Signs and Symptoms
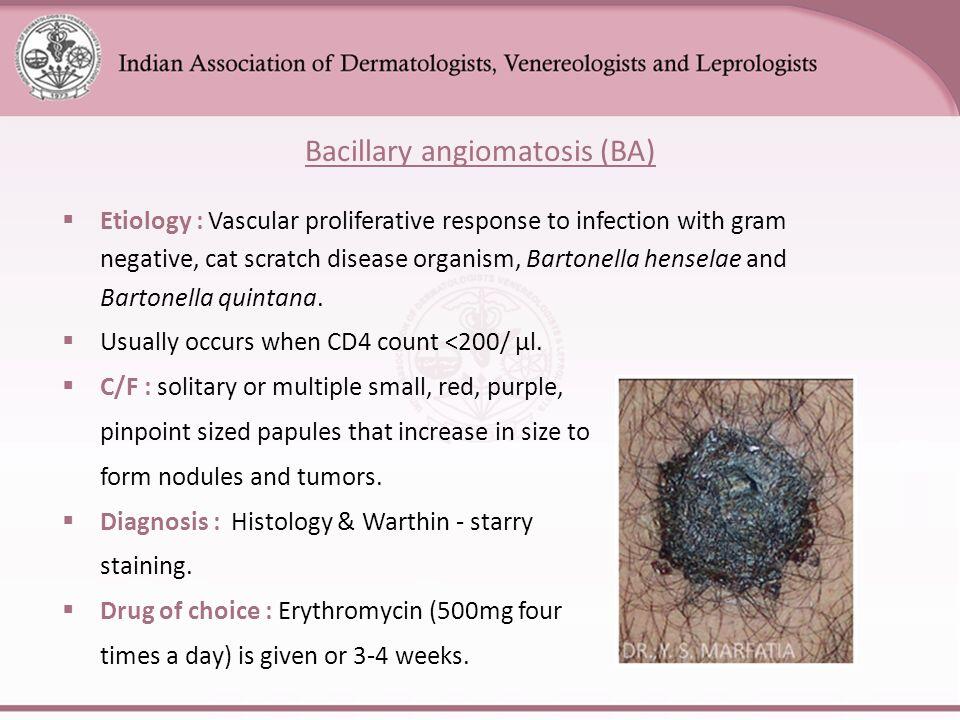
The most common manifestation of bacillary angiomatosis is a dermal lesion (Table 1). Three types of lesions are seen: cutaneous papules, subcutaneous nodules, and hyperpigmented plaques, in decreasing order of frequency.
Papules are usually red-purple in color and range in size from a few millimeters to several centimeters, often surrounded by a collarette of scale. They vary in number, are often friable and bleed easily, are occasionally tender, and may resolve spontaneously even in immunosuppressed patients. These lesions are easily removed by curettage. Slight hyperpigmentation and induration may persist.
Subcutaneous nodules or lobules are the second most common presentation and may vary markedly in size and number. Underlying cortical bone erosion may be associated with these nodules. There is often minimal epidermal change or hyperpigmentation, but, infrequently, the overlying skin changes may resemble cellulitis. While cutaneous disease is associated with both Bartonella species, subcutaneous and bony disease is associated almost exclusively with B quintana. Regional lymph node enlargement may be present; these nodules may be tender but rarely ulcerate or bleed.
Less common are indurated hyperpigmented plaques, which are often oval in shape and several centimeters in diameter. These hyperkeratotic plaques are typically found on the extremities.
Liver and spleen involvement by Bartonella spp. with or without cutaneous disease is frequently associated with B henselae in the immunocompromised host. The spectrum of liver and spleen pathology varies from a nonspecific necrotizing inflammatory reaction to bacillary peliosis. Bacillary peliosis is characterized by cystic blood-filled spaces throughout the tissue parenchyma. Since the advent of AIDS, peliosis, a previously rare entity associated with chronic debilitating illnesses (such as tuberculosis and malignancy) and anabolic steroid use, has increased. Bacillary peliosis is fatal in rare cases.
Bacillary angiomatosis may also involve the mucus membranes of the mouth, nose, larynx, bronchi, conjunctiva, and anus; the lung and pleura; bone; and the central nervous system.
Bacillary angiomatosis should strongly be considered in any HIV-infected patient with skin and lytic bone lesions. B. Laboratory Findings. Patients with bacillary peliosis may have elevated serum alkaline phosphatase levels, as well as thrombocytopenia or pancytopenia. C. Imaging. Computed tomographic scans of patients with bacillary peliosis often show multiple hypodense areas that are enhanced following the use of contrast agents, scattered throughout an enlarged liver, and ascites. D. Differential Diagnosis.
The differential diagnosis of a bacillary angiomatosis skin lesion includes Kaposi’s sarcoma, pyogenic granuloma, simple hemangioma, angiokeratoma, and verruga peruana (in the appropriate geographic region). Lesions of bacillary angiomatosis and Kaposi’s sarcoma cannot be distinguished by gross appearance.
Links
https://en.wikipedia.org/wiki/Bacillary_angiomatosis http://emedicine.medscape.com/article/212737-overview http://www.pathologyoutlines.com/topic/skintumornonmelanocyticbacillaryangiomatosis.html