General Considerations
Chlamydia trachomatis, Chlamydia psittaci, and Chlamydia pneumoniae are among the most prevalent microbial pathogens in humans worldwide. C trachomatis is responsible for a variety of sexually transmitted disease (STD) syndromes in both sexes. In addition, certain serotypes of C trachomatis are responsible for trachoma, the most common infectious cause of blindness in humans. C psittaci is a zoonotic pathogen associated with atypical pneumonia. C pneumoniae infects approximately one-half of the world’s human population and is a cause of upper and lower respiratory tract disease. It has also been associated with atherosclerotic cardiovascular disease.
Epidemiology
In the United States, genital infections by C trachomatis serovars D through K occur frequently among sexually active adolescents and young adults. These serovars are also important perinatal pathogens. In 1998, > 600,000 cases were reported in the United States (237 per 100,000 population), making it the most common notifiable infectious disease in this country. Asymptomatic infection is rather common in both women and men.
Prevalence rates vary according to the geographic locale and the specific populations. The prevalence of urethral infection among young men is < 10% for those seen in general medical settings, between 10% and 15% for asymptomatic soldiers undergoing routine medical care, and > 10% for heterosexual men seen in STD clinics. The prevalence of C trachomatis genital infection among women is 5% for asymptomatic college students, > 10% for women monitored in family-planning clinics, and > 20% for women seen in STD clinics.
Chlamydial genital infections are found at a higher rate among women who use oral contraceptives or have cervical ectopy. It is estimated that 5-25% of pregnant women in the United States carry C trachomatis in their cervix. Of the neonates who get infected during birth, ~ 25% develop inclusion conjunctivitis, and 10% develop pneumonia.
Lymphogranuloma venereum (caused by serovars L1, L2, and L3) is a rare disease in the United States. The vast majority of cases are transmitted sexually, but transmission by nonsexual routes has been documented.
C trachomatis serovars A, B, Ba, and C cause trachoma, one the most common causes of preventable blindness in the world. These serovars are usually transmitted from person to person (most often involving a child) via hands and fomites. Endemic areas include Asia, the Middle East, sub-Saharan Africa, and northern Africa.
C psittaci is usually transmitted to humans by contact with birds or from occupational exposure in avian-processing plants or poultry farms. Essentially all common birds and several wild species are capable of carrying the organism and shedding it while remaining healthy. Only brief exposure to an area where an infected bird has been present is necessary for transmission of C psittaci. Rarely, the bite of a bird transmits the disease.
C pneumoniae was established as a human respiratory pathogen in 1983, and it is now associated with 6-12% of cases of community-acquired pneumonia. Approximately 50% of persons worldwide have been infected by early adulthood. Outbreaks of C pneumoniae respiratory disease have been described especially in military recruits but also in the general population; the highest rates of C pneumoniae pneumonia are found among the elderly. There is no seasonal predominance. Exchange of respiratory secretions by aerosol route or by hand appears to be the primary mode of transmission of C pneumoniae. In more recent years, this organism has been associated with atherosclerosis and coronary artery disease.
Microbiology
Members of the genus Chlamydia are small, obligate intracellular prokaryotic organisms. They contain DNA, RNA, ribosomes, and a discrete cell envelope. The envelope lacks peptidoglycan between the inner and outer membranes, which explains why cell wall-active antibiotics have no role in the treatment of chlamydial infections.
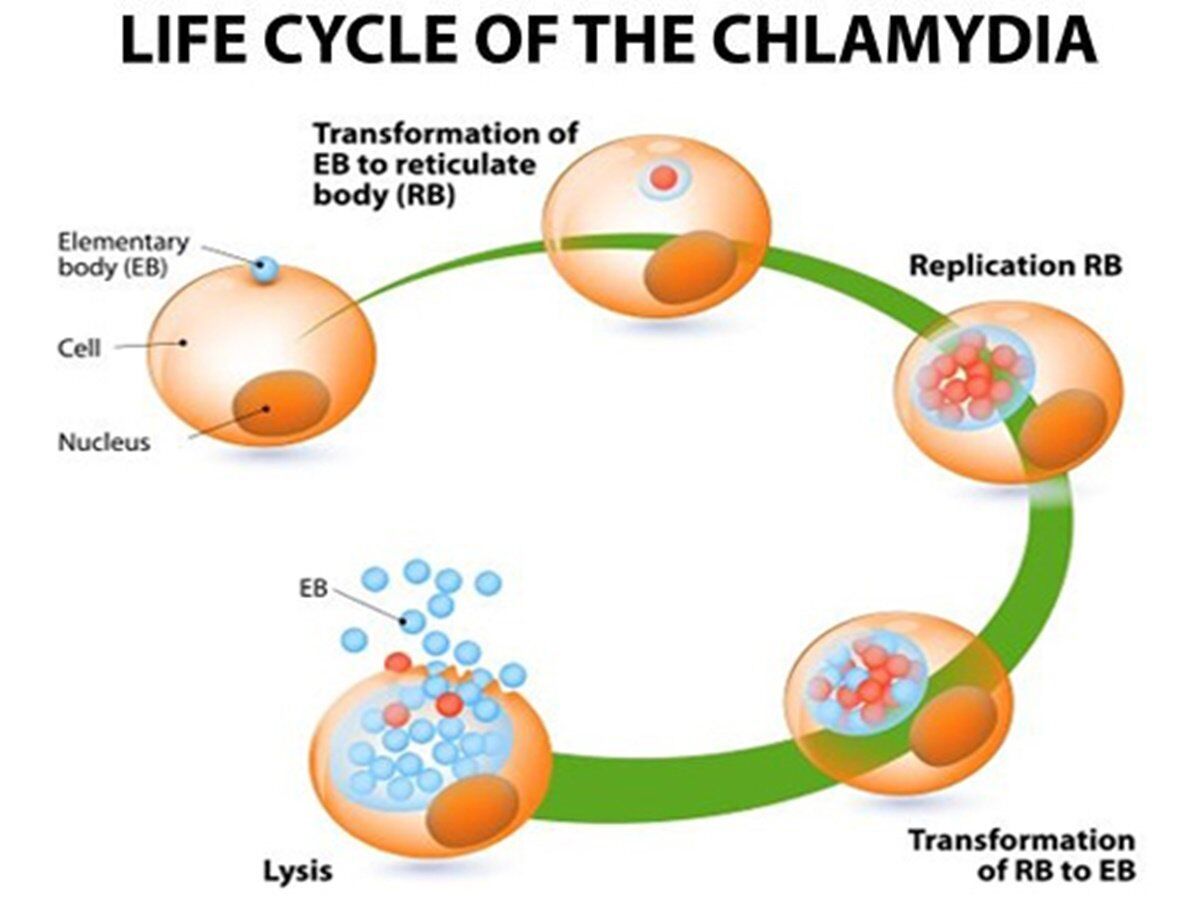
During their unique life cycle, Chlamydia species are observed in two distinct forms: the extracellular elementary body and the intracellular reticulate body. The elementary body is responsible for person-to-person transmission. It attaches to, and is engulfed by mammalian target cells.
Within the phagosome, the elementary bodies reorganize and develop into reticulate bodies, which are adapted for intracellular survival and multiplication. After multiple rounds of replication by binary fission, the reticulate bodies condense and form elementary bodies.
The elementary bodies eventually rupture the host cell to continue the cycle by infecting other contiguous cells. The complete genome sequences of C trachomatis and C pneumoniae reveal a large number of genes that are most similar to versions found in eukaryotes, emphasizing the coevolution of pathogen and host. Despite their distant relationship with the gram-negative bacilli, both Chlamydia species contain genes that appear to encode a “type III” secretion system typically associated with invasiveness and other virulence attributes.
Members of the genus Chlamydia share a common heat-stable lipopolysaccharide antigen and specific cell envelope protein antigens which facilitate their classification into a number of serotypes. Protein antigenic and gene sequence variability of the major outer-membrane protein have led to the identification of at least 20 sero- and sequence types of C trachomatis. The vast majority of the serotypes can be assigned to one of three major groups: (1) serovar group A, B, Ba, and C, which is associated with trachoma; (2) serovar group D, E, F, G, H, I, J, and K, which is associated with sexually transmitted and perinatally acquired infections; and (3) serovar group L1, L2, and L3, which is associated with lymphogranuloma venereum and hemorrhagic proctocolitis.
Pathogenesis
Chlamydia species rupture mammalian cells after unregulated replication of elementary bodies; pathology results from this cell lysis, as well as damage caused by recruited inflammatory cells and cytokine mediators. Repeated or persistent exposure is believed to elicit more intense host inflammatory responses, some of which may be directed at chlamydial heat shock proteins. A crucial and common pathologic endpoint of chlamydial infection is scarring of mucous membranes, especially of the conjunctiva (trachoma) and female upper genital tract (resulting in infertility).
The elementary body of C trachomatis attaches to host epithelial cells by using heparan sulfate as a bridging ligand and later infects mononuclear leukocytes in lymph nodes via the local lymphatic draining system. Immunity against C trachomatis appears to protect only partially against reinfection.
C psittaci is acquired through inhalation of respiratory secretions or aerosolized droppings of infected birds; it spreads via the bloodstream and eventually reaches reticuloendothelial cells of the spleen and liver. Pneumonitis is characterized by edema, necrosis, erythrocytes, and a chronic inflammatory cellular infiltrate.
Little is known regarding the pathogenesis of C pneumoniae. It appears that C pneumoniae has a less rigid cell wall than that in other chlamydial species.
Diagnosis
Chlamydial infections require laboratory studies for a definitive diagnosis. Available laboratory techniques include cytology, culture, serology, and demonstration of chlamydial antigens or nucleic acid sequences.
Treatment
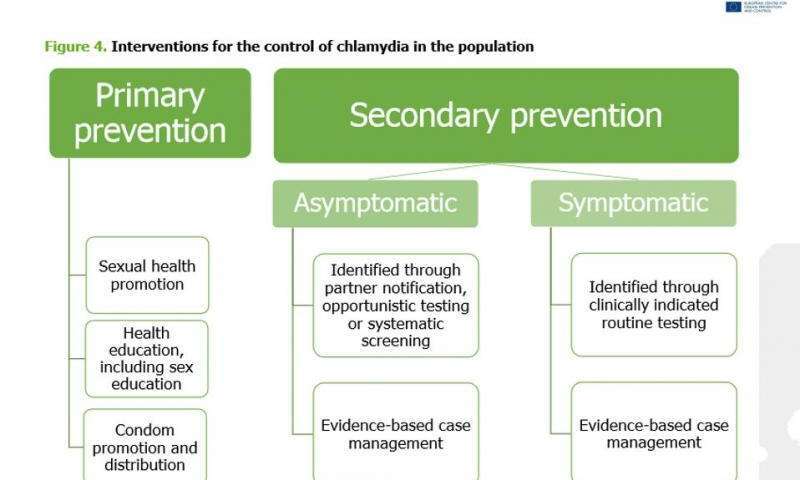
Antimicrobial agents such as the tetracyclines, certain macrolides, and some fluoroquinolones are highly active against Chlamydia infections. Clinically relevant resistance to these antibiotics has not been observed. All sex partners of patients with sexually transmitted chlamydial infections should be referred for evaluation and treatment.
C Trachomatis Infections
C Psittaci Infections
C PNEUMONIAE INFECTIONS
Essentials of Diagnosis
- Hoarseness may accompany atypical pneumonia.
- Positive C pneumoniae-specific microimmunofluorescence serologies.
- Positive complement fixation titers (not species specific)
- Isolation and PCR techniques available in research laboratories only.
Clinical Findings
Upper- and lower-respiratory-tract infections including sinusitis, pharyngitis, bronchitis, and pneumonia have been associated with C pneumoniae infection (Box 7). Bronchitis and pneumonia are the most common syndromes seen in clinical practice.
The incubation period for C pneumoniae pneumonia has been estimated at ~ 21 days. Patients usually present with a history of fever and prominent upper respiratory symptoms followed by sore throat and nonproductive cough. Physical exam can be entirely normal or can reveal mild to moderate respiratory distress, usually with minimal auscultatory changes.
The leukocyte count is usually normal or slightly elevated. Chest radiography may reveal minimal segmental infiltrates. Despite this more common picture, C pneumoniae pneumonia can be life threatening in patients older than 65 years. More recent serologic and anatomic data suggest that chronic C pneumoniae infections may play a role in atherosclerosis and in the progression of coronary artery disease. The clinical relevance of this information is not clear at this time.
Diagnosis
Serological methods are commonly used for the diagnosis of C pneumoniae infections. They are rarely helpful in the acute setting, and they are mostly used for surveillance purposes. Complement fixation methods do not differentiate among infections caused by C trachomatis, C psittaci, and C pneumoniae. Microimmunofluorescence methods detect C pneumoniae-specific antibodies and are the approaches most commonly used in clinical practice. Acute and convalescent sera samples obtained = 3-4 weeks apart should be analyzed in parallel. Isolation of this organism and PCR-based methods are not routinely performed outside research laboratories.
Treatment
C pneumoniae infection should be treated with a tetracycline, a macrolide, or a fluoroquinolone (Box 8).
The recommended treatment regimens for C pneumoniae infections in children include erythromycin (50 mg/kg/d for 10-14 days) or clarithromycin (15 mg/kg/d for 10 days). Some patients may require retreatment.
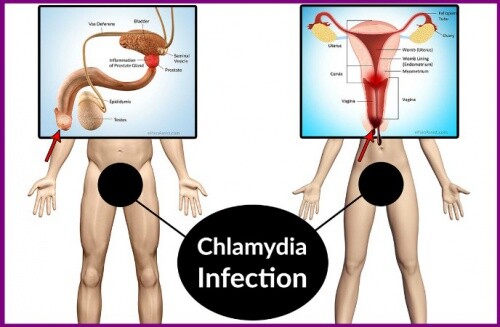
BOX 1. C trachomatis Infections
Women
Men
Children
More Common
- Mucopurulent cervicitis
- Acute salpingitis
- Endometritis
- Bartholinitis
- Acute urethral syndrome
- Nongonococcal urethritis
- Postgonococcal urethritis
- Epididymitis
- Inclusion conjunctivitis in infants
- Pneumonia in infants
Less Common
- Perihepatitis
- Proctitis
- Conjunctivitis
- Reiter’s syndrome
- Proctitis
- Conjunctivitis
- Reiter’s syndrome
- Otitis media
- C trachomatis in genital secretions should raise the suspicion of sexual abuse
These syndromes are also categorized under the syndrome PID.
BOX 2. Treatment of C trachomatis Genital Infections (Serovars D-K)1,2
First Choice
- Azithromycin, 1 g orally in a single dose
OR
- Doxycycline, 100 mg orally twice a day for 7 d
- Erythromycin base, 500 mg orally four times a day for 7 d
Second Choice
OR
- Erythromycin ethylsuccinate, 800 mg orally three times a day for 7 d
OR
- Ofloxacin, 300 mg orally twice a day for 7 d
Pediatric Considerations
- Erythromycin, 40 mg/kg/d orally, divided into 4 doses/day, for 14 days
OR
- Doxycycline (children = 8 years old), 4 mg/kg/d orally in 2 divided doses for 14 days
- Sex partners should be evaluated, tested, and treated if they had sexual contact with the patient during the 60 days preceding onset of symptoms. The most recent partner should be treated even if time of the last sexual contact was >60 days preceding onset of symptoms.
- Coinfection with C trachomatis often occurs among patients who have gonococcal infection.
- Children with genital C trachomatis infection should raise the possibility of sexual abuse.
BOX 3. Treatment of Lymphogranuloma Venereum (Serovars L1, L2, and L3)1
First Choice
- Doxycycline, 100 mg orally twice a day for 21 days
Second Choice
- Erythromycin base, 500 mg orally four times a day for 21 days
Sex partners should be evaluated, tested, and treated if they had sexual contact with the patient during the 30 days preceding onset of symptoms
BOX 4. Treatment of Other C trachomatis Infections
Infant Pneumonia and Ocular Infections
- Erythromycin, 50 mg/kg/d in four divided doses for 10-14 d
Adult Inclusion Conjunctivitis
- Doxycycline, 100 mg orally twice a day for 1-3 weeks
OR
- Erythromycin, 250 mg four times a day orally for 1-3 weeks
Topical treatment is not recommended.
BOX 5. C psittaci Infections in Adults and Children
More Common
- Community-acquired pneumonia with nonproductive cough, fever, and headache (exposure to birds)
Less Common
- Mononucleosis-like syndrome with pharyngitis, hepatosplenomegaly, and lymphadenopathy
- Typhoidal form with fever, bradycardia, malaise, and splenomegaly
- Endocarditis, myocarditis, and pericarditis
BOX 6. Treatment of C psittaci Infections
First Choice
- Tetracycline, 500 mg four times a day for 10-21 days
OR
- Doxycycline 100 mg orally twice a day for 10-21 days
Second Choice
- Erythromycin base, 500 mg orally four times a day for 7 d (erythromycin may be less efficacious in severe cases)
Pediatric Considerations
- Erythromycin, 50 mg/kg/d orally up to 2 g/d for 7-10 days
OR
- Tetracycline (children = 8 years old), 500 mg every 6 h for 7-10 days
BOX 7. C pneumoniae Infections in Adults and Children
More Common
- Community-acquired pneumonia
- Possible association with atherosclerotic cardiovascular disease
- Possible association with adult-onset asthma and acute exacerbations among adults with asthma
Less Common
- Bronchitis
- Pharyngitis
- Sinusitis
- Endocarditis
- Lumbosacral meningoradiculitis
- Erythema nodosum
- Encephalitis
BOX 8. Treatment of C pneumoniae Infections
First Choice
- Azithromycin, 500 mg/d for 10 d
OR
- Clarithromycin, 500 mg twice a day for 10-14 days
OR
- Levofloxacin, 500 mg every day for 10-14 days
Second Choice
- Tetracycline, 500 mg four times a day for 10-14 days
OR
- Doxycycline, 100 mg orally twice a day for 10 to 14 days
Pediatric Considerations
- Erythromycin, 50 mg/kg/d orally for 10-14 days
OR
- Clarithromycin, 15 mg/kg/d orally for 10 days
Articles:
https://en.wikipedia.org/wiki/Chlamydia_infection
https://www.healthline.com/health/std/chlamydia
https://www.avert.org/sex-stis/sexually-transmitted-infections/chlamydia
https://www.plannedparenthood.org/learn/stds-hiv-safer-sex/chlamydia