Essentials of Diagnosis
- Key symptoms and signs: abrupt onset of high fever, headache, myalgias, chills 8-9 days after tick bite; rash (36% of human monocytic ehrlichiosis [HME] patients; only 2% of human granulocytic ehrlichiosis [HGE] patients); central nervous system involvement (20-25% of patients).
- Predisposing factors: tick and rural exposure (April through September).
- Presentation: most present as flu-like illness.
- Key laboratory features: thrombocytopenia, leukopenia, and elevated liver transaminases.
- Diagnosis: confirmed by a fourfold or greater rise in titers with an IFA.
General Considerations
Human ehrlichiosis was first recognized in the United States in 1986 as a life threatening tick-borne illness similar to Rocky Mountain spotted fever (RMSF), but with a much lower incidence of rash.
Epidemiology
Ehrlichiosis is not a reportable disease, so its true incidence is unknown. The majority of cases of HME have been reported from the south, central, and southeastern United States. Cases have also been reported from Western Europe, Scandinavia, and Africa.
In contrast, most cases of HGE have been reported from the upper midwestern and northeastern United States. This difference in disease geography reflects the distinct habitats of the respective tick vectors.
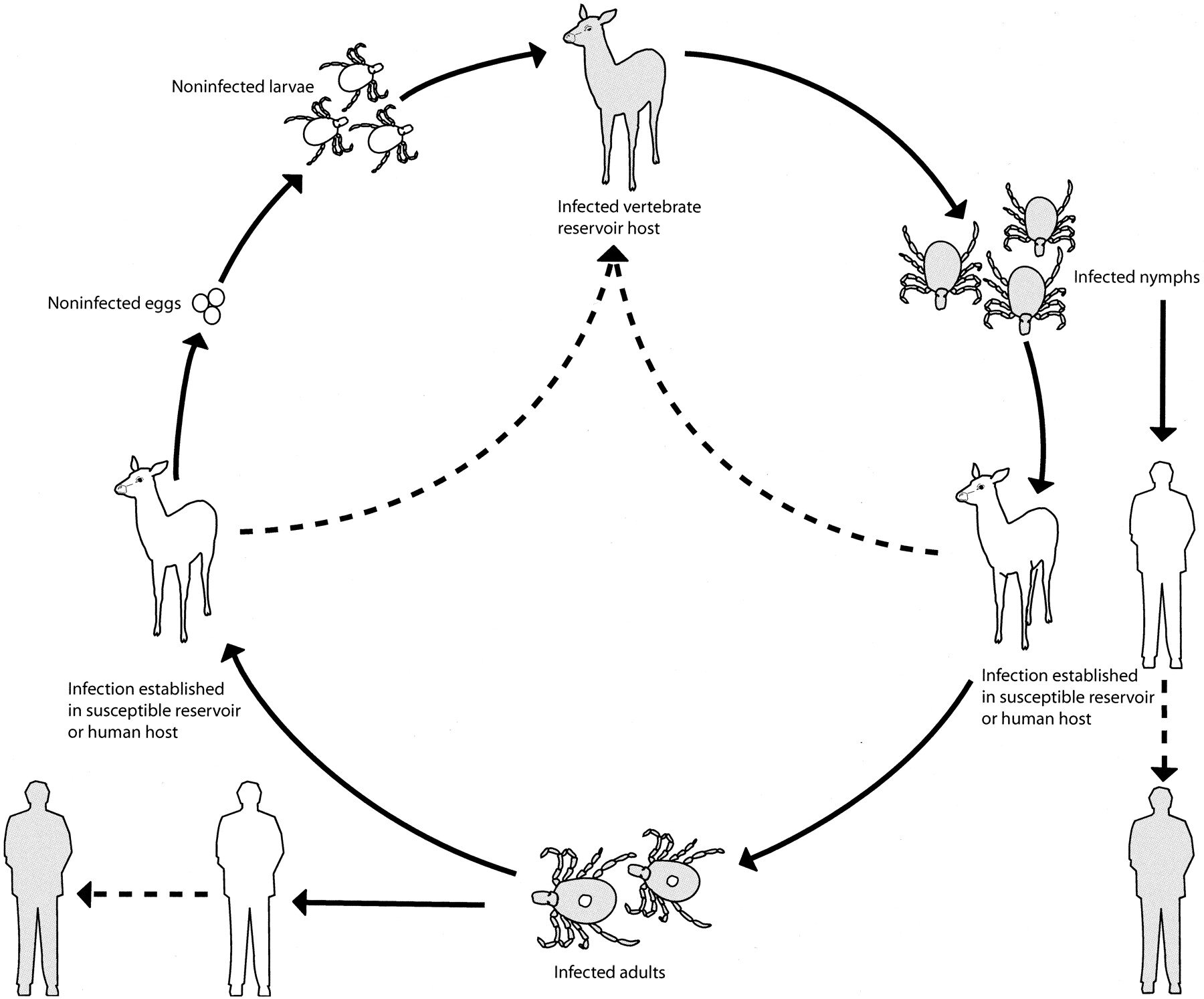
Amblyoma americanum transmits HME and is found throughout the southeastern and south central United States. The white-tailed deer serves as a reservoir for the etiologic agent, E chaffeensis. The Ixodes species are the tick vectors of HGE (as well as Lyme disease and babesiosis), and they are found in the Northeast, upper Midwest, and Pacific Coast regions of the United States. The white-tailed deer is the primary host for adult Ixodes ticks, but small rodents — especially the white-footed mouse — play an important role in the deer-tick-rodent cycle and transmission of the agent of HGE to humans. Of infected humans, 80-100% report tick exposure within the 10 days preceding the onset of illness.
The median age of patients reported with HME is 44 years; 75% are male. The median age of HGE cases is 60 years, with a similar sex ratio. Cases of HME occur from April through December, but HGE cases are seen throughout the year, owing to the seasonal feeding patterns of the different tick vectors in different regions of the United States.
Microbiology
There are two forms of human ehrlichiosis in North America, HME and HGE; their clinical features are indistinguishable. The causative agent of HME, Ehrlichia chaffeensis, was the first member of this genus to be detected in humans in the United States; HGE was first recognized in 1994, and it is caused by an organism closely related to Ehrlichia equi and Ehrlichia phagocytophila. Ehrlichia sennetsu is the only other known pathogen for humans in this genus, but it has been reported only in Western Japan.
Canine ehrlichiosis is caused by Ehrlichia canis and Ehrlichia ewingii, which infect macrophages and granulocytes, respectively. E phagocytophila is a pathogen of ruminants in Europe and exhibits tropism for neutrophils. E equi causes both equine and canine disease.
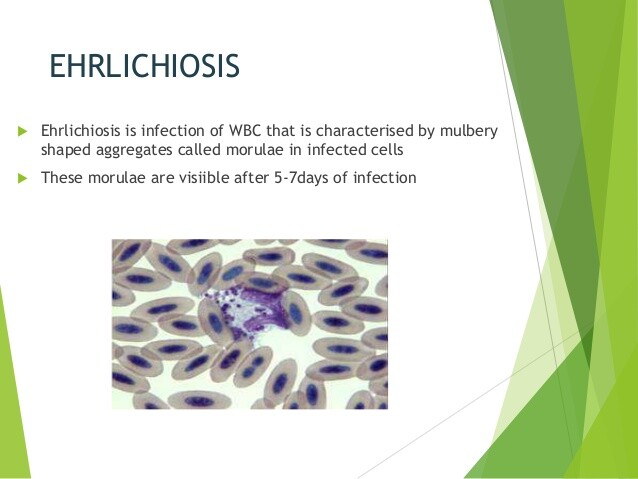
C. Pathogenesis. Ehrlichia species are small, obligate intracellular organisms whose life cycle includes the formation of intraleukocytic inclusions, termed morulae. Replication and development of organisms within morulae lead to rupture and release of elementary bodies into the circulatory system and subsequent infection of other leukocytes. Recent data indicate that the granulocytic Ehrlichia species may enhance their survival within neutrophils by down-regulating expression of one component of the host NADPH oxidase enzyme complex, a critical feature of the oxidative burst machinery.
Clinical Findings
Signs and Symptoms
The symptoms and signs of human ehrlichiosis are nondescript, thereby making the diagnosis difficult. The median incubation period is 8-9 days after tick bite, with a range of 0-34 days. The clinical presentation characteristically includes an abrupt onset of high fever (>39°C), headache, myalgias, and shaking chills (Box 4). Other symptoms include malaise, confusion, rigors, sweats, nausea, vomiting, and abdominal pain. Rash is reported in 36% of patients with HME but only 2% of those with HGE.
Laboratory Findings
The laboratory findings of human ehrlichiosis are relatively consistent and include thrombocytopenia in 72-92% of patients, elevated liver transaminase levels in the serum in 85-90% of patients, and leukopenia in 50-75% of patients. These laboratory findings are most pronounced at the end of the first week of illness. Morulae are rarely seen on acute-phase peripheral blood smears of patients with HME but are seen more commonly in the peripheral blood smears of patients with HGE. Detection of morulae in peripheral blood smears remains an insensitive and time-consuming task, and, when found, morulae have been reported most often by clinical hematology laboratory technicians.
Differential Diagnosis
Diseases in the differential diagnosis include ehrlichiosis (see Diagnosis section), typhus, Q fever, tularemia, early Lyme disease, viral hepatitis, leptospirosis, influenza, and Colorado tick fever. Coinfection with other tick-borne agents must always be considered.
Complications
Central nervous system involvement is reported in 20-25% of patients, with symptoms ranging from confusion through coma. Other severe complications may occur, such as disseminated intravascular coagulation, respiratory failure, renal insufficiency, and opportunistic infections secondary to neutropenia. Most elderly patients with HME who have been reported have also been hospitalized. Case fatality rates are 2-5% for HME and 7-10% for HGE. However, it is also now clear from seroprevalence studies that many patients have mild or asymptomatic infection.
Diagnosis
It is necessary and important to consider the diagnosis of ehrlichiosis based only on epidemiological and clinical features, to facilitate administration of empiric therapy, because there is no widely available rapid diagnostic test other than detection of visible morulae. Ehrlichiosis should be considered in any febrile patient in an endemic region with exposure to ticks within the preceding 3 weeks.
The diagnosis becomes more likely if thrombocytopenia, elevated hepatic transaminases, or leukopenia is present. There are no absolute clinical criteria that distinguish ehrlichiosis from RMSF, although patients with ehrlichiosis are less likely to have a rash and more likely to have leukopenia and elevated hepatic transaminases. In addition to finding intraleukocytic morulae, serology offers a reliable but retrospective method for diagnosing Ehrlichia infection.
Acute and convalescent titers are required. IFA detection assays are available for both HME and HGE. Although E chaffeensis and the agent of HGE can be cultured, this method of detection and PCR-based assays are not widely available.
Treatment
Doxycycline is the agent of choice for both HGE and HME (Box 5). The clinical response is rapid, usually within 24-48 h. Chloramphenicol has been used in younger children to prevent teeth discoloration secondary to tetracyclines; however, in vitro and in vivo failures have been described. Enhanced mortality and morbidity from ehrlichiosis are associated with delayed administration of appropriate therapy, advanced age, and a higher percentage of infected leukocytes. Although most patients respond to therapy within several days, most experts advocate a 14-day course of therapy, in part to treat more adequately for possible concomitant Borrelia burgdorferi infection.
Prevention & Control
Preventive measures against tick exposure should be used to prevent transmission of ehrlichiosis. If tick exposure occurs, thorough whole-body examination for and prompt removal of attached ticks are important for prevention of transmission.