M leprae is the etiologic agent of Hansen’s Disease or leprosy.
Although not a common problem in the United States, it is in other parts of the world. With the advent of effective antimicrobial agents, the number of cases of leprosy worldwide has fallen from 12 million in 1982 to 6 million in 1991. It remains a significant problem, however, because the incidence of new cases has not yet declined, and much of the affected population lives in areas where effective medical treatment is difficult to obtain.
Leprosy is endemic in Asia, Africa, Latin America, and the Pacific. In the United States, Canada, and Europe, there are virtually no cases of leprosy except those that are imported from areas where leprosy is endemic. Risk factors for acquisition of leprosy in endemic areas include poverty and rural residence.
However, even in endemic areas, the distribution of leprosy can vary greatly, sometimes with significant differences in incidence of leprosy in adjacent villages. In North America, armadillo contact has been reported as a risk factor for acquisition.
Other risk factors that have been reported in certain populations are the human leukocyte antigens HLA-DR3 (with the tuberculoid or paucibacillary form of disease) and HLA-MTI (with the lepromatous or multibacillary form of disease). Interestingly, the proportions of the lepromatous and tuberculoid types of leprosy (Box 3) vary geographically; in Mexico, 90% are lepromatous, whereas, in India and Africa, 90% are tuberculoid.
Clinical Findings
Signs and Symptoms
The manifestations of leprosy involve the skin, upper respiratory system, peripheral nerves, and, in men, testes (Table 3). The peripheral neuropathy that is seen in leprosy results in impaired sensation of fine touch, temperature, and pain, whereas proprioception and vibratory sensation are intact. Such loss of sensation leads to recurrent trauma and ulceration in the extremities. For example, loss of sensation in the feet can lead to chronic nonhealing ulcers, especially at the metatarsal heads. Large nerve trunks may also be affected. A common nerve trunk that is affected in leprosy is the ulnar nerve at the elbow, which results in clawing of the fourth and fifth digits of the hand, dorsal interosseus muscle atrophy, and loss of sensation in the hand along the ulnar nerve distribution.
The lepromatous or multibacillary form of leprosy is characterized by symmetric skin nodules, plaques, and thickened dermis. Usually, the ear lobes and extremities are affected. Diffuse lepromatosis is seen usually in patients from Mexico, who show areas of diffuse dermal infiltration and no focal lesions. Untreated, lepromatous leprosy results in a high level of continuous bacteremia. Peripheral neuropathy is symmetric and generalized. There is a characteristic deformity associated with this type of leprosy, “saddle-nose deformity,” which occurs because of infiltration of the upper respiratory system and nasal cartilage.
Other upper respiratory system effects include chronic nasal congestion and epistaxis. The tuberculoid, or paucibacillary, form of leprosy is characterized by one or few hypopigmented macules, which are anesthetic and variable in size. These macules have distinct and elevated borders. Peripheral neuropathy in this form of leprosy is usually asymmetric and affects large nerves. Neural leprosy is characterized by functional impairment of large nerve trunks without skin lesions. The upper respiratory system is not involved.
Laboratory Findings
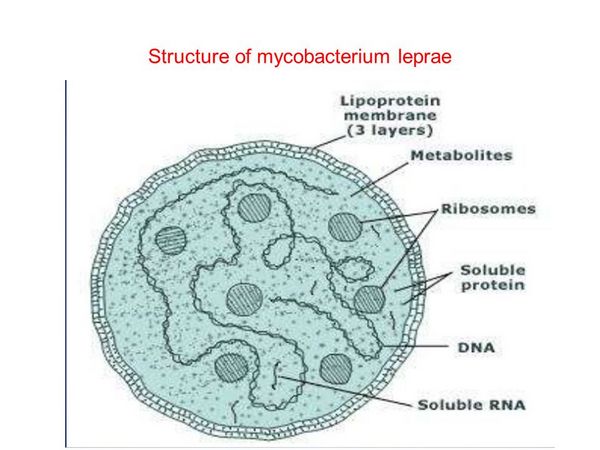
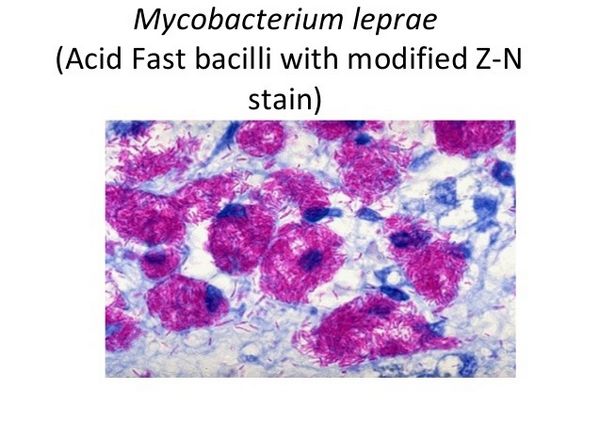
M leprae is an acid-fast, Gram-stain-variable bacillus. Its size varies from 1 to 8 um long by 0.3 to 0.5 um wide. It cannot be distinguished morphologically from other mycobacteria. M leprae’s distinguishing characteristics include loss of acid fastness by pyridine extraction, presence of dopa-oxidase activity, and a doubling time of 12 days in the mouse footpad. It is an obligate intracellular parasite but can remain viable outside its natural hosts, i.e. humans and the nine-banded armadillo, for several days.
Doubling time of the bacillus is very slow, but, by the time of diagnosis in a lepromatous patient, the number of bacilli present, 1015, is enormous, greater than any human bacterial infectious agent. M leprae has a predilection for cooler areas of the body because it grows best at temperatures under 37 °C, hence its characteristic effects on extremities, the nose, and the pinna of the ears.
Complications
Leprosy patients may develop Lepra type 1 reaction (downgrading and reversal reactions), Lepra type 2 reaction (erythema nodosum leprosum), or a reaction called Lucio’s reaction. Lepra type 1 reactions usually occur in borderline leprosy patients, before therapy (downgrading reaction) or after initiation of therapy (reversal reaction).
The reaction consists of inflammation within previous skin lesions, new multiple-satellite maculopapular skin lesions, neuritis, and low-grade fever. Irreversible nerve damage can occur unless therapy with corticosteroids is started promptly.
The recommended treatment is prednisone, 40-60 mg daily, tapered over 2-3 months. Lepra type 2 reactions affect nearly half of lepromatous patients, usually within 2 years of instituting antimicrobial therapy. Painful papules on the extensor surface of extremities, neuritis, fever, uveitis, lymphadenitis, orchitis, and glomerulonephritis can occur.
Treatment of erythema nodosum leprosum requires a short course of corticosteroids. Lucio’s reaction is seen in patients with diffuse lepromatosis and consists of shallow recurrent ulcerations on the lower extremities. Occasionally, the lesions can be generalized, and, in that case, Lucio’s reaction can be fatal.




