This section focuses on the clinical findings, diagnosis, and treatment of pneumococcal pneumonia.
Clinical Findings
Signs and Symptoms
The so-called classic presentation of pneumococcal pneumonia consists of an abrupt onset of a shaking chill followed shortly after by fever and production of rusty sputum (Box 2). This classic presentation, however, is not the most common. Typically, patients present because of a change in preexisting symptoms. Many have had several days of a viral upper respiratory infection marked by coryza, sore throat, and nonproductive cough, or they have chronic pulmonary disease with its attendant persistent productive cough. In these patients, the development of pneumonia is heralded by the onset of fever (which can be as high as 40 °C), chills, sweats, malaise, dyspnea, and a change in the nature of the cough. Cough may either turn productive in those without prior production or increase in volume and change color in those with prior production. Less common symptoms include pleuritic chest pain and — for reasons that are poorly understood — nausea, vomiting, and diarrhea. Some patients, particularly the elderly, will present with merely an alteration in mental status. Thus, the very common entity of pneumococcal pneumonia must be entertained for a wide variety of clinical presentations.
On physical examination, persons with pneumococcal pneumonia are usually markedly ill appearing and may be cyanotic. Altered vital signs such as elevated temperature, tachycardia, and tachypnea (> 22 breaths/min) are common but, as noted above, can be absent in the elderly. In fact, in the elderly, hypothermia may be present. With the exception of the appearance of oral herpes lesions, the majority of the physical findings relate to the lungs. Dullness to percussion, increased tactile fremitus, bronchophony, whispered pectoriloquy, and egophony are sometimes present as clues to underlying consolidation, but often only rales are heard. It must be remembered, however, that even the presence of rales in an otherwise normal individual must be considered an abnormal finding and prompt further radiographic consideration of pneumonia. Conditions associated with pneumonia, meningitis (eg, nuchal rigidity), and endocarditis (eg, murmur) should also be routinely evaluated.
Laboratory Findings
An elevated leukocyte count, often with early forms (left-shifted), is common. However, in certain patient populations (eg, alcohol abusers and persons with HIV infection), the absence of a high leukocyte count does not have sufficient negative predictive value to exclude pneumococcal disease. In acutely ill patients, a low serum bicarbonate concentration and an anion gap may be seen. This should prompt arterial blood gas determination to document the presence and extent of acidemia. Although determination is not necessarily indicated in all patients presenting with suspected pneumonia, an elevated bilirubin level and lactate dehydrogenase are prevalent. Pulse oximetry on room air should be performed in all patients. Individuals with low pulse oximetry readings and for whom acid-base status is unsettled should have arterial blood gas measurements.
Two sets of blood cultures should be performed on all patients with suspected pneumonia in that this may be the only way (aside from pleural fluid culture) to diagnose definitively the etiologic agent. Nevertheless, the majority of patients with pneumococcal pneumonia are not bacteremic. Hence, particular attention must be paid to the adequate collection and processing of expectorated sputum. Although S pneumoniae can be a colonist, its growth in sputum culture in a patient with clinically diagnosed pneumonia is usually satisfactory proof of pneumococcal pneumonia. The sensitivity of culture, however, is often solely dependent on the rigor practiced by microbiology staff in the identification and subculturing of a-hemolytic colonies. Findings on Gram stain of the sputum can also be helpful but require careful interpretation. The presence of characteristic gram-positive lancet-shaped diplococci accompanied by an abundance of leukocytes (> 25 per low [100×]-power field) and a paucity of epithelial cells (< 10 per low-power field) on Gram stain suggests pneumococcal pneumonia, but the absence of this Gram stain pattern does not exclude pneumococcal disease. Although there are increasing regulations regarding clinician-prepared Gram stains, clinicians should routinely review stains that are prepared by microbiology staff.
Imaging
The sine qua non of pneumococcal pneumonia is the presence of an infiltrate on chest radiography. The clinical diagnosis of pneumonia has to be seriously questioned if, after 24 h of observation and volume repletion, a patient has not yet developed an infiltrate. A variety of radiographic findings can be observed. Lobar or segmental consolidation is classic but is less common than subsegmental involvement. Multiple subsegmental consolidation may be seen, and, occasionally, multilobar consolidation may be present. Pleural effusion is the other common finding, and the failure of a patient to improve necessitates prompt investigation of this fluid for the presence of empyema. Lung abscesses are rare, and their presence suggests serotype-3 infection. More commonly, the presence of an abscess suggests preexisting cavitary disease or coinfection with other abscess-producing organisms.
Differential Diagnosis
In patients presenting with community-acquired pneumonia (ie, acute pulmonary infection in a patient who has not been hospitalized nor has resided in a long-term-care facility in the 14 days prior to the onset of symptoms), a number of agents must be considered along with S pneumoniae in the differential diagnosis. H influenzae, Branhamella (Moraxella) catarrhalis, Chlamydia pneumoniae, and Mycoplasma pneumoniae are the most common agents, but, in certain populations, Legionella spp., Klebsiella pneumoniae, Staphylococcus aureus, Escherichia coli, Chlamydia psittaci, Coxiella burnetti, Mycobacterium tuberculosis, Coccidioides immitis, Histoplasma capsulatum, Blastomyces dermatitidis, Cryptococcus neoformans, and several respiratory viruses (eg, influenza virus, adenovirus, parainfluenza virus, and hantavirus) must also be considered. In immunocompromised hosts, the differential diagnosis expands to include a variety of other opportunistic pathogens.
A number of studies have attempted to develop algorithms that can distinguish the causative organism on clinical grounds, but none has provided sufficient predictive value upon which to base pathogen-directed empiric treatment decisions. Hence, a broad differential must be considered upon initial presentation, and definitive diagnosis can be made only with the appropriate microbiologic testing.
Complications
Bacteremia, progressive respiratory failure, and hemodynamic instability (ie, septic shock) are the most severe complications of pneumococcal pneumonia. As noted above, patients with either anatomic or functional asplenia are at particularly high risk for sepsis. Spread of infection via either contiguous extension or hematogenous routes constitutes the basis of extrapulmonary complications.
Empyema deserves special attention because it both is common and has severe manifestations if unrecognized. Empyema, which can occur either from hematogenous or contiguous spread, is defined by pleural fluid containing frank pus, a positive Gram stain or positive culture, or a pH of = 7.1. Untreated, it can result in persistent fever and may be the focus for further spread of infection. Rarely, rupture through the chest wall (ie, empyema necessitatis) can occur. If empyema fluid is not properly drained, it may heal with residual fibrosis and result in long-term functional pulmonary defects.
Purulent pericarditis, arthritis, endocarditis, and meningitis are also possible complications.
Diagnosis
The diagnostic approach to pneumococcal pneumonia first involves correctly diagnosing the syndrome of pneumonia and second involves defining S pneumoniae as the causative agent. Whether the setting is community acquired or nosocomial, the diagnosis of pneumonia is made by chest radiography of patients with suggestive predisposing factors, symptoms, and physical-examination findings. This avoids the unnecessary costs and medication side effects that are associated with prescribing antibiotics to the large numbers of individuals who have viral upper-respiratory-tract infections and who do not have pneumonia. Although chest radiography has been dismissed by some as being cost ineffective in the outpatient setting, this ignores the incalculable costs of the subsequent development of antibiotic resistance that occurs when antibiotics are inappropriately prescribed. Thus, a chest radiograph is required for all patients in whom pneumonia is suspected.
No constellation of presenting signs or symptoms has proven to be adequately predictive of pneumonia caused by S pneumoniae. Hence, once the diagnosis of pneumonia has been established on clinical and radiographic grounds, definitive diagnosis of pneumococcal pneumonia is based on the identification of the organism in normally sterile fluid (see above and Table 1 for microbiologic identification of S pneumoniae). With the rare exception of when transthoracic biopsies are performed, normally sterile fluid means either blood or pleural fluid. As stated above, detection of S pneumoniae in culture of expectorated sputum, although not entirely specific, is sufficient for a probable diagnosis of pneumococcal pneumonia and evidence enough for specific pathogen-directed therapy. The unambiguous sighting of gram-positive diplococci on sputum Gram stain without growth in culture is the least definitive evidence but may be sufficient if other pathogens are excluded and if the patient has an epidemiologic profile consistent with pneumococcal disease.
Obtaining both blood and sputum for culture is the only way to specifically diagnose pneumococcal pneumonia, but there is debate whether to perform these procedures at all, particularly in the outpatient setting. It has been argued that broad-spectrum empiric antibiotics are sufficiently effective in most patients and that specific identification of the pathogen is not required. Until a definitive trial addresses this issue and accounts, by modeling, for the far-reaching effects of broad-spectrum antibiotic use, it is the author’s opinion that, when practical to perform, all patients should receive both blood and sputum cultures.
Obtaining cultures can benefit both the individual patient and society. For individuals, determining the specific causative agent allows for altering from empiric broad-spectrum therapy to definitive treatment with an antibiotic that is usually less toxic, expensive, and disruptive to normal flora. In patients who are not responding to initial empiric therapy, a pretreatment culture may be the only opportunity to identify the causative agent and assess its antibiotic resistance patterns. Likewise, the absence of S aureus or gram-negative species in well-collected pretreatment sputum specimens essentially excludes these as pathogens and obviates the need to cover them when reconsidering the antibiotic regimen. For society, in addition to the cost savings derived from cheaper and less toxic antibiotic choices, the benefits of specific pathogen detection include the diminution of antibiotic resistance (and its associated costs) and the epidemiologic surveillance for pathogens such as drug-resistant S pneumoniae and Legionella spp. Knowledge of the prevalence of these pathogens in the community is essential for health care providers as they make empiric treatment decisions for subsequent patients who present with pneumonia.
Treatment
The approach to treatment of any of the syndromes caused by S pneumoniae must be considered in two parts — empiric and definitive therapy. Empiric therapy is prescribed when a patient presents with a clinical syndrome (eg, pneumonia) and, as is often the case, the causative agent has not yet been identified. Empiric therapy must cover all the epidemiologically likely agents. Definitive treatment is used once S pneumoniae has been identified as the causative agent.
On presentation with a clinical syndrome compatible with pneumonia, most patients are treated empirically with broad-spectrum antibiotics (see site). Assuming that a patient is responsive to an empiric regimen that covers S pneumoniae, a switch to definitive therapy depends on the confidence that the clinician and microbiology laboratory have that S pneumoniae is the sole causative agent. As noted above, growth of S pneumoniae in normally sterile body fluids like blood or pleural fluid is definitive proof of pneumococcal disease. In these instances, if other copathogens have been adequately excluded, a switch to definitive therapy is indicated.
Growth of S pneumoniae in a culture of expectorated sputum offers suggestive but not definitive proof because some persons may have pneumococcal colonization without pneumococcal disease. The isolated appearance of gram-positive lancet-shaped diplococci on sputum Gram stain (without culture growth) is again suggestive but is also the least definitive. Switching to definitive therapy in these latter two patient groups is a matter of clinical judgment and depends on several factors, including the epidemiologic likelihood of S pneumoniae compared to other pathogens, microbiologic exclusion of other pathogens, patient tolerance of empiric therapy, and cost.
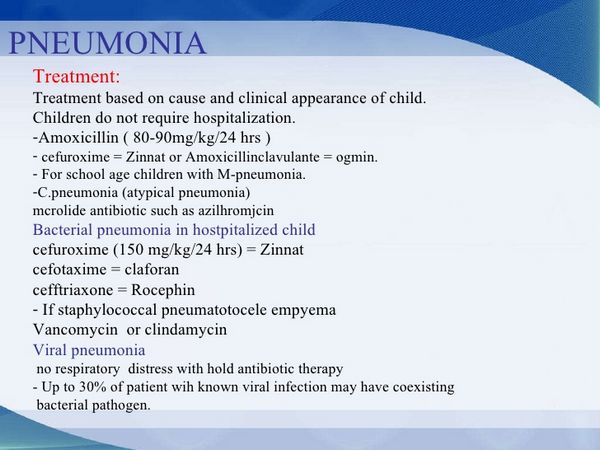
In the past, definitive therapy of pneumococcal pneumonia routinely consisted of penicillin because S pneumoniae was uniformly susceptible. In fact, antimicrobial susceptibility was not routinely tested. This has changed markedly in the past decade. Full susceptibility to penicillin is defined as a minimal inhibitory concentration (MIC) of = 0.06 ug/mL. A recent 30-center survey in the United States found that 14% of isolates had intermediate-level susceptibility (MIC = 0.1-1.0 ug/mL), and 9.5% had high-level resistance (MIC = 2.0 ug/mL). Furthermore, resistance to other antibiotics has also been increasing and is associated with penicillin resistance.
Because of the emergence of resistance, all pneumococcal isolates, including those from expectorated sputum, must undergo antimicrobial susceptibility testing. The choice of definitive therapy must be guided by these results (Box 3). Fully susceptible isolates may be treated with parenteral or oral penicillin, depending on the condition of the patient and gastrointestinal function. Fortunately, isolates demonstrating intermediate-level penicillin resistance can still be treated with parenteral penicillin. Because of its excellent bioavailability, amoxicillin is recommended for definitive oral therapy of intermediately resistant strains. Although some highly resistant isolates may also respond to parenteral penicillin or oral amoxicillin, clinical experience in this area is lacking. Hence, agents should be used for which in vitro susceptibility has been shown (eg, ceftriaxone disodium; cefotaxime sodium; a fluoroquinolone such as sparfloxacin or levofloxacin; or vancomycin).
When only a characteristic Gram stain serves as evidence of pneumococcal infection, such isolates should be considered at least intermediately resistant for purposes of definitive therapy unless no such resistance has been reported in the area. Whether these isolates should be considered highly resistant (thus necessitating choices other than parenteral penicillin or oral amoxicillin) again depends on the known prevalence of high-level resistance in the community and whether the empiric regimen to which the patient is responding would be expected to cover isolates with high-level penicillin resistance. If the regimen would not be expected to cover high-level penicillin-resistant isolates and if the patient is nonetheless responding, high-level resistance is unlikely.
Adequate duration of therapy for pneumococcal pneumonia is not known precisely, but patients should be treated for at least 5 days after they become afebrile.



