Essentials of Diagnosis
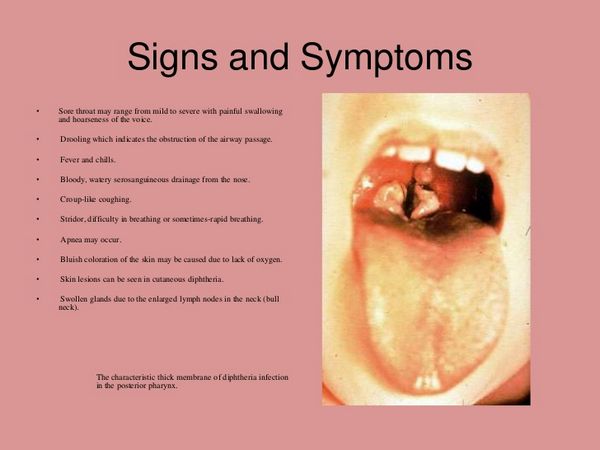
- Mildly painful tonsillitis/pharyngitis with associated membrane, cervical adenopathy, and signs of systemic toxicity; “bull neck” appearance.
- Hoarseness and stridor.
- Palatal paralysis.
General Considerations
Epidemiology
Humans are the only known natural hosts for C diphtheriae, the organism that causes diphtheria. This organism is usually spread via upper respiratory tract droplets, but it can also be spread by direct contact with skin lesions. Transmission appears to be more common when people are living indoors in crowded conditions. Disease is transmitted by those incubating the disease, those convalescing from infection, and also healthy carriers. The organism itself can survive for = 6 months in dust, which may also serve as the vehicle for transmission. Immunization against diphtheria toxin prevents the serious complications of disease, by blocking the ability of the toxin to enter cells and also by reducing colonization of the nasopharynx by toxin-producing strains. Diphtheria is a rare disease in the United States; however, this disease can easily spread in populations that lack adequate levels of antitoxin immunity, as dramatically demonstrated in the former Soviet Union in the early 1990s.
Microbiology
C diphtheriae is a gram-positive rod with club-shaped swellings at each end. Most strains produce an exotoxin, diphtheria toxin, which is encoded by a gene carried by a lysogenic bacteriophage and is responsible for the disease.
Pathogenesis
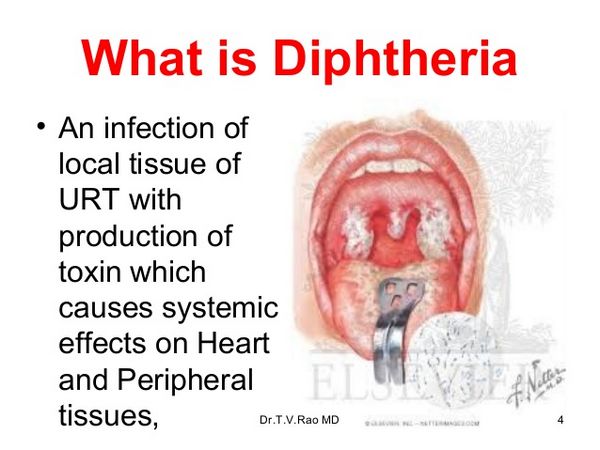
C diphtheriae attaches to the mucosal surfaces of the nasopharynx. There it remains in the superficial layers of the mucosa. When iron concentrations are low, lysogenic diphtheria bacilli produce high concentrations of diphtheria toxin. The conversion of nontoxigenic, nonlysogenic C diphtheriae to toxin-producing strains can occur within the nasopharynx after bacterial infection with the beta-corynephage. Diphtheria toxin is composed of A and B fragments. The B fragment is recognized by a specific host cell membrane receptor resulting in endocytosis of the entire molecule. Once the toxin is inside the endosome, acidification results in a conformational change of the B fragment. A membrane channel is formed, allowing passage of fragment A into the host cell cytoplasm. Fragment A blocks protein synthesis by cleaving NAD and covalently attaching ADP-ribose to the essential host protein, elongation factor-2. ADP-ribosylation interferes with the ability of elongation factor-2 to add amino acids to a peptide chain, blocking protein synthesis. Its effects are seen throughout the body but are most prominent in the heart and kidney and on nerves. Local cytotoxic effects lead to production of the characteristic “pseudomembrane.” Anti-toxin antibody can neutralize toxin adsorbed to cells, but, once the toxin penetrates, its toxic affects are irreversible.
Clinical Findings
Respiratory Diphtheria
The incubation period for respiratory diphtheria is generally 2-4 days, but it can last = 7 days. Initial symptoms include a low-grade fever. Sore throat and malaise are the most common manifestations of pharyngeal diphtheria. Unvaccinated patients tend to have more severe disease. The development of cell necrosis, secondary to the exotoxin, is commensurate with the presence of the characteristic membrane. Initially the membrane is white and smooth, but later it becomes gray with patches of green and black necrosis. As the membrane spreads, it can interfere with airflow. Involvement of the posterior pharynx is often accompanied by cervical adenopathy and swelling, giving rise to a “bull neck” appearance. With extensive disease there is increased release of exotoxin, resulting in myocardial and neurologic complications, thereby increasing the mortality associated with this disease.
Cutaneous Diphtheria
Cutaneous diphtheria usually begins with pustules that progress to ulcer formation with a gray-brown membrane at the base. Commonly, C diphtheriae will superinfect existing skin lesions such as insect bites, ecthyma, and impetigo. Cutaneous infections induce high levels of antitoxin antibody that prevent progression to systemic disease; therefore, the infections tend to be indolent and are not usually associated with signs of intoxication. Cutaneous infection poses a greater risk of environmental contamination and transmission to others than does pharyngeal infection.
Cardiac Disease
Myocarditis with clinically-significant cardiac dysfunction is observed in 10-20% of patients with pharyngeal disease. The likelihood and severity of myocarditis are correlated with the extent and severity of respiratory tract compromise. ST segment and T-wave changes and first-degree block are found by electrocardiography in less severe disease, whereas left bundle branch block and atrioventricular block are associated with high mortality. In severe cases, patients usually sustain permanent injury to the myocardium.
Neurologic Disease
Neurologic complications occur in ~ 10% of respiratory cases and are predicted by the severity of respiratory tract involvement. Symptoms and signs develop 10-28 days after the respiratory complaints and reflect both cranial nerve involvement and a peripheral neuropathy that can lead to complete paralysis. These complications are usually reversible.
Diagnosis
Prompt recognition and treatment of respiratory diphtheria are critical for preventing complications and mortality. A dark pharyngeal membrane that cannot be removed without bleeding, systemic toxicity, neurologic abnormalities such as 9th and 10th cranial nerve deficits, and/or electrocardiograph changes should alert the clinician to the possibility of diphtheria. The microbiology laboratory should be notified about the possibility of diphtheria, because special media, such as Loeffler’s or tellurite selective media, must be used to prevent overgrowth of normal flora.
Treatment
All patients should be hospitalized and isolated. Rapid institution of antitoxin is critical because it is most effective if given within 4 days of the onset of illness (Box 8). Hyperimmune antiserum produced in horses has been used for > 100 years. The dose of antitoxin is adjusted to the severity of disease. Sensitivity of the patient to horse protein must be assessed (see recommendations in Box 8). An initial scratch test may be performed on the volar forearm with a 1:100 dilution. If negative, this should be followed by an intracutaneous injection of 0.02 mL of a 1:1000 dilution of antitoxin in saline. No additional benefit is provided by repeated doses. Antibiotics should be initiated as soon as possible to kill organisms, stop toxin production, and eliminate the carrier state. Erythromycin for 2 weeks is the treatment of choice and should be given intravenously until the patient is able to handle oral medications. Procaine penicillin for 2 weeks is an alternative. Other measures include airway and cardiac support. If diphtheria is suspected, the patient should be isolated until two cultures from the affected site are negative. Cultures should be taken from all persons who have been in close contact with a diphtheria patient, to determine whether they are pharyngeal carriers. All carriers need to be treated with erythromycin or penicillin for 14 days.
Prevention
Children 6 weeks to 7 years of age should be immunized with three injections of vaccine containing formalin-inactivated diphtheria toxin (Box 9). Susceptibility to diphtheria correlates inversely with serum levels of anti-toxin antibody. Because these levels wane, adults should receive booster vaccinations every 10 years.



