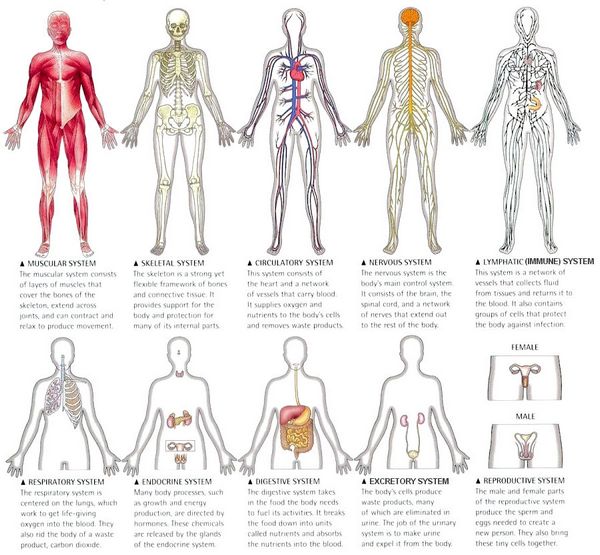
Respiratory
Bronchospasm may be a consequence of penicillin allergy. Acute severe dyspnea with cyanosis has also been observed without symptoms of bronchial obstruction or pulmonary edema. Specific mechanisms for such cases have yet to be identified.
Allergic pneumonitis and transient eosinophilic pulmonary infiltrate (Loeffler’s syndrome) are rare. These syndromes have also been observed with penicillin hypersensitivity. In one case, an alveolar allergic reaction, probably due to ampicillin, showed features of an adult respiratory distress syndrome.
Nervous system
High doses of penicillins, in the order of several million units/day of penicillin G, can produce myoclonic jerks, hyper-reflexia, seizures, or coma. Drowsiness and hallucinations can occur occasionally. Such reactions are due to a direct toxic effect and are more likely with high concentrations, as seen with intravenous administration and with cardiopulmonary bypass in open-heart surgery.
Myasthenia gravis can be aggravated by ampicillin, a reaction that is well described with aminoglycosides and some other antibiotics. Intrathecal instillation of more than 10 000 units of penicillin and the topical application of high concentrations of penicillin to the nervous system, especially the brain, during surgery have produced comparable reactions. All penicillin formulations can produce this kind of reaction. Benign intracranial hypertension is an extremely rare reaction to penicillins, possibly allergic.
Metabolism
Lipoatrophy can occur after the injection of some drugs, including penicillin.
A 2-year-old boy developed a non-tender, hypopigmen-ted, atrophic patch measuring about 2×6 cm on his right buttock. He had been well until 5 months before, when he had received an injection of penicillin into the right buttock.
The incidence of this adverse effect is unknown, as is the mechanism. In six healthy subjects, ampicillin caused an increase in urinary uric acid excretion; this effect was attributed to competition for active renal tubular reabsorption of urate.
Electrolyte balance
Potassium penicillin G can significantly alter potassium balance when given in very high doses; 20 million units of potassium penicillin G contains about 30 mmol of potassium, and in patients with renal insufficiency this amount can decisively aggravate potentially lethal hyperkalemia.
Similarly, large doses of sodium penicillin G, carbenicil-lin, or ticarcillin can cause hypernatremia. High doses of sodium penicillin can cause urinary potassium loss, presumably by acting as a non-absorbable anion in the distal tubule. Apparently by analogous mechanisms a variety of semisynthetic penicillins, including carbenicillin, cloxacillin, mezlocillin, nafcillin, piperacillin, and ticarcillin, caused hypokalemia, mainly in severely ill patients. Urinary loss of potassium and interstitial nephritis are well-recognized adverse effects of piperacillin.
Since patients in ICU may have increased risks of renal complications, serum electrolyte concentrations have been measured in 43 patients before and after piperacillin administration and in 40 patients who were given other antibiotics. The groups were comparable in regard to age and severity of disease and all had normal serum creatinine concentrations before the study. Serum concentrations of magnesium, potassium, and, to a lesser degree, calcium fell significantly 36 hours after the start of therapy in patients who were given piperacillin, but not in patients who were given other antibiotics.
The fall was most pronounced in the subgroup of patients who were also given furosemide. The authors concluded that treatment with piperacillin can cause or aggravate electrolyte disorders and tubular dysfunction in ICU patients, even when serum creatinine is normal and that the mechanism is probably exacerbation of pre-existing tubular dysfunction. Serum concentrations of electrolytes, including magnesium, should be regularly monitored and, if necessary, supplements should be given to patients in ICU who are receiving piperacillin. This may hold true for all patients receiving piperacillin.
Gastrointestinal
Antibiotic-induced colitis and diarrhea and non-specific gastrointestinal symptoms are discussed in the post on beta-lactam antibiotics.
Pancreas
The list of agents associated with pancreatitis is long and diverse and is growing. Drugs such as glucocorticoids, estrogens, diuretics, and cancer chemotherapeutic agents have all been implicated, as have various antibiotics, including tetracyclines, rifampicin, and isoniazid. Cases of pancreatitis have been reported after the administration of ampicillin and a penicillin derivative.
A 7-year-old boy developed epigastric pain, nausea, and vomiting, starting 10 days after a course of oral penicillin (dose and derivative not stated). His serum amylase activity was 1260 U/l and lipase 528 U/l; electrolytes and liver functions tests were within the reference ranges. Ultrasonography showed a normal liver, spleen, and gallbladder, but his pancreas was diffusely enlarged.
Urinary tract
Acute tubulointerstitial nephritis has been reported in relation to various penicillins, including penicillin G, ampicillin, and amoxicillin, dicloxacillin, meticillin, nafcillin, oxacillin, and piperacillin. However, meticillin is the prototype that has caused this reaction more often than any other beta-lactam. Meticillin-induced acute interstitial nephritis follows a similar pattern of dose-dependence and time-dependence to that of neutropenia.
This reaction occurred in 16% of all children treated with high-dose meticillin. Nephritis occurred after a mean of 17 days and a mean cumulative dose of 120 g. Fever and hematuria (macroscopic or microscopic) are the dominating symptoms. Rash, eosinophilia in the blood, possibly eosinophiluria, and signs of non-oliguric renal insufficiency can occur but are not always present.
Acute anuric/oliguric renal insufficiency is rare. Hemorrhagic cystitis has been observed in connection with meticillin and carbenicillin. A very high dose of amoxicillin (250 mg/kg/day for Listeria monocytogenes meningitis) combined with an aminoglycoside led to crystal-induced acute renal insufficiency after 14 days. Drug-induced nephrolithiasis, often seen during the sulfonamide era, is nowadays rare, especially in patients taking beta-lactams.
However, it can still occur with penicillins.
A 48-year-old woman with pneumococcal meningitis developed acute oliguric renal insufficiency after taking high-dose amoxicillin (320 mg/kg/day) for 4 days. Amoxicillin crystallization was documented by infrared spectrometry. The outcome was favorable after dosage reduction, a single hemodialysis, and adequate hydration. As was true for the sulfonamides, the risk of crystalluria due to penicillins is increased by high doses, a low urinary pH, and low urine output.




