in cytosolic second messengers other than cyclic AMP. It is known that the invasion of enterocytes by salmonellae causes the production of interleukin-8, a potent neutrophil chemotactic factor. Diarrhea may in part result from disruption of the epithelium through the influx of neutrophils and release of their toxic contents.
Salmonella species survive poorly at low pHs and are killed rapidly by stomach acid. Unlike Shigella species, a substantial number of salmonellae are required to successfully cross the gastric acid barrier and cause disease. Any decrease in gastric acidity increases the likelihood of Salmonella survival. Anyone, such as persons that have had gastric surgery, with hypo- or achlorhydria are at increased risk for salmonellosis. Undercooked foods that are contaminated with salmonellae buffer gastric acid and thereby facilitate the passage of bacteria into the small intestine. Neonates and infants that may be relatively hypochlorhydric are at increased risk for infection. Persons with an impaired immune response are also at risk for nontyphoidal salmonellosis.




