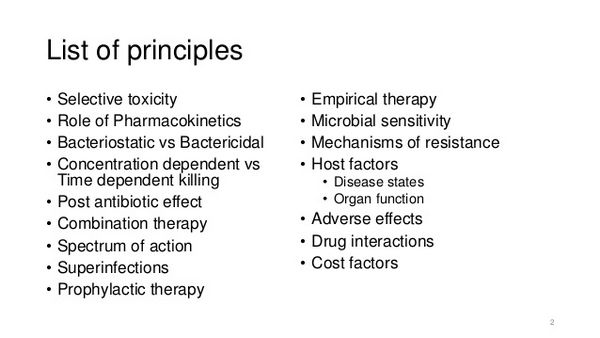
A wide variety of antimicrobial agents is available to treat established infections caused by bacteria, fungi, viruses, or parasites. This section will cover the general principles of antimicrobial therapy and will also include illustrative clinical problems to emphasize proper decision-making in using antimicrobials.
Determinants of Antimicrobial Efficacy
Measurement of antimicrobial activity in vitro
Susceptibility testing is indicated for any bacterial pathogen warranting chemotherapy. Drugs that irreversibly destroy the ability of an organism to replicate, and perhaps in the process destroy the structural integrity of the organism, are microbicidal. Drugs that reversibly impair replicating ability, with this function being restored when drug concentrations fall below critical inhibitory levels, are microbiostatic. In quantitative assays of in vitro antimicrobial activity, an organism is said to be “susceptible” to an antimicrobial when in vitro microbicidal or microbiostatic concentrations of drug are comparable to those that can be easily achieved in plasma during clinical use.
Mot quantitative assays express this property in terms of the concentrations in plasma that can be reached with standard forms of administration of drug. It is important to recognize that factors such as tissue and intracellular concentrations, as well as the activity of antibiotic metabolites, the presence or absence of concentration-dependent killing and postantibiotic effects, will also affect the in vivo activity of an antimicrobial agent.
Assays that do not correlate in vitro activity with their potential in vivo therapeutic values have been abandoned. Detailed discussions of antimicrobial sensitivity testing can be found elsewhere. Discussion of susceptibility tests will be confined to the three most commonly employed assays for aerobic bacteria: disk diffusion, E-test, and broth dilution sensitivity testing. Susceptibility testing for anaerobic bacteria, mycobacteria, fungi, and viruses is more complex and less well standardized and is usually performed by reference laboratories. The susceptibility testing of anaerobic bacteria is technically demanding-disk susceptibility testing is unreliable, and automation cannot be used.
Since there are a number of effective antibiotics to which anaerobic bacteria are predictably susceptible, it is not necessary to regularly assess the susceptibility of anaerobic bacteria to a variety of agents. It is important that susceptibility testing be performed in serious or persistent bacterial infections including bacteremia, brain abscess, and infections of the eyes, joints, and bones.
Disk sensitivity testing
Disk diffusion tests (e.g., Kirby-Bauer) developed in 1966 are the most widely used type of nonautomated susceptibility test. This method has been standardized for rapidly growing pathogens including Enterobacteriaceae, Staphylococcus, Pseudomonas, some streptococci such as S. pneumoniae, Haemophilus, and Neisseria species (National Committee for Clinical Laboratory Standards 1993). This method is not appropriate for anaerobic bacteria, slow-growing organisms, or organisms that show marked strain-to-strain variation. These assays measure the ability of drug to inhibit a microorganism’s growth by placing drug-impregnated paper disks on a “lawn” of organisms inoculated onto the surface of agar plates. With diffusion of the antibiotic through the agar, a decreasing gradient of antibiotic concentrations develop around the disk. If the antibiotic is active against the organism tested, a growth-free zone surrounds the disk.
Since a standard amount of active antibiotic and a standardized bacterial inoculum are used, the diameter of the zone of growth inhibition can be correlated directly with broth dilution assays that measure minimal inhibitory concentrations. Thus, when the diameter of the inhibitory zone is greater than a certain size, there is a correlation with a good clinical outcome, and in these cases the organism is said to be susceptible to the antimicrobial. When the zone diameter is below a defined size, then in vivo concentrations of antibiotic are not likely to inhibit the organism and it is said to be resistant.
Results are labeled intermediate sensitivity when the size of the zone indicates that antibiotic concentrations that are inhibitory to the organisms might be reached in vivo, provided that high dosages are used or that the infection is localized to an area where concentrations of antibiotic may exceed those in the blood (e.g., in the urine). The reliability of the Kirby-Bauer technique depends on adequate growth of bacteria on agar suitable for susceptibility testing, a standardized inoculum size, specific concentrations of active antibiotic in the antimicrobial disk, and standardized growth conditions. Any alteration of these specifications can invalidate the results. The Kirby-Bauer technique does not provide information on whether the drug is bactericidal or bacteriostatic.
E-test
The E-test developed by AB Biodisk is a plastic strip with an exponential antimicrobial gradient applied. The strip is applied to the surface of an agar plate in much the same manner that an antibiotic disk might be for Kirby-Bauer disk diffusion testing. The strip is marked with the concentrations of antibiotics at regular intervals along the gradient. After incubation there is an elliptical shaped zone of inhibition around the strip. The point at which the pointed end of the ellipse intersects with the strip represents the minimal inhibitory concentration of the organism. E-test strips are expensive and are usually used for specific minimal inhibitory concentration determinations and for testing organisms that do not produce reliable results by other methods. Since E-test strips are easy to use and require no instrumentation, their use has increased markedly in recent years.
Broth dilution sensitivity testing
The broth dilution technique is a widely used method to measure quantitatively the in vitro activity of an antimicrobial agent against a particular bacterial isolate (National Committee for Clinical Laboratory Standards 1994). It may be more expensive to perform (especially if done manually), and it is technically more sophisticated than disk diffusion tests.
There are very few indications for mandatory use of broth dilution testing, since information derived from disk diffusion tests is adequate in the majority of common bacterial infections. Broth dilution studies should be performed when it is critical for the clinician to prescribe antibiotics for difficult-to-treat infections.
Usually the broth dilution test is performed in microtiter plates. Each well containing specified dilutions of antibiotic is inoculated with a standardized inoculum of organisms; the plates are incubated for a sufficient time to permit the detection of growth in the control well. When determined visually, this usually requires 16 to 24 hours; however, newer instruments that measure optical density in the wells are often able to produce susceptibility testing results on the same day. The lowest concentration of antibiotic that inhibits bacterial growth is the minimal inhibitory concentration. A minimal microbicidal concentration can be determined by subculturing, onto antibiotic-free agar, material from wells that show no visual growth.
The lowest concentration of antimicrobial that prevents growth on subculture is the minimal microbicidal concentration. In the case of bacteriostatic drugs, the organism may not be killed unless exposed to suprapharmacologic concentrations of antibiotic. With most bactericidal drugs, the minimal microbicidal concentration usually is 1 or 2 dilutions (2 times) as high as the minimal inhibitory concentration. If the organism is not killed unless the antibiotic concentration is increased to 16 times the minimal inhibitory concentration, then it is tolerant to the antibiotic.
The data derived from these tests can be coupled with the knowledge of expected or measured antibiotic concentrations in vivo to predict efficacy of the antibiotic. As with the disk diffusion method, reproducibility depends on standardization of inoculum sizes and incubation conditions. These tests provide the clinician with a direct measure of antimicrobial concentrations that should inhibit microbial replication in vivo.
Unless automation is employed, measurements of antimicrobial minimal microbicidal concentrations and MBCs against a specific organism usually are reserved for patients with serious systemic infections such as endocarditis, in which antibiotic efficacy is a more critical factor than host defenses in eradicating the infection. The use of minimal microbicidal concentrations may also be necessary when disk testing is not able to adequately characterize susceptibility results.
For example, Streptococcus pneumoniae isolates may be screened for penicillin susceptibility using a disk diffusion test, but minimal microbicidal concentrations must be carried out in order to determine whether high-, intermediate-, or low-level resistance is present. Minimal inhibitory concentration testing is used to determine S. pneumoniae susceptibility to third-generation cephalosporins. Minimal inhibitory concentration testing may also be useful in evaluating causes of treatment failure when other causes are not apparent.
Other sensitivity-testing techniques
Agar dilution testing is a method for measuring antimicrobial susceptibility that lends itself to testing large numbers of microorganisms. A standardized inoculum is inoculated onto the surface of media containing relevant concentrations of antibiotics using a multitined replicator. The minimal microbicidal concentrations can then be determined from the concentration of antibiotic that inhibits visible growth of the organisms on the surface of the agar.
Results of these assays usually correlate well with broth dilution minimal microbicidal concentrations. This method is well suited to the testing of slower-growing organisms including anaerobes. It is also well suited to batch testing of bacteria, as might be necessary in comparing the activity of a newer antibiotic with commercially available agents and for performing periodic surveys for public health or other purposes.
The serum bactericidal test is another susceptibility test. It is a simple variation of the broth dilution test. It is performed in the same manner, except serial dilutions of a sample of serum from the patient are used instead of the various concentrations of antimicrobial agents. The serum is obtained from the patient during antimicrobial therapy (usually when drug concentration is at its nadir) and diluted. The tubes or wells are then inoculated with a standardized suspension of the pathogen isolated from the patient. After appropriate growth, the tubes are examined, and the serum’s inhibiting titer is determined. All samples are subsequently subcultured. The serum bactericidal titer is that dilution of serum that shows >99.9% killing of the initial inoculum.
The use of the serum bactericidal test is controversial, with concern focusing on the technology and the clinical significance of the results. To date there is no conclusive recommendation as to its utility in predicting antimicrobial efficacy in vivo. The serum bactericidal test may be useful in several conditions, including bacterial endocarditis, bacteremia in cancer patients, osteomyelitis, septic arthritis, monitoring combinations of antibiotics, and as a guide when changing from parenteral to oral therapy in infected patients.
On occasion neither disk diffusion nor microdilution testing reliably detects antibiotic resistance. For example, both methicillin resistance in staphylococci and vancomycin resistance in enterococci are often missed by these methods. In such cases many laboratories will use a screening plate to detect resistance. Using this method a specific concentration of the antibiotic is incorporated into a suitable agar, and a defined concentration of the organism is spotted onto the surface of the plate. The plate is incubated overnight (or for up to 48 hours in the case of methicillin-resistant staphylococci) and examined for growth. Growth in the presence of the antibiotic predicts the presence of the resistance factor.
Antibiotic pharmacodynamics and dosing regimens
As a result of integration of in vitro testing of sensitivity of organisms, in vivo measures of antibiotic efficacy, and understanding of bacterial growth and antimicrobial action, certain key principles have emerged. For β-lactam antibiotics, vancomycin, clindamycin, and macrolides, the cidal effect occurs at low multiples of the minimal inhibitory concentration (4× or 5×), and the extent of the killing depends on the duration of exposure. In animal models of infection, maximal killing of microorganisms occurs when the plasma drug concentration exceeds the minimal inhibitory concentration during 60% to 70% of the dose interval.
Fluoroquinolones and aminoglycosides demonstrate concentration-dependent killing, and here the ratio of the area under the concentration-over-time curve to the mic (AUC/minimal inhibitory concentration) correlates best with efficacy. For fluoroquinolones, concentrations in serum need to average 4 times the minimal inhibitory concentration for each 24-hour period to produce almost 100% survival in animal models of infection. To obtain a clinical response of ≥90% with aminoglycoside treatment, the peak level needs to exceed the minimal inhibitory concentration by 8- to 10-fold. This observation, plus the fact that aminoglycoside uptake by bacteria is downregulated following exposure and persists or several hours, forms the basis for once daily dosing of aminoglycosides. [Reviewing ed asks, Principle here regardinr dosing?]
Principle
Effective dosing of antibiotics depends on many factors that are drug-class dependent and in addition to the simple minimal inhibitory concentration.
Selection of Antimicrobial Agents for Testing Panels
Agents selected for inclusion in susceptibility testing panels should be chosen carefully, since results from these tests showing sensitivity encourage the practitioner to use the agents, and to assume that the antibiotic is likely to have in vivo efficacy. Suggested guidelines for selecting agents to be tested against common bacterial pathogens are listed in Table Suggested Groupings of Antimicrobial Agents That Should Be Considered for Routine Testing and Reporting by Clinical Microbiology Laboratories and a Guide for Appropriate Antibiotic Usage.
Changes in this list can be anticipated as improved and more cost-effective agents are developed. Deliberate selective reporting of the results of antibiotic susceptibility tests by the laboratory also provides a useful method to promote efficacious and cost-effective use of antimicrobials. For example, if an E. coli blood isolate is sensitive to gentamicin, there is no reason to report susceptibility to the other aminoglycosides unless the patient has a hypersensitivity reaction to gentamicin.
Reporting of the susceptibility results for the other aminoglycosides in this case might encourage physicians to prescribe a more costly aminoglycoside agent when it is not necessary. Such reasoning is particularly important for the large group of β-lactam antibiotics. Close coordination between the microbiology laboratory and hospital drug formulary committee provides a rational basis for antibiotic selection. Communication with physicians is vital to their understanding of the reasons for this policy.
Understandably, antibiotic manufacturers would prefer to see more comprehensive sensitivity reports that include their products! Physicians must also remember that reports of in vitro sensitivity tests do not guarantee that the antibiotic selected will work in vivo. The drug must reach the site of infection in concentrations adequate to reproduce the in vitro effects when coupled with the host’s defense mechanisms.
Pharmacologic Factors Affecting Antibiotic Activity
A major goal in antimicrobial therapy is to choose an agent that is selectively active for the most likely infecting microorganisms at the site of infection. Pharmacologic factors that affect antimicrobial drug efficacy include absorption of the drugs from the site of administration, delivery by the circulation to the infected region, diffusion from the plasma through tissues, penetration to the site of infection, and maintenance of adequate amounts of active drug at that site. If antibiotics only inhibit the growth of organisms rather than kill them, the host’s defense mechanisms must be sufficiently effective to eradicate the pathogenic microorganism to achieve a therapeutic success.
If this is not the case, microbicidal agents should be employed. In selected clinical syndromes (e.g., bacteremia in a neutropenic leukemic patient undergoing chemotherapy), sufficient bactericidal drug must be administered so that a cure will be produced, whereas in the vast majority of infections, antimicrobial agents are required only to augment host defenses to effect cure.
Principles
Consideration of the patient’s physiologic resilience and ability to fight infection is a key factor in choice of drug in a panoply of disease settings.
Absorption of antimicrobials
Determining the most effective route of administration to achieve adequate concentrations in the blood and tissue is important in choosing an antimicrobial (Table 14-14). Although oral administration of many antibiotics is preferred because of ease, safety, and cost, parenteral administration is usually required when treating an infection that poses a serious threat to life. Parenteral administration helps ensure that adequate concentrations of drug are achieved in the blood. Two important considerations in choosing the route of administration of a drug are the plasma concentration of drug that can be achieved by oral versus parenteral administration and the location and severity of the infection. For example, penicillin G has an oral bioavailability of only 20 to 30%.
Plasma concentrations following oral therapy may be inadequate to treat serious infections, particularly when the infections are located in tissues resistant to penetration by the antibiotics (e.g., brain or endocardium). The use of a variety of tests to measure drug concentration in plasma is appropriate when there are questions as to the adequacy of those concentrations in seriously ill patients.
Principles
In treating an infection that poses a serious threat to life, it is unwise to depend on oral absorption, especially in the presence of vomiting or gastrointestinal dysfunction. A parenteral formulation is usually indicated.
| Table Suggested Groupings of Antimicrobial Agents That Should Be Considered for Routine Testing and Reporting by Clinical Microbiology Laboratories and a Guide for Appropriate Antibiotic Usage | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Table Systematic Antimicrobial Drugs by Class and Action | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Tissue distribution of antimicrobials
The most important are those of protein and tissue binding. Biologic activity of an antimicrobial is best correlated with the concentration of free (rather than total) drug in a protein-rich medium. Extensive protein binding of an antimicrobial may not only reduce its biologic activity but also restrict its distribution into tissues, its penetration into interstitial and inflammatory spaces, and its excretion by glomerular filtration. Likewise, extensive tissue binding of drugs (e.g., the polymyxins) also may restrict distribution and penetration into sites of infection. The development of an inflammatory response at the site of bacterial infection, with an increase in blood flow and capillary permeability, presumably counteracts some of the restrictive effects of extensive protein binding. Furthermore, most drugs in clinical use can be given in dosages that are adequate to overcome their potentially “negative” binding characteristics.
| Table Classification of Antimicrobial Agents | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Table Factors Affecting Tissue Penetration of Antimicrobials | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Antimicrobial concentrations in soft tissues, joint spaces, and body fluids are usually adequate to inhibit microbial growth. However, there are some special situations in which the tissue-penetrating characteristics of drugs may be particularly important in determining clinical responses to treatment. Such situations include suppurative meningitis, bacterial endocarditis, and septic arthritis. Critical concentrations of antibiotics in plasma for the treatment of other infections have not been established, but it is usually recommended that, for treatment of bacterial meningitis, plasma concentrations exceed the minimal inhibitory concentration by 10-fold or greater. This practice ensures a margin of safety such that less-than-optimal distribution of drug to site of action [e.g., cerebrospinal fluid]can be overcome.
Pathways of excretion
Therapeutic success of an antibiotic may be partially determined by the pharmacokinetics of its excretion. This point is amply illustrated by the ability of nalidixic acid to sterilize the urinary tract despite its low concentration in plasma. Tetracyclines that do not accumulate well in the urine (e.g., minocycline or doxycycline) may be less effective in the treatment of urinary tract infection than tetracycline itself, which is predominantly excreted in the urine. When the normal renal pathway of excretion of tetracycline is impaired, therapeutic success is reduced. This is particularly true in patients with renal failure, when delivery of drugs to urine is decreased. In such patients not only is tetracycline less effective in treating urinary tract infections, but standard doses become more toxic. Similarly, in patients with biliary tract obstruction, the concentrations of antimicrobials in bile are decreased; this may be a factor in the failure of treatment.
| Table Penetration of Antimicrobial Agents into Cerebrospinal Fluid | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Table Antimicrobial Agents Excreted into Urine in Therapeutic Concentrations | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||






