Consideration should be given to altering the initial antiretroviral regimen in HIV-infected pediatric patients if there is clinical, immunologic, or virologic evidence of disease progression; if there are signs of toxicity or intolerance; or if new data become available indicating that a drug or regimen is superior to the current regimen.
Clinical events that may indicate disease progression in an HIV-infected child and warrant consideration of a change in antiretroviral therapy include progressive neurodevelopmental deterioration or growth failure (i.e., persistent, unexplained decline in weight growth velocity despite adequate nutritional support).
Progressive neurodevelopmental deterioration is defined as persistence or progression of deterioration documented on repeated testing as demonstrated by the presence of 2 or more of the following findings: impairment in brain growth, decline in cognitive function documented by psychometric testing, or clinical motor dysfunction. If there is evidence of progressive neurodevelopmental deterioration, the new antiretroviral regimen optimally should include at least one drug that has substantial CNS penetration (e.g., zidovudine or nevirapine).
While prognosis generally is poorer as the disease progresses, disease progression in a patient with stable immunologic and virologic parameters is not necessarily an indication that the antiretroviral regimen needs to be changed. For example, development of a new opportunistic infection, especially in those who were severely immunocompromised at the time antiretroviral therapy was initiated, may indicated persistence of immunologic dysfunction despite adequate antiretroviral therapy rather than a lack of response to the antiretroviral regimen.
Therefore, in pediatric patients whose disease progression is not associated with neurologic deterioration or growth failure, virologic and immunologic parameters should be considered when deciding whether to change antiretroviral therapy.
Immunologic status (i.e., CD4+ T-cell counts and percentages) is an important factor when deciding whether to change an antiretroviral regimen; however, in pediatric patients, CD4+ T-cell counts and percentages are independent predictors of disease progression and mortality.
Because the absolute CD4+ T-cell count that identifies a specific level of immunosuppression changes with age, changes in CD4+ percentage may be a better marker for immunologic status and disease progression in children.
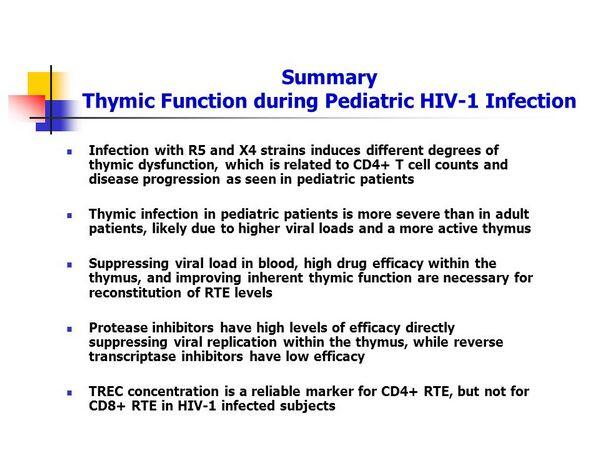
Before any alterations are made in the antiretroviral regimen based on apparent changes in CD4+ T-cell counts or percentages, these values should be confirmed by at least 2 separate measurements made at least one week apart. Immunologic indications of disease progression in an HIV-infected child that may warrant alteration of the antiretroviral regimen include a change in the child’s HIV immune classification, rapid and substantial decrease in absolute CD4+ T-cell count (e.g., greater than 30% decrease in less than 6 months), or a persistent decline of 5% or more in CD4+ T-cell percentage in those with baseline values less than 15%.
Limited information is available regarding expected changes in plasma HIV-1 RNA levels in infants and children following initiation of antiretroviral therapy. There is evidence that plasma HIV-1 RNA level criteria used to assess the response to antiretroviral therapy in adults may be appropriate for adolescents and possibly also could be used for perinatally infected children older than 3 years of age; however, adult criteria should not be used to assess the response to antiretroviral therapy in other pediatric patients. It has been suggested that consideration be given to altering the antiretroviral regimen if, after 8-12 weeks of therapy, there is a less than tenfold (1.0 log) decrease in plasma HIV-1 RNA level from baseline in children receiving a 3-drug regimen that includes 2 NRTIs and an HIV protease inhibitor or a less than fivefold (0. log) decrease in those receiving a less potent regimen (e.g., a 2-drug regimen that includes NRTIs without an HIV protease inhibitor).
Other situations that may indicate a need for a change in the regimen include detectable plasma HIV-1 RNA levels after 4-6 months of antiretroviral therapy; repeated detection of plasma HIV-1 RNA in children who initially had undetectable levels in response to therapy; or a reproducible increase in plasma HIV-1 RNA levels in a child who had a viral response but still had low levels of detectable plasma HIV-1 RNA. The most recent guidelines for use of antiretroviral agents in pediatric infection should be consulted for further information regarding virologic or immunologic considerations for altering an antiretroviral regimen in pediatric patients.
Because limited information is available regarding the pharmacokinetics, efficacy, adverse effects profile, and most appropriate dosage of some antiretroviral agents in children, consultation with a specialist who has extensive experience in the care of HIV-infected children is strongly advised when a change in antiretroviral therapy is being considered. If a change in the antiretroviral regimen is indicated because of toxicity or intolerance, new agents should be selected that have a different toxicity and adverse effects profile In the event of drug intolerance, changing a single drug in the multidrug regimen and, in certain circumstances, reduction in dosage are possible options.
However, antiretroviral dosage should only be reduced to the lower end of the therapeutic range for those drugs for which an effective dosing range is known, and adequacy of antiretroviral activity should be confirmed by monitoring plasma HIV-1 RNA levels. If a change in the antiretroviral regimen is indicated by lack of response, disease progression, or drug failure, the possibility that noncompliance with the regimen may have contributed to treatment failure should be considered. If the patient has been adherent to the prescribed drug regimen, resistance to the antiretroviral agents can be assumed and the potential for cross-resistance between antiretrovirals should be considered when selecting a new regimen. The value of in vitro genotypic or phenotypic resistance assays in guiding treatment of HIV-infected children has not been established.
Whenever a change in the antiretroviral regimen is being considered, all drugs being taken by the patient should be reviewed for possible drug interactions. If the antiretroviral regimen is altered, at least 2 drugs in the prior regimen should be changed; changing only a single drug or adding a single drug to a failing regimen is considered suboptimal. Ideally, the new regimen should include at least 3 new drugs. If a change in an antiretroviral regimen is being made because of disease progression in a patient with advanced disease, the patient’s quality of life should be considered.
Each time a change in the antiretroviral regimen is made, especially when the regimen includes HIV protease inhibitors, the importance of adhering to the prescribed regimen should be discussed with the caregivers of the infected child.

