Tobramycin is an aminoglycoside antibiotic.
Uses
Parenteral
Tobramycin sulfate is used parenterally for the treatment of serious infections, including septicemia, lower respiratory tract infections, CNS infections (meningitis), intraabdominal infections (including peritonitis), bone infections, skin and skin structure infections, and complicated and recurrent urinary tract infections caused by susceptible bacteria. (For information on parenteral uses of tobramycin, see Uses: Parenteral, in the Aminoglycosides General Statement 8:12.02.)
Oral Inhalation
Commercially available tobramycin solution for oral inhalation is administered via nebulization in the management of bronchopulmonary Pseudomonas aeruginosa infections in cystic fibrosis patients 6 years of age or older. Use of tobramycin oral inhalation solution can be considered for suppressive therapy in cystic fibrosis patients colonized with Ps. aeruginosa if they are 6 years of age or older and have a forced expiratory volume in 1 second (FEV1) that is 25-75% of the predicted value.
Safety and efficacy of the solution for oral inhalation have not been established in pediatric patients younger than 6 years of age, in patients with FEV1 less than 25% or exceeding 75% of the predicted value, or in patients colonized with Burkholderia cepacia (formerly Ps. cepacia).
Results of randomized, double-blind, placebo-controlled studies in cystic fibrosis patients 6 years of age or older with Ps. aeruginosa indicate that tobramycin solution for oral inhalation given in conjunction with standard therapy for cystic fibrosis can improve lung function, decrease the density of P. aeruginosa in expectorated sputum, and reduce the need for hospitalization and parenteral therapy with antipseudomonal anti-infectives.
At baseline, the FEV1 in all study patients was 25-75% of the predicted value. Patients were randomized to receive 3 cycles of tobramycin solution for oral inhalation (300 mg twice daily given using a hand-held reusable nebulizer [PARI LC PLUS®] connected to a Pulmo-Aide® compressor) or placebo (sodium chloride solution flavored with 1.25 mg of quinine sulfate to mimic the taste of the active treatment); each cycle consisted of 28 days of administration of drug or placebo followed by 28 days without administration of drug or placebo.
Besides tobramycin solution for oral inhalation or placebo, patients received standard therapy recommended for patients with cystic fibrosis, such as oral and parenteral anti-infectives active against Pseudomonas, b2-adrenergic agonists, cromolyn sodium, orally inhaled corticosteroids, and techniques for clearance of the airway; about 77% of patients also received concurrent therapy with dornase alfa. Tobramycin solution for inhalation was superior to placebo based on the primary end point of lung function at 20 weeks (at the end of the third cycle), measured as FEV1 and expressed as the percentage of the predicted value. At 20 weeks, the change in lung function in patients who received the drug was an average 10% increase in FEV1 over baseline compared with an average 2% decrease in FEV1 in those who received placebo.
Tobramycin solution for oral inhalation also was superior to placebo based on the primary end point of the density of P. aeruginosa in sputum at 20 weeks, calculated as the log value for the sum of colony forming units (CFUs) per g of sputum.
At 20 weeks, there was an average decrease of 0.8 log CFU per g of sputum from baseline in patients who received the drug compared with an average increase of 0.3 log CFU per g of sputum in those who received placebo. The greatest reductions in the density of P. aeruginosa in sputum in patients who received the drug were observed during the first 2 cycles of administration.
At 4 weeks (after the initial 28-day treatment regimen), there was an average reduction of 1.9 log CFU per g of sputum in patients treated with the drug; at 12 weeks (after the second 28-day treatment regimen), there was an average reduction of 1.8 log CFU per g of sputum in those treated with the drug.
During the periods when patients were alternated off of administration of tobramycin solution for oral inhalation, the density of P. aeruginosa in sputum in patients treated with the drug approached values calculated at the start of the first cycle of administration of the drug.
The average duration of hospitalization was 5.1 days in patients who received tobramycin solution for oral inhalation and 8.1 days in those who received placebo. Parenteral anti-infectives active against Pseudomonas were administered for an average of 9.6 days in patients who received tobramycin solution for oral inhalation and 14. days in patients who received placebo.
One or more courses of parenteral anti-infectives active against Pseudomonas were administered to 39% of patients who received tobramycin solution for oral inhalation and 52% of patients who received placebo. In vitro susceptibility testing of Ps. aeruginosa isolates obtained from patients in these clinical studies indicates that susceptibility of most isolates was not adversely affected by 3 treatment cycles of tobramycin oral inhalation therapy. However, Ps. aeruginosa isolates with increased tobramycin MICs were reported in some patients who received the drug. The relationship between clinical outcome and in vitro susceptibility of Ps. aeruginosa to tobramycin is unclear. There was no evidence of improvement in FEV1 or reduction in the bacterial density in sputum in a limited number of patients who had clinical isolates of P. aeruginosa that were resistant to tobramycin (MICs of 128 mcg/mL or greater) at study entry.
Administration
Reconstitution and Administration
Tobramycin sulfate is administered by IM injection or IV infusion. Commercially available tobramycin solution for oral inhalation is administered via nebulization.
Parenteral
Parenteral preparations of tobramycin sulfate should be inspected visually for particulate matter and discoloration before use. Commercially available tobramycin sulfate injections should not be used if they are discolored.
IM Injection
For IM injection, the appropriate dose should be withdrawn from multiple-dose vials of tobramycin sulfate or should be injected directly using a commercially available prefilled syringe. Solutions prepared from or commercially available in pharmacy bulk packages, those available in ADD-Vantage® vials, or the commercially available injections in 0.9% sodium chloride should not be used for IM administration of the drug.
IV Infusion
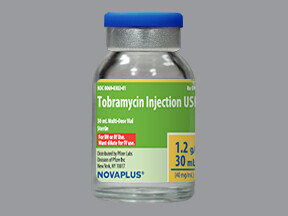
Tobramycin sulfate sterile powder is reconstituted by adding 30 mL of sterile or bacteriostatic water for injection to a vial labeled as containing 1.2 g of tobramycin (pharmacy bulk package). The resultant solution contains 40 mg of tobramycin per mL.
The commercially available pharmacy bulk package injection of tobramycin sulfate or reconstituted solutions prepared from the pharmacy bulk package sterile powder are not intended for direct IV infusion; the appropriate dose must be withdrawn and diluted in sufficient volume of a compatible IV infusion solution prior to administration.
Likewise, the manufacturer recommends that the appropriate dose from other multiple-dose vials of the drug be diluted prior to IV administration. ADD-Vantage® vials of tobramycin sulfate should be diluted according to the manufacturer’s directions prior to IV infusion.
For adults, IV infusions are prepared by diluting the calculated dose of tobramycin with 50-100 mL of a compatible IV infusion solution. The diluted solution usually should be infused over 20-60 minutes.
The manufacturer states that infusion periods of less than 20 minutes should not be used because they may give peak serum concentrations exceeding 12 mcg/mL. For pediatric patients, the volume of infusion solution depends on the patient’s needs, but should be sufficient to allow an infusion period of 20-60 minutes. Diluted solutions prepared from ADD-Vantage® vials of the drug should be administered only by IV infusion. Tobramycin sulfate that is commercially available as diluted solutions (0.8, 1.2, or 1.6 mg of tobramycin per mL) in 0.9% sodium chloride should only be administered by IV infusion.
Additives should not be introduced into the injection container, and the injection should not be used in series connections. However, if needed, additional tobramycin sulfate injection may be introduced into the injection container. The manufacturer’s instructions should be consulted for proper use of the commercially available injections of tobramycin sulfate in 0.9% sodium chloride.
Oral Inhalation
Commercially available tobramycin solution for oral inhalation is administered via nebulization. The oral inhalation solution should not be administered IV, subcutaneously, or intrathecally. Tobramycin solution for oral inhalation should be administered using a PARI LC PLUS® nebulizer (a hand-held, reusable nebulizer) connected to a DeVilbiss Pulmo-Aide® compressor.
Prior to administration of tobramycin solution for oral inhalation, the manufacturers’ information should be reviewed to ensure thorough familiarity with the use and maintenance of the nebulizer and compressor. Tobramycin solution for oral inhalation should be administered while the patient is sitting or standing upright and breathing normally through the mouthpiece of the nebulizer. Patients may find that breathing through the mouth may be aided by using nose clips.
A nebulizer treatment period of about 15 minutes usually is required to completely administer the usual dose of tobramycin solution for oral inhalation. Tobramycin solution for oral inhalation should not be diluted prior to administration and should not be admixed with other drugs (e.g., dornase alfa) in the nebulizer. Patients usually receive tobramycin solution for oral inhalation in conjunction with various other standard therapies recommended for patients with cystic fibrosis.
The manufacturer and some clinicians recommend that patients should receive other therapies prior to doses of tobramycin solution for oral inhalation.
Based on protocols used in clinical studies evaluating tobramycin solution for oral inhalation, it has been recommended that patients receive doses of inhaled bronchodilators first, then dornase alfa administered by oral inhalation, then chest physiotherapy, then tobramycin solution administered by oral inhalation. If orally inhaled corticosteroids, cromolyn sodium, or nedocromil sodium also are indicted in the patient, these drugs should be administered following the dose of tobramycin solution for oral inhalation.
Dosage
Parenteral Dosage
Dosage of tobramycin sulfate is expressed in terms of tobramycin and is identical for IM or IV administration. Parenteral dosage should be based on an estimate of ideal body weight. The usual dosage of tobramycin recommended by the manufacturer for adults, children, and infants older than 1 week of age with normal renal function is 3 mg/kg daily given in equally divided doses at 8-hour intervals.
The manufacturer states that in life-threatening infections, up to 5 mg/kg may be administered daily in 3 or 4 equally divided doses; dosage should be reduced to 3 mg/kg daily as soon as clinically indicated.
The manufacturer states that dosage in neonates 1 week of age or younger should not exceed 4 mg/kg daily given in equally divided doses at 12-hour intervals. However, some clinicians recommend 5-7. mg/kg daily given in equally divided doses at 12-hour intervals in neonates. Alternatively, many clinicians recommend that tobramycin dosage be determined using appropriate pharmacokinetic methods for calculating dosage requirements and patient-specific pharmacokinetic parameters (e.g., elimination rate constant, volume of distribution) derived from serum concentration-time data; in determining dosage, the susceptibility of the causative organism, the severity of infection, and the patient’s immune and clinical status also must be considered.
Current evidence suggests that once-daily administration of aminoglycosides is at least as effective as, and may be less toxic than, conventional dosage regimens employing multiple daily doses of the drugs; however, additional controlled trials in children, patients with renal dysfunction, and other appropriate patient groups are needed to fully define optimal use of once-daily aminoglycoside dosing regimens. (See Dosage and Administration: Dosage, in the Aminoglycosides General Statement 8:12.02.)
Whenever possible, and especially in patients with life-threatening infections, suspected toxicity or nonresponse to treatment, decreased or varying renal function, and/or when increased aminoglycoside clearance (e.g., patients with cystic fibrosis, burns) or prolonged therapy is likely, peak and trough serum concentrations of tobramycin should be determined periodically and dosage should be adjusted to maintain desired serum concentrations.
A causal relationship between maintenance of certain peak or trough serum concentrations or other pharmacodynamic endpoints and clinical response or toxicity has not been established to date for aminoglycoside dosing regimens.
However, in general, desirable peak serum concentrations of tobramycin are 4-12 mcg/mL, and trough concentrations of the drug should not exceed 1-2 mcg/mL. Some evidence suggests that an increased risk of toxicity may be associated with prolonged peak tobramycin serum concentrations greater than 10-12 mcg/mL and/or trough concentrations greater than 2 mcg/mL. In conjunction with IM or IV administration of the drug, tobramycin doses of 3-8 mg have been administered intrathecally or intraventricularly every 18-48 hours in adults.
Oral Inhalation Dosage
Dosage of commercially available tobramycin solution for oral inhalation is the same for all patients regardless of age or body weight. The drug is given in an intermittent dosage regimen that involves alternating 28-day periods when the drug is given with 28-day periods when the drug is not given.
The dosage of tobramycin solution for oral inhalation recommended for adults and children 6 years of age or older is 300 mg twice daily for 28 days. Doses should be administered using the recommended nebulizer system every 12 hours (or at intervals as close to every 12 hours as possible); doses should not be administered at intervals less than 6 hours. Each 28-day regimen of tobramycin solution for oral inhalation should be followed by a 28-day period when the drug is not administered.
Dosage in Renal Impairment
In patients with impaired renal function, doses and/or frequency of administration of tobramycin must be modified in response to serum concentrations of the drug and the degree of renal impairment.
There are various methods to determine dosage and a wide variation in dosage recommendations for these patients. However, even when one of these methods is used, peak and trough serum concentrations of the drug should be monitored, especially in patients with changing renal function. The manufacturers recommend an initial loading dose of 1 mg/kg.
For subsequent therapy, the manufacturers state that 1-mg/kg doses can be given at intervals (in hours) calculated by multiplying the patient’s steady-state serum creatinine (in mg/dL) by 6.
Alternatively, many clinicians recommend the dosing method of Sarubbi and Hull, which is based on corrected creatinine clearance. (See Dosage and Administration: Dosage in Renal Impairment, in the Aminoglycosides General Statement 8:12.02.)
These dosage calculation methods should not be used in patients undergoing hemodialysis or peritoneal dialysis. In adults with renal failure undergoing hemodialysis, some clinicians recommend supplemental doses of 50-75% of the initial loading dose at the end of each dialysis period. However, serum concentrations of the drug should be monitored in dialysis patients and dosage should be adjusted to maintain desired serum concentrations.
Pharmacokinetics
The pharmacokinetics of tobramycin are similar to those of the other aminoglycosides. In all studies described in the Pharmacokinetics section, tobramycin was administered parenterally as the sulfate salt; dosages and concentrations of the drug are expressed in terms of tobramycin.
Absorption
Following IM administration of a single dose of tobramycin of 1 mg/kg in adults with normal renal function, peak plasma tobramycin concentrations averaging 4-6 mcg/mL are attained within 30-90 minutes; plasma concentrations of the drug are 1 mcg/mL or less at 8 hours.
When the same dose is administered by IV infusion over 30-60 minutes, similar plasma concentrations of the drug are attained. In one study in neonates, average peak plasma tobramycin concentrations of about 5 mcg/mL were attained 30-60 minutes after a single IM dose of 2 mg/kg; plasma concentrations averaged 1-2 mcg/mL at 12 hours. In one adult with meningitis, intrathecal administration of 3-8 mg of tobramycin every 48 hours in conjunction with IM administration of 3 mg/kg daily resulted in CSF concentrations of the drug averaging 15-46 mcg/mL during the first 24 hours and 3-9 mcg/mL at 48 hours.
Bioavailability of tobramycin administered by oral inhalation via a nebulizer may be variable because of individual differences in nebulizer performance and airway pathology. Following oral inhalation via nebulization, tobramycin remains concentrated principally in the airways; the drug does not readily cross epithelial membranes.
Tobramycin sputum concentrations are highly variable following oral inhalation, but the drug does not appear to accumulate in sputum following multiple doses. Following an initial 300-mg dose of commercially available tobramycin solution for oral inhalation given via a nebulizer, sputum concentrations of the drug at 10 minutes averaged 1237 mcg/g (range: 35-7414 mcg/g).
After 20 weeks of intermittent therapy (300-mg twice daily for 28 days followed by 28 days without the drug), sputum concentrations 10 minutes after administration averaged 1154 mcg/g (range: 39-8085 mcg/g) and sputum concentrations 2 hours after administration were approximately 14% of those obtained 10 minutes after administration. Following a single 300-mg dose of the commercially available tobramycin solution for oral inhalation given via nebulization in patients with cystic fibrosis, serum tobramycin concentrations averaged 0.95 mcg/mL at 1 hour after administration; after 20 weeks of intermittent therapy (300 mg twice daily for 28 days followed by 28 days without the drug), serum tobramycin concentrations averaged 1.05 mcg/mL at 1 hour after administration.
Elimination
The plasma elimination half-life of tobramycin following parenteral administration is usually 2-3 hours in adults with normal renal function and is reported to range from 5-70 hours in adults with impaired renal function.
The plasma elimination half-life of tobramycin is reported to average 4.6 hours in full-term infants and 8.7 hours in low birth-weight infants. In adults with normal renal function, up to 84% of a single 1 mg/kg IM dose of tobramycin is excreted unchanged by glomerular filtration within 8 hours and up to 93% is excreted unchanged within 24 hours. Peak urine concentrations of tobramycin may range from 75-100 mcg/mL following a single IM dose of 1 mg/kg in adults with normal renal function.
Complete recovery of the dose in urine requires approximately 10-20 days in patients with normal renal function, and terminal elimination half-lives of greater than 100 hours have been reported in adults with normal renal function following repeated IM or IV administration of the drug. When tobramycin is administered by oral inhalation using a nebulizer, any drug that is not absorbed systemically probably is eliminated principally in expectorated sputum.
Chemistry and Stability
Chemistry
Tobramycin is an aminoglycoside antibiotic obtained from cultures of Streptomyces tenebrarius. Tobramycin occurs as a white to off-white, hygroscopic powder and is freely soluble in water and very slightly soluble in alcohol.
The drug is commercially available as the sulfate salt for parenteral administration and as the base for administration by oral inhalation via a nebulizer. The commercially available sterile powder is formulated with sulfuric acid or sodium hydroxide to adjust the pH.
When reconstituted as directed, solutions prepared from the sterile powder have a pH of 6-8. Commercially available tobramycin sulfate and tobramycin sulfate in 0.9% sodium chloride injections are clear, colorless, sterile, and aqueous solutions; sulfuric acid or sodium hydroxide is added during the manufacture of the injections to adjust the pH to 3-6.
Commercially available injections of tobramycin sulfate in 0.9% sodium chloride have an osmolarity of approximately 316 mOsm/L and contain about 15. mEq of sodium per 100 mL of the solution. Commercially available tobramycin solution for oral inhalation occurs as a clear, slightly yellow, aqueous solution. Each 5-mL single-use ampul containing 300 mg of tobramycin contains 11. mg of sodium chloride in sterile water for injection; sulfuric acid and sodium hydroxide are added during the manufacture of the solution to adjust the pH to 6.241
The solution for oral inhalation does not contain preservatives.
Stability
Tobramycin sulfate powder for injection and commercially available tobramycin sulfate injections should be stored at 15-30°C. The injections should not be used if they are discolored. Commercially available injections of tobramycin sulfate in 0.9% sodium chloride should be stored at 25°C; freezing should be avoided. Although brief exposure to temperatures up to 40°C does not adversely affect these solutions, exposure to excessive heat should be avoided.
Following reconstitution of the sterile powder with sterile water for injection, tobramycin solutions containing 40 mg/mL are stable for 24 hours at room temperature or 96 hours at 2-8°C. Extemporaneously prepared reconstituted solutions containing 40 mg/mL may be frozen immediately after reconstitution in their original containers and are stable for up to 12 weeks when stored at -10 to -20°C. Once thawed, solutions should not be refrozen.
Tobramycin sulfate is stable for 24 hours at room temperature in most IV infusion solutions; however, the drug is incompatible with IV solutions containing alcohol. Once ADD-Vantage® vials have been connected to an appropriate diluent container and activated for dilution, resultant solutions should be used within 24 hours.
Commercially available injections of tobramycin sulfate in 0.9% sodium chloride are provided in flexible plastic (LifeCare®) containers and are stable for 18 months following the date of manufacture when stored as directed. Additives should not be introduced into the injection containers of the commercially available diluted solutions of the drug; however, if needed, additional tobramycin sulfate injection may be introduced into the injection containers. Unused portions of commercially available injections of tobramycin sulfate in 0.9% sodium chloride should be discarded.
The manufacturers state that tobramycin sulfate solutions should not be mixed with other drugs. Commercially available tobramycin solution for oral inhalation should be stored at 2-8°C. If refrigeration is not available, intact or opened foil pouches containing ampuls of the solution for oral inhalation may be stored at room temperature up to 25°C for up to 28 days.
The ampuls should not be exposed to intense light. Tobramycin solution for oral inhalation may darken if stored at room temperature, but this does not indicate a change in the quality of the preparation.
Any tobramycin solution for oral inhalation that is cloudy or has visible particles should be discarded. In addition, any tobramycin solution for oral inhalation that has been stored at 2-8°C beyond the expiration date stamped on the ampul or stored for longer than 28 days at room temperature should be discarded. For further information on chemistry and stability, mechanism of action, spectrum, resistance, pharmacokinetics, uses, cautions, drug interactions, and dosage and administration of tobramycin, see the Aminoglycosides General Statement 8:12.02.
Preparations
Tobramycin Oral Inhalation Solution, for 300 mg per 5 mL Tobi®, (preservative-free; nebulization available as polyethylene ampuls) Chiron Tobramycin Sulfate Parenteral For injection, for 1.2 g (of tobramycin) Nebcin®, IV infusion pharmacy bulk package Lilly Injection 10 mg (of tobramycin) per mL Nebcin® Pediatric, (with (20 mg) edetate disodium, phenol, and sodium bisulfite) Lilly Tobramycin Sulfate Injection, Abbott 40 mg (of tobramycin) per mL Nebcin®, (with edetate (60 or 80 mg) disodium, phenol, and sodium bisulfite) Lilly Tobramycin Sulfate Injection, Abbott Sandoz GensiaSicor 40 mg (of tobramycin) per mL Nebcin®, (with edetate (1. or 2 g) pharmacy bulk disodium, phenol, and sodium package bisulfite) Lilly Tobramycin Sulfate Injection, Abbott Sandoz GensiaSicor Injection, for IV 10 mg (of tobramycin) per mL Tobramycin Sulfate ADD- infusion (60 or 80 mg) Vantage®, (with sodium metabisulfite) Abbott Tobramycin Sulfate in Sodium Chloride Parenteral Injection, for IV 0.8 mg (of tobramycin) per Tobramycin Sulfate in 0.9% infusion only mL (80 mg) in 0.9% Sodium Sodium Chloride Injection, Chloride (LifeCare®) Abbott 1.2 mg (of tobramycin) per Tobramycin Sulfate in 0.9% mL (60 mg) in 0.9% Sodium Sodium Chloride Injection, Chloride (LifeCare®) Abbott 1.6 mg (of tobramycin) per Tobramycin Sulfate in 0.9% mL (80 mg) in 0.9% Sodium Sodium Chloride Injection, Chloride (LifeCare®) Abbott

