Because there is evidence that pools of latently infected CD4+ T-cells are established during the earliest stages of acute HIV infection and persist even in patients who have received potent multiple-drug antiretroviral regimens that suppress viral load to undetectable levels for prolonged periods, eradication of HIV infection with currently available antiretroviral regimens is not a realistic goal.
Therefore, the primary goals of antiretroviral therapy in the management of HIV infection are maximal and durable suppression of HIV viral load (as measured by plasma HIV-1 RNA levels), restoration and/or preservation of immunologic function, improvement of quality of life, and reduction of HIV-related morbidity and mortality. These goals can best be met by use of potent multiple-drug antiretroviral regimens that decrease viral replication, limit the potential for selection of resistant HIV strains, and delay disease progression. In addition, the benefits of antiretroviral therapy can be maximized by rational sequencing of drugs and preservation of future treatment options, use of strategies that maximize compliance with the antiretroviral regimens, and use of resistance testing in selected clinical settings.
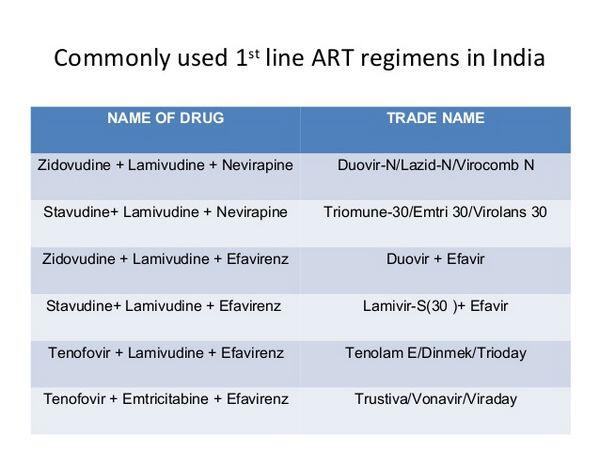
Antiretroviral regimens that were considered treatments of choice for the initial management of HIV infection in the past (e.g., monotherapy with zidovudine, didanosine, or stavudine; 2-drug regimens that include only NRTIs) are now considered suboptimal regimens since clinical benefits associated with such therapy (i.e., delay in disease progression, decrease in incidence of opportunistic infections, improved survival) are not sustained over the long term.
Potent antiretroviral regimens that include a minimum of 3 drugs currently are recommended for the management of HIV infection in most patients. These regimens often are referred to as highly active antiretroviral therapy (HAART) to differentiate them from the less potent regimens previously used for the management of HIV infection.
A major advantage of currently recommended potent multiple-drug antiretroviral regimens over previously recommended regimens is the potential for additive or synergistic effects against HIV and possible prevention or delay in emergence of resistant strains of the organism. There is clear evidence that antiretroviral regimens that only partially suppress viral replication allow more rapid selection of resistant variants that contribute to therapeutic failure.
Another advantage of potent multiple-drug therapy that includes drugs that have different mechanisms of action is that such therapy may provide antiretroviral activity in a broader range of viral reservoirs, including CD4+ T-cells, monocytes/macrophages, CNS tissue, and lymphoid tissue, and at different stages of cellular activity. Potential disadvantages of these regimens include the possibility of additive toxicities, pharmacokinetic interactions or cross-resistance among the drugs, limited options for future regimens, increased cost, and decreased patient compliance because of the complexity of the regimens.
Experience with various antiretroviral regimens has shown that the duration of clinical benefit from any one antiretroviral regimen may be limited and that optimal antiretroviral therapy involves continuous evaluation of the patient’s response to the current regimen and appropriate modification of the regimen whenever the need for a change is indicated by increases in viral load (plasma HIV-1 RNA levels), disease progression, or drug toxicity or intolerance.
There also is growing evidence that while potent multiple-drug antiretroviral regimens may effectively decrease plasma HIV-1 RNA to undetectable levels for 2 years or longer and provide substantial benefits in terms of immunologic, virologic, and clinical responses, no antiretroviral regimen evaluated to date can suppress HIV replication completely or eliminate the virus from the body. The virus apparently continues to persist in various tissues (e.g., lymphoid tissue, latently infected resting CD4+ T-cells, CNS). Infectious HIV has been isolated from CD4+ T-cells obtained from infected individuals whose plasma HIV-1 RNA levels have been suppressed below the limits of detection for prolonged periods (2 years of more). There is evidence that discontinuance of effective antiretroviral therapy can result in rapid rebound HIV replication, antiretroviral therapy may need to be continued indefinitely.
Although structured or supervised interruption of antiretroviral therapy has been suggested in certain situations or certain patients (e.g., following early therapy of primary [acute] HIV infection, following suppressive antiretroviral therapy of established infection, as part of salvage therapy, for auto-immunization and better immune control over HIV, to allow less total time on antiretroviral therapy), experts state that data are insufficient to date regarding the benefits and risks of interrupting antiretroviral therapy and this strategy cannot be recommended at this time for use in general clinical practice and should be attempted only in the context of cohort studies or clinical trials.
Results of a study in patients with multidrug-resistant HIV and plasma HIV-1 RNA levels exceeding 5000 copies/mL indicate that structured interruption of treatment for 4 months followed by a change in the antiretroviral regimen was associated with greater disease progression and provided no immunologic or virologic benefits compared with an immediate change to a new antiretroviral regimen.
Since information on, and experience with, available multiple-drug regimens are changing rapidly, experts in the management of patients with HIV infection need to be consulted regarding the potential advantages and limitations of available therapeutic options. The choice of antiretroviral agents to include in the initial regimen used in HIV-infected individuals who are treatment naive (have not previously received antiretroviral therapy) and the most appropriate agents to use in subsequent regimens in previously treated individuals must be individualized based on virologic, immunologic, and clinical characteristics of the individual patient.
Some factors to be considered when selecting antiretrovirals to include in a multiple-drug regimen are the antiretroviral potency of the agents, availability and cost of the agents, possible presence of drug-resistant HIV variants, potential rate of development of resistance, potential pharmacokinetic interactions among the drugs and with other drugs that the patient may be receiving, and the patient’s ability to be compliant with the dosage regimens involved.
Ideally, drugs included in the regimen should have additive or synergistic antiretroviral activity and nonoverlapping toxicities, and lack the potential for pharmacokinetic interactions. If several options are available, antiretrovirals should be selected that preserve future therapeutic options if the current regimen were not to achieve the desired antiretroviral effect.
While the most appropriate antiretroviral regimen cannot be defined for each clinical scenario, guidelines for the use of antiretroviral agents in certain clinical situations have been identified by several groups, including the Panel on Clinical Practices for Treatment of HIV Infection convened by the Department of Health and Human Services (DHHS), a committee convened by the British HIV Association (BHIVA), and an international panel convened by the International AIDS Society—USA. The guidelines proposed by these and other experts are based on current knowledge regarding the pathogenesis of HIV.
Although a large number of clinical studies evaluating a wide variety of antiretroviral regimens have been published and many more are under way, some of the regimens included in these guidelines have not been evaluated in controlled clinical trials to date and are recommended based on the general principles of antiretroviral therapy and data available to date regarding safety and efficacy of the individual antiretroviral agents included in the regimens. For information on results of controlled clinical studies evaluating the safety and efficacy of currently available antiretroviral agents and experience to date regarding various antiretroviral regimens.





