Potential Severity
A chronic debilitating infection that can cause severe disfiguring complications by blocking lymphatic drainage.
Prevalence, Epidemiology, and Life Cycle
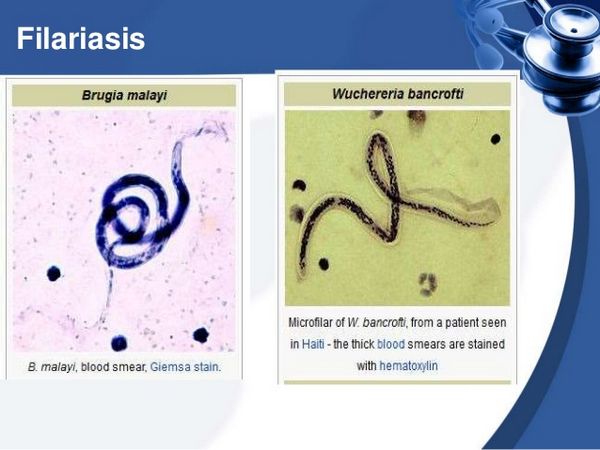
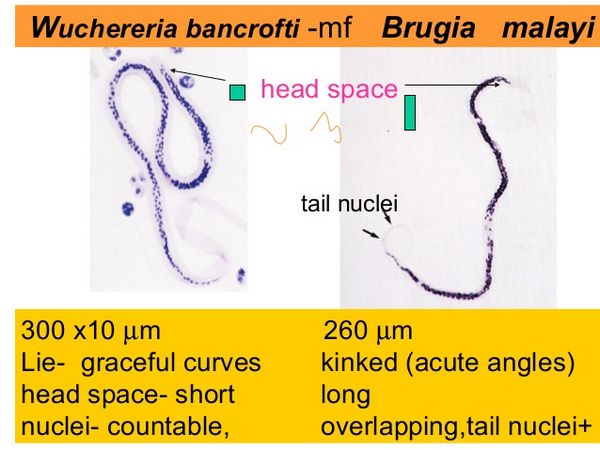
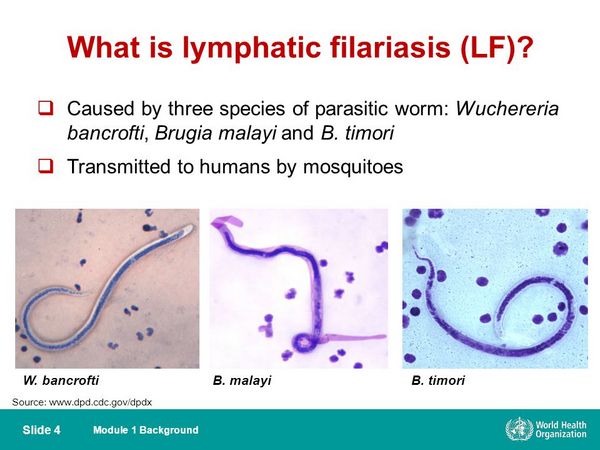
Microfilaria is less common than many parasites, being estimated to infect approximately 120 million people. Several strains of worm can cause this disease. Wuchereria bancrofii is found throughout the tropics, and Brugia malayi is restricted to the southern regions of Asia. A third strain, Brugia timori is found only in Indonesia. Infectious larvae are transmitted by the bite of a mosquito.
Larvae pass from the skin into the lymphatic system, where, over several months, they mature near the lymph nodes. Adult worms (40 to 100 mm in length) can survive in the lymphatic system for 5 to 15 years. During this period, males and females mate, daily producing an average of 10,000 microfilaria (dimensions: 200 to 300 mm in length, and 10 mm in width). The microfilaria are released into the bloodstream.
The time from initial insect bite to appearance of microfilaria in the infected human is usually 12 months. In W bancrofii, the highest concentration of microfilaria in the blood is generally found in the middle of the night, explaining why midnight blood smears are recommended for diagnosis. If a mosquito bites an infected human, the microfilaria are ingested and, over 10 to 14 days, they develop into infective larvae that can be transmitted to a new human host. The percentage of mosquitoes containing infective larvae has been estimated to be just 1% in endemic areas.
Repeated mosquito bites are therefore generally required to contract this infection, which may explain why adults — particularly men — more commonly contract this infection.
Clinical Presentation
Asymptomatic Filariasis
Many individuals have asymptomatic infection. Peripheral eosinophilia and palpable lymphadenopathy may be the only clinical manifestations. Children usually experience no symptoms, despite high numbers of microfi-laria in their blood.
Inflammatory Filariasis
Adults more commonly react with strong allergic reactions to the invasion by worms that begins approximately 1 year after exposure. Fever, chills, vomiting, headache, and malaise may be associated with lymphangitis of an extremity, orchids, epididymitis, or scrotal swelling. The affected extremity becomes hot, swollen, erythematous, and painful, mimicking cellulitis. These symptoms are associated with peripheral leukocytosis and an increased percentage of eosinophils (6% to 25%). Unlike cellulitis, which usually begins peripherally and moves up the limb, inflammatory filariasis begins centrally near the lymph nodes and extends peripherally. Attacks may occur monthly and do not respond to antibiotics. The granulo-matous response in the lymphatic tissue is thought to be a host inflammatory reaction to dying worms. Death of the worms is associated with release of the rickettsial-like bacteria Wolbachia that live in a symbiotic relationship within the adult worms.
Obstructive Filariasis
Over time, chronic inflammation leads to fibrosis and permanent obstruction of lymphatic flow. This syndrome is the result of continuous microfilaria infection. Persistent lymphatic obstruction and edema lead to marked skin thickening and deposition of collagenous material, eventually causing elephantiasis. Patients suffer with debilitating enlargement of the legs or massive enlargement of the scrotal tissue, making walking difficult. Cellulitis caused by streptococci or Staphylococcus aureus may periodically recur, requiring antibiotic treatment. Rupture of the lymphatics into the kidney or bladder can result in chyluria, and rupture into the peritoneum can cause chylous ascites.
Life Cycle of Wuchereria bancrofti and Brugia malayi
- Transmitted bythe bite of an infected mosquito.
- Repeated mosquito bites are required.
- Microfilaria live in the lymphatic system, and worms enter the bloodstream at midnight (except in the South Pacific).
- Mosquitoes are infected by biting humans.
Diagnosis and Treatment
Giemsa- or Wright-stained peripheral smears should be obtained at midnight in all cases except for those from the South Pacific. Identification of adult worms in the blood is definitive; however, in early and late disease, worms often are not seen. Antibody and antigen assays are highly sensitive and specific. An IgG4 antibody titer correlates with active disease. An ELISA for W bancrofti circulating antigen is now the diagnostic test of choice, and titers correlate with adult worm burden. A Polymerase chain reaction test for W bancrofti has been developed, but it is not widely available. Biopsy of infected lymph nodes is generally not recommended, but when performed, may reveal adult worms in addition to granuloma. Ultrasonography of dilated lymphatics in the spermatic cord have revealed motile worms. In early infection and during the inflammatory stage, peripheral eosinophilia is commonly seen.
Clinical Presentation of Filariasis
- Many people, particularly children, are asymptomatic.
- Inflammatory filariasis is associated with periodic erythema, warmth, pain, and swelling that mimic cellulitis (associated with peripheral eosinophilia).
- Obstructive disease results in chronic limb swelling (elephantiasis) because of lymphatic fibrosis.
- Obstructive disease can lead to recurrent bacterial cellulitis.
- Rupture of lymphatics can cause chyluria or chylous ascites.
- Release of the rickettsial-like bacteria Wolbachia from the adult worms may be the major stimulus for inflammation.
Diagnosis and Treatment of Filariasis
- Midnight blood smear demonstrating worms yields a definitive diagnosis.
- In early and late disease, worms may not be seen.
- Ultrasound of dilated lymphatics may demonstrate worms.
- Peripheral eosinophilia is common.
- Enzyme-linked immunoabsorbent assay is sensitive and specific, and levels correlate with disease activity.
- Diethylcarbamazine or ivermectin plus alben-dazole is used for treatment.
Treatment can exacerbate symptoms. During the chronic stages of disease, eosinophilia is generally not present. If worms cannot be identified, the diagnosis has to be made on clinical grounds. Diethylcarbamazine in a single dose is the recommended therapy, but fails to kill adult worms.
A reduction in the level of microfilaria in the blood is usually observed. Treatment may increase inflammation and may not halt progression to fibrosis and lymphatic obstruction. Ivermectin 200 to 400 mg/kg, combined with albendazole 400 mg, is another effective regimen that may more effectively kill the adult worms.
For more severely infected patients, a 3-week course of doxycycline kills the symbiant Wolbachia, resulting in sterility of the adult worms. This treatment can be followed by diethylcarbazine or ivermectin plus albendazole.
Normally, these agents exacerbate the host’s inflammatory reaction as the microfilaria die, but doxycycline eradication of the Wolbachia eliminates this complication. Anti-inflammatory agents may be used to reduce the extent of inflammation, and elastic support stockings can be helpful in reducing moderate lymphedema.